To analyze the relationship between high-fidelity clinical simulation and levels of anxiety, stress and self-perceived competence in masters level nursing students.
MethodsWe conducted a quasi-experimental pre–post study from June 2021 to December 2022 at the Faculty of Nursing. 190 Masters students took part in the study. Students were alphabetically divided into four sections of about 20 students and these sections were in turn divided into subgroups of three to four people. Seven clinical scenarios were designed, coinciding with frequent problems in critically ill children and each group of students was assigned one of them. Before and after resolving clinical scenarios students assessed their level of anxiety using the State-Trait Anxiety Inventory (STAI), the Self-Confidence in Learning Scale (SCLS), stress and the Nursing Student Satisfaction.
ResultsThe overall median score for anxiety was 8 (5–10) pre-CS versus 5 (3–7) post-CS, with a statistically significant relationship (p<0.001). As for stress, we observed scores of 3.0 (2–4) points pre-CS vs. 2.0 (1–3) post-CS, also with statistical significance (p<0.001). An overall self-confidence in learning score of 25.0 (22–28) points was obtained. Previous experience in CS was independently related to a lower level of stress after performing the CS, and the older the age, the higher the level of self-confidence in learning.
ConclusionWhen designing scenarios that focus on the attention of critically ill pediatric patients, professionals should consider the relevant sociodemographic and professional variables in order to reduce anxiety and stress.
Analizar la relación entre la simulación clínica de alta fidelidad y el grado de ansiedad, estrés y autopercepción competencial en los estudiantes de máster de enfermería.
MétodosEstudio cuasi-experimental pre-post desde junio de 2021 hasta diciembre de 2022 en una facultad de enfermería. Participaron en el estudio 190 estudiantes de máster. Los estudiantes se dividieron alfabéticamente en 4 grupos de 20 estudiantes, y éstos en subgrupos de 3 a 4 personas. Se diseñaron 7 escenarios clínicos que coincidían con problemas frecuentes en niños/as críticamente enfermos/as y a cada grupo de estudiantes se le asignó uno de ellos. Antes y después de resolver los escenarios clínicos los/las estudiantes evaluaron su nivel de ansiedad, mediante la escala de ansiedad estado-rasgo (STAI), su autopercepción competencial, cumplimentando la Nursing Student Satisfaction and Self-Confidence in Learning Scale (SCLS), su estrés y su grado de satisfacción.
ResultadosLa puntuación mediana global para la ansiedad fue de 8,0 (5-10) puntos pre-SC frente a 5,0 (3-7) puntos post-SC, con una relación estadísticamente significativa (p<0,001). En cuanto al estrés, se observaron puntuaciones de 3,0 (2-4) puntos pre-SC frente a 2,0 (1-3) post-SC, también con significación estadística (p<0,001). Se obtuvo una puntuación global de autoconfianza en el aprendizaje de 25,0 (22-28) puntos. La experiencia previa en SC se relacionó de forma independiente con un menor nivel de estrés tras realizar el SC, y a mayor edad, mayor nivel de autopercepción competencial.
ConclusionesEn el diseño de escenarios centrados en el manejo del paciente crítico pediátrico, los profesionales deben considerar las variables sociodemográficas y profesionales relevantes para reducir la ansiedad y el estrés.
Clinical simulation is an appropriate educational strategy in nursing, especially at the undergraduate level, for pediatric and midwifery residents, and for newly registered nurses.
What it contributesThis is one of the studies focusing on postgraduate nursing students who have direct contact with pediatric patients in clinical practice. Although participants showed anxiety and stress before CS, this decreased after CS. At the same time, we found moderate levels of satisfaction and confidence in learning. We also observed that variables such as age and clinical simulation experience can influence the perception and effectiveness of clinical simulation.
Implications for clinical practiceParticipants reported anxiety and stress prior to clinical simulation. Faculties and pediatric intensive care units should continue to use clinical simulation, but particularly consider age and experience when designing it, as there are variables that affect anxiety and stress. Therefore, in addition to the purpose of the simulation, the simulation should be adapted to different profiles of participants and pediatric patients.
Previous studies show that theoretical-practical training programs are necessary for new nurses who are starting their careers or undertaking graduate studies.1,2 Transition programs have demonstrated an increase in self-confidence and self-perception and an improvement in nurses’ knowledge and competencies in some activities and procedures. The design of these educational programs is varied, although all consist of theoretical classroom teaching and guided clinical experience.2,3
Providing comprehensive care for pediatric patients can be challenging due to the presence of multiple co-occurring health problems, which necessitate complex treatment strategies.4,5 In terms of training methods that can improve care for these patients, research suggests that simulation is a more effective training method than traditional theoretical approaches.4,6,7 Thus, the World Health Organization (WHO) suggests the use of clinical simulation (CS) in training programs to promote patient safety8 and recognizes it as an important method in nursing, since training is essential to increasing the quality of care and patient safety.9
Therefore, although CS does not replace supervised learning in the clinical units of healthcare centers, it emerges as an effective methodological tool, which allows inexperienced staff to acquire knowledge and practice technical and non-technical skills without any risk to patients10 and in a clinical environment similar to that of a health center.11
The attention and care of pediatric patients is one of the most challenging tasks because they usually have multiple pathological problems simultaneously, which requires complex treatment strategies. Furthermore, the progression of these patients is often characterized by considerable variability, with their clinical status fluctuating rapidly, making timely interventions crucial for devising prognoses and mitigating the development of associated morbidities.4 In the specific case of the pediatric critically ill patient, this is much more complex as they suffer from pathological problems so severe that they are potentially or actually life threatening. For this reason, their clinical management requires complex strategies and treatments offered in the pediatric intensive care unit (PICU). In addition, their pathophysiological evolution is characterized by a high degree of variability and their clinical condition can change rapidly, making the timing of interventions essential to improve prognosis and prevent the development of morbidities4,12 To ensure the safe clinical care of these patients, it is essential to manage the risks appropriately and try to minimize the number of errors and adverse effects that can occur. To this end, one of the key aspects is the implementation of training interventions for PICU staff, and the effectiveness of clinical simulation (CS) compared to traditional learning methods has been demonstrated.12,13
The incorporation of simulation in professional education programs helps health professionals improve their knowledge, skills, and competencies in evaluating and managing clinical situations6 and simulate caring for different patient types.14 Furthermore, it allows inexperienced professionals to practice without placing patients at risk.6,15
While the benefits of simulation are clear, a drawback is that CS can generate higher levels of anxiety and stress in students than other educational approaches.16 Notably these mental states are often linked.17,18
Several authors have pointed out the benefits of CS as an educational strategy in nursing, especially at the undergraduate level,11,19–22 among residents in pediatrics and midwifery,23 and among newly registered nurses.14 Moreover, several point out that CS is associated with anxiety and stress in students.16–18 However, we have not found studies that examine the relationship between students’ anxiety, stress, self-confidence in learning and/or sociodemographic and professional variables. Therefore, we describe students’ experiences of anxiety and stress surrounding CS as well as their perception of how CS impacts their learning, in order to guide the design of CS and the implementation of activities prior to CS that can reduce students’ negative experiences and ensure adequate learning.
The general objective of the research was to analyze the relationship between high-fidelity CS and levels of anxiety, stress and self-perceived competence in masters level nursing students. The specific objectives are as follows: (a) to describe the level of anxiety and stress in a group of graduate nursing students before and after carrying out a pediatric CS activity, (b) to determine their perception of their own learning after having performed pediatric CS, (c) to analyze the relationship of the level of anxiety, stress, and self-confidence in learning with the various sociodemographic and professional variables, (d) to determine their degree of satisfaction with the CS.
MethodsStudy designWe conducted a quasi-experimental pre–post study from June 2021 to December 2022 at the Faculty of Nursing of the University of Barcelona.
ParticipantsBy means of non-probabilistic intentional sampling, all students of the Master's in Pediatric Nursing (201 students) and Master's in Critical Care Nursing (96 students) of the Faculty of Nursing of the University of Barcelona who met the selection criteria were included. All of the students were working as nurses in a hospital in the area. The following were established as inclusion criteria: verbal acceptance, signing of informed consent document, and having attended the entire pediatric CS activity. The following exclusion criteria were established: nursing students undertaking their practicum and health professionals without a degree in nursing. Finally, the following were established as withdrawal criteria: request by the participant to be withdrawn from the study without academic or perceived academic penalty.
VariablesThe following variables were recorded for each participant: Sociodemographic and professional variables (age, sex, nursing experience, pediatric nursing experience, previous experience in CS, and current work unit), anxiety using the State-Trait Anxiety Inventory (STAI),21 self-confidence in learning,22,23 personal stress,24 and overall satisfaction.
Data collection toolsState-Trait Anxiety Inventory (STAI)We used the short STAI validated in Spanish by Guillén-Riquelme in 2013 for use with students, which is composed of six items. Items 1, 3 and 4 refer to the absence of anxiety and therefore are reverse-scored. Participants rated statements related to their current state of anxiety on a 4-point Likert scale from 0 (not at all) to 3 (very much so). High scores on the scale indicate high levels of anxiety. Appropriate validity and reliability were obtained, and Cronbach's alpha was 0.82.24
Nursing Student Satisfaction and Self-Confidence in Learning Scale (SCLS)To measure students’ perception of their own learning, we used the adaptation of the SCLS in a population of Spanish master's degree students carried out by Perpignan-Galvañ in 2018–201925 and later used by Farrés with 489 undergraduate students in nursing.26 Self-confidence and self-awareness are inextricably linked in the learning process, as the way we see ourselves directly influences our willingness to face new challenges. When a person has high self-confidence, he/she tends to perceive him/herself as capable and competent, which motivates him/her to actively participate in the learning process. On the other hand, a negative self-perception can lead to doubt and fear of failure, which can limit participation and effort in the learning process. For this reason, since no instrument has been found that directly measures competence self-perception, and since the items included in the SCLS could be useful in assessing it and establishing the relationship between high/low self-confidence and competence self-perception, this scale was used in the present study.
The SCLS is composed of 13 items grouped into two dimensions: satisfaction with current learning (five items related to the CS) and self-confidence with learning (eight items that measure students’ confidence about skills and knowledge in the resolution of the clinical case in the CS). We used only the self-confidence with learning subscale. Students rated their learning on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). The lowest and highest scores for the self-confidence subscale are 8 and 40, respectively. High scores indicate greater self-confidence with learning related to the CS. The scale has shown good internal consistency, obtaining, in the study of Perpignan-Galvañ et al. a Cronbach's Alpha greater than 0.92 for the total scale (0.94 for the satisfaction subscale and 0.87 for the self-confidence subscale) and, in the case of the research by Farrés et al., 0.88 (from 0.83 to 0.81) in each of the dimensions.
Perceived personal stress scaleBecause there is no validated scale for measuring students’ stress when facing a CS, we designed a 5-point Likert scale from 1 (no stress) to 5 (a lot of stress). We based the scale on one used in a study with a sample of 107 nursing students in which stress was assessed before and after a simulation intervention.27
Overall satisfaction surveyBecause the satisfaction portion of the SCLS does not cover all aspects of satisfaction that were of interest to us, we designed an ad hoc satisfaction survey, which was administered after the CS. It evaluated the usefulness of the SC, the materials included in the scenario, the didactics and the correlation between theory and practice. The survey used a 5-point Likert scale from 1 (not at all satisfied) to 5 (very satisfied). In creating the survey, we kept in mind the learning objectives of the CS and drew on the satisfaction portion of the SCLS. The entire CS teaching team met to discuss and approve the survey (Supplementary file 1).
Data collection procedureSeven clinical scenarios were designed, coinciding with frequent problems in critically ill children (bronchiolitis, sepsis, meningitis, traumatic brain injury, febrile seizure, dehydration, and comprehensive care for premature patients) and each group of students was assigned one of them. Using a consensus technique, these scenarios were validated by 5 pediatric nursing experts, two of whom were SC instructors accredited by Boston and Sant Joan de Déu Hospital. Students had to perform a physical assessment, conduct monitoring and clinical management related to identifying the health problem, and perform nursing care and other actions. In addition, transversal competences such as teamwork and leadership were considered. Each group of master's students was alphabetically divided into four sections of about 20 students and these sections were in turn divided into subgroups of three to four people.
Prior to the activity, the instructions were explained in the students’ regular classroom, and both the CS classroom and the resources available to solve the case were shown to the students. Once students’ questions were answered, oral and written informed consent was obtained, and participants filled out the pre-CS questionnaire related to sociodemographic and professional variables, anxiety, and stress. Then, each subgroup entered the CS room where two or three teachers (two of them accredited instructors) guided the clinical case, taking on different roles depending on the clinical situation (family member, doctor, and facilitator). The facilitator established the clinical progression of the patient and improved or worsened their condition depending on the actions carried out by the students. The rest of the students were in a continuous room watching how the case was being solved. Once each CS case was completed, a debriefing of key aspects of each case was carried out jointly with the whole group. After addressing the questions that arose, participants completed the post-CS questionnaires (anxiety, stress, self-confidence in learning, overall satisfaction). The time allocated to each phase of the intervention with CS was as follows:
- 1.
Presentation of the activity, CS classroom, necessary resources, informed consent, and completion of the pre-CS questionnaires: 15min.
- 2.
Carrying out the CS: 15min.
- 3.
Debriefing and completion of post-CS questionnaires: 30min.
Qualitative variables were described with absolute frequencies and percentages. Quantitative variables were described using mean, standard deviation, median and interquartile range. The Kolmogorov–Smirnov test was used to assess the normality of distributions.
The sociodemographic and professional characteristics were analyzed according to the main outcomes (anxiety, stress, self-confidence in learning, and overall satisfaction after CS). In the case of quantitative variables, Student's t-tests were carried out (Mann–Whitney U-tests for non-normal distributions). Linear relationships were analyzed using the Pearson correlation coefficient.
Backward stepwise linear regression models or analysis of covariance (ANCOVA models) were performed in order to identify variables related to (1) anxiety and stress before CS, (2) changes in anxiety and stress pre- and post-test, and (3) self-confidence in learning after CS. Variables with a p-value<0.2 in the univariate analysis were included as independent variables. The results were described with beta coefficients (β), 95% confidence interval (CI) and p-values.
For all the tests, p-values<0.05 were considered statistically significant. The statistical package R Studio (V2.5.1) was used for the analysis.
Ethical considerationsPermission was granted from the administration and two department heads of the Faculty of Nursing. We followed the Belmont Report's (1978) principles of respect for persons, beneficence, and justice. To this end, oral and written informed consent was obtained from all participants. We protected participants’ data in accordance with the General Data Protection Regulation of the European Union 2016/679, applicable in Spain since May 2018, as well as Law 41/2002 Regulating Patient Autonomy and Rights and Obligations Regarding Clinical Information and Documentation. Participants answered the questionnaires anonymously. Participation was voluntary and students were informed that their course grades would not be affected by their decisions about participation.
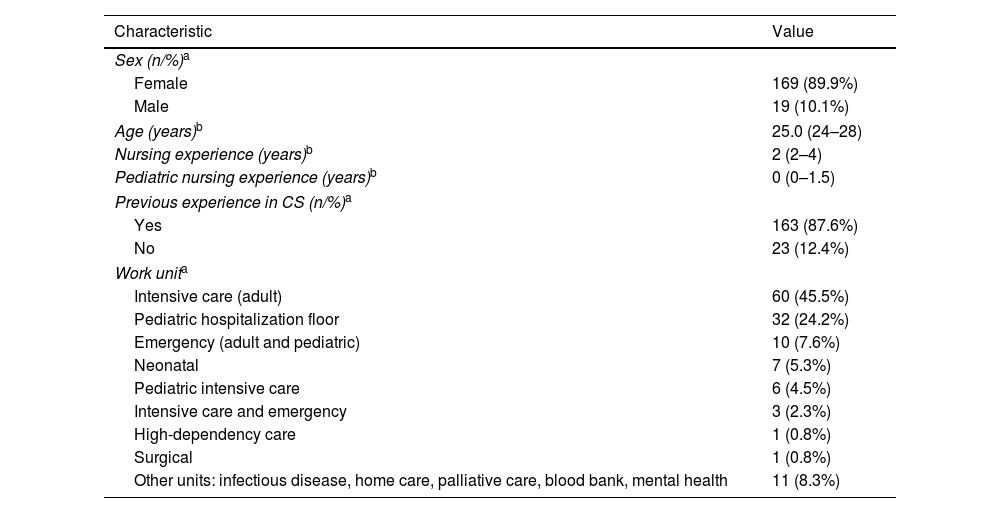
ResultsSociodemographic and professional characteristics of the sampleOf a total of 201 students who met the selection criteria, 190 participated in the study, of which 89.9% (n=169) were female. The median age was 25.0 (24–28) years. The median nursing experience was 2 years (2–4), and the median pediatric nursing experience was 0 (0–1.5) years. Of the total sample, 45.5% (n=60) worked in adult intensive care units, followed by 24.2% (n=32) who worked on pediatric hospitalization floors. Additionally, 87.4% (n=163) stated that they had previously performed other CS activities (Table 1).
Sociodemographic and professional characteristics of the sample (n=190).
| Characteristic | Value |
|---|---|
| Sex (n/%)a | |
| Female | 169 (89.9%) |
| Male | 19 (10.1%) |
| Age (years)b | 25.0 (24–28) |
| Nursing experience (years)b | 2 (2–4) |
| Pediatric nursing experience (years)b | 0 (0–1.5) |
| Previous experience in CS (n/%)a | |
| Yes | 163 (87.6%) |
| No | 23 (12.4%) |
| Work unita | |
| Intensive care (adult) | 60 (45.5%) |
| Pediatric hospitalization floor | 32 (24.2%) |
| Emergency (adult and pediatric) | 10 (7.6%) |
| Neonatal | 7 (5.3%) |
| Pediatric intensive care | 6 (4.5%) |
| Intensive care and emergency | 3 (2.3%) |
| High-dependency care | 1 (0.8%) |
| Surgical | 1 (0.8%) |
| Other units: infectious disease, home care, palliative care, blood bank, mental health | 11 (8.3%) |
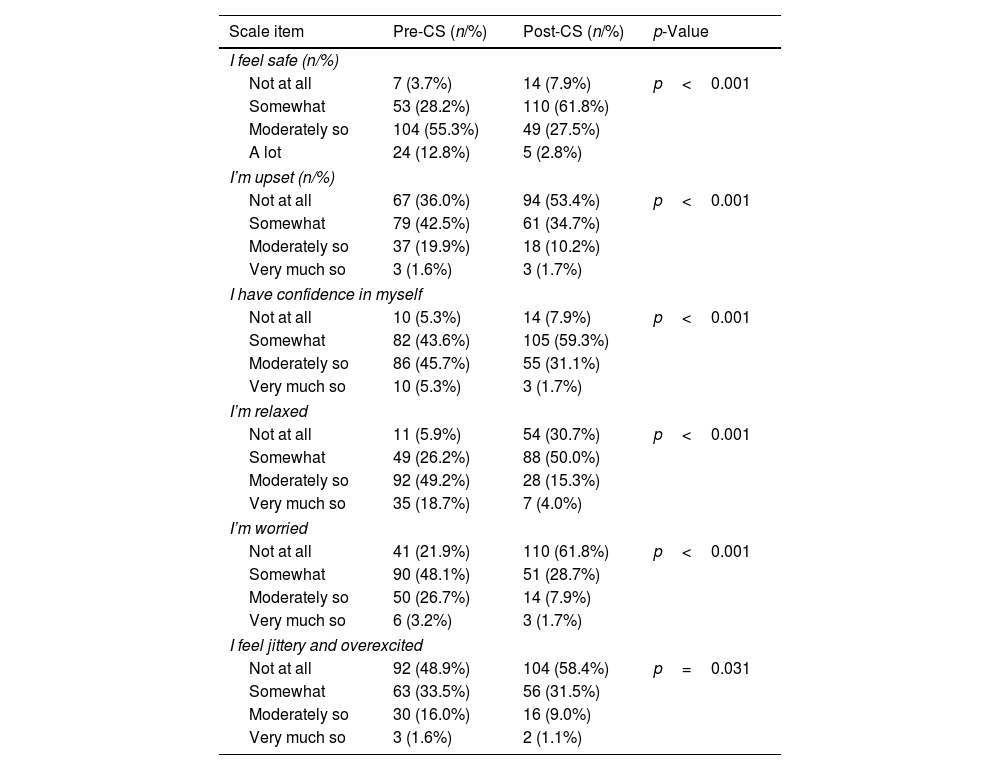
The overall median score for anxiety was 8.0 (5–10) pre-CS vs. 5.0 (3–7) post-CS (out of a total of 18 points), with a statistically significant relationship (p<0.001). At the same time, statistical significance was observed for all items related to the level of anxiety pre- and post-CS, with the exception of “I am jittery and overexcited” (Table 2).
Scores obtained on the STAI scale (n=190).
| Scale item | Pre-CS (n/%) | Post-CS (n/%) | p-Value |
|---|---|---|---|
| I feel safe (n/%) | |||
| Not at all | 7 (3.7%) | 14 (7.9%) | p<0.001 |
| Somewhat | 53 (28.2%) | 110 (61.8%) | |
| Moderately so | 104 (55.3%) | 49 (27.5%) | |
| A lot | 24 (12.8%) | 5 (2.8%) | |
| I’m upset (n/%) | |||
| Not at all | 67 (36.0%) | 94 (53.4%) | p<0.001 |
| Somewhat | 79 (42.5%) | 61 (34.7%) | |
| Moderately so | 37 (19.9%) | 18 (10.2%) | |
| Very much so | 3 (1.6%) | 3 (1.7%) | |
| I have confidence in myself | |||
| Not at all | 10 (5.3%) | 14 (7.9%) | p<0.001 |
| Somewhat | 82 (43.6%) | 105 (59.3%) | |
| Moderately so | 86 (45.7%) | 55 (31.1%) | |
| Very much so | 10 (5.3%) | 3 (1.7%) | |
| I’m relaxed | |||
| Not at all | 11 (5.9%) | 54 (30.7%) | p<0.001 |
| Somewhat | 49 (26.2%) | 88 (50.0%) | |
| Moderately so | 92 (49.2%) | 28 (15.3%) | |
| Very much so | 35 (18.7%) | 7 (4.0%) | |
| I’m worried | |||
| Not at all | 41 (21.9%) | 110 (61.8%) | p<0.001 |
| Somewhat | 90 (48.1%) | 51 (28.7%) | |
| Moderately so | 50 (26.7%) | 14 (7.9%) | |
| Very much so | 6 (3.2%) | 3 (1.7%) | |
| I feel jittery and overexcited | |||
| Not at all | 92 (48.9%) | 104 (58.4%) | p=0.031 |
| Somewhat | 63 (33.5%) | 56 (31.5%) | |
| Moderately so | 30 (16.0%) | 16 (9.0%) | |
| Very much so | 3 (1.6%) | 2 (1.1%) | |
Note: STAI=state-trait anxiety inventory.
In the case of stress, we observed scores of 3.0 (2–4) points pre-CS vs. 2.0 (1–3) post-CS (out of 5 points), also with statistical significance (p<0.001).
An overall self-confidence in learning score of 25.0 (22–28) points was obtained. If we break down the values obtained according to the SCLS items, a median score of 3.0 (2–3) points out of 5 was observed for the subject, 4.0 (3–4) for included content, 4.0 (3–4) for carrying out the CS, 4.0 (3–4) for resources used, 4.0 (3–4) points for professional responsibility, 4.0 (3–5) for ability to request help and, 4.0 (3–4) for communication skills, teamwork, and leadership.
Finally, the overall median satisfaction score was 5.0 (4–5) out of 5. The utility of the CS, the available resources, and participants’ comfort with the activity obtained a score of 4.0 (4–5) points, while satisfaction with the learning approach and the fit between theory and practice obtained scores of 4.0 (4–5) and 4.0 (4–5) points, respectively.
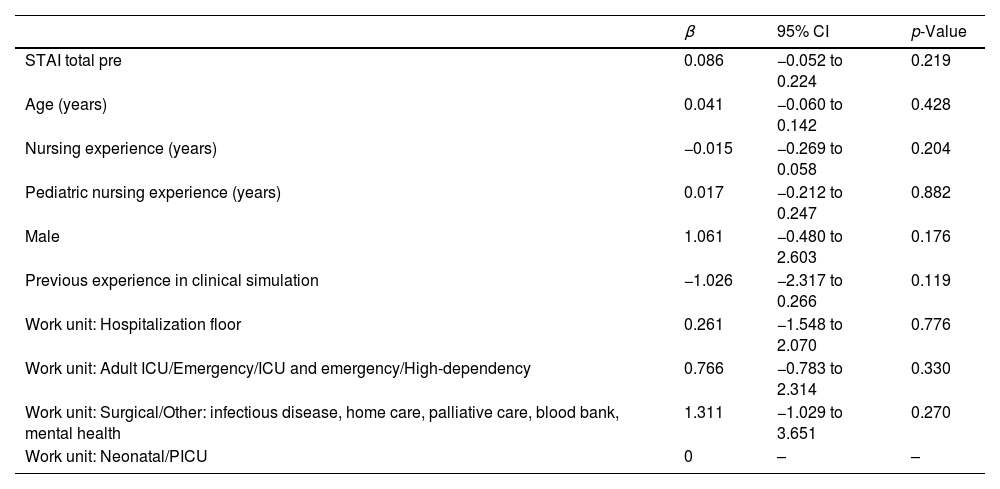
Relationship between sociodemographic and professional variables, anxiety, stress, and self-confidence in learningThe multivariate model shows that there are no statistically significant relationships between the sociodemographic and professional variables and final scores for anxiety (Table 3).
Analysis of covariance for anxiety after clinical simulations.
| β | 95% CI | p-Value | |
|---|---|---|---|
| STAI total pre | 0.086 | −0.052 to 0.224 | 0.219 |
| Age (years) | 0.041 | −0.060 to 0.142 | 0.428 |
| Nursing experience (years) | −0.015 | −0.269 to 0.058 | 0.204 |
| Pediatric nursing experience (years) | 0.017 | −0.212 to 0.247 | 0.882 |
| Male | 1.061 | −0.480 to 2.603 | 0.176 |
| Previous experience in clinical simulation | −1.026 | −2.317 to 0.266 | 0.119 |
| Work unit: Hospitalization floor | 0.261 | −1.548 to 2.070 | 0.776 |
| Work unit: Adult ICU/Emergency/ICU and emergency/High-dependency | 0.766 | −0.783 to 2.314 | 0.330 |
| Work unit: Surgical/Other: infectious disease, home care, palliative care, blood bank, mental health | 1.311 | −1.029 to 3.651 | 0.270 |
| Work unit: Neonatal/PICU | 0 | – | – |
Abbreviations: STAI=state-trait anxiety inventory, ICU=intensive care unit, β=parameter estimate, CI=confidence interval. Data are shown as estimated βs (95% CIs) of the explanatory variables. The β parameter estimate is defined as the degree of change in the STAI total post for every one unit of change in the predictor variable. The p-value is based on the null hypothesis that all βs relating to an explanatory variable equal zero (no effect).
Adjusted R2=0.35.
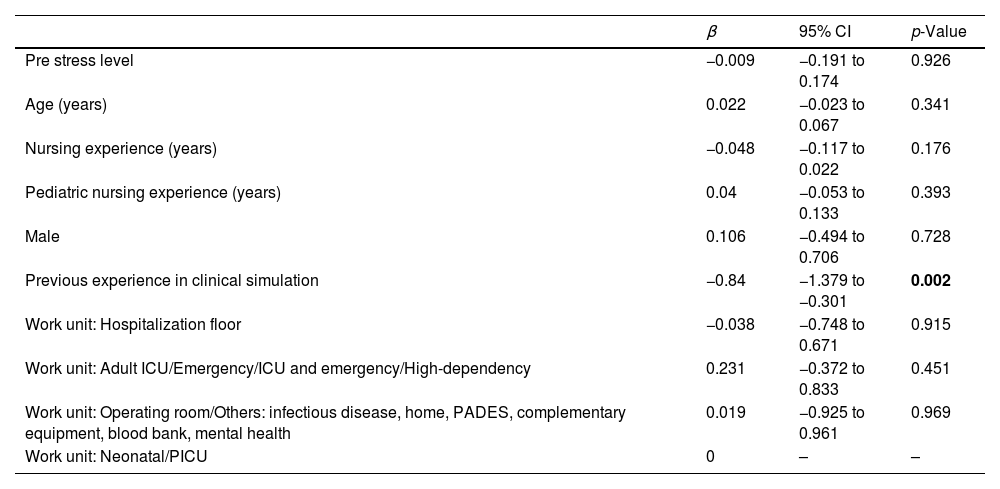
Previous experience in CS was independently related to a lower level of stress after performing the CS (β=−0.84, p=0.002) (Table 4).
Analysis of covariance for stress after clinical simulations.
| β | 95% CI | p-Value | |
|---|---|---|---|
| Pre stress level | −0.009 | −0.191 to 0.174 | 0.926 |
| Age (years) | 0.022 | −0.023 to 0.067 | 0.341 |
| Nursing experience (years) | −0.048 | −0.117 to 0.022 | 0.176 |
| Pediatric nursing experience (years) | 0.04 | −0.053 to 0.133 | 0.393 |
| Male | 0.106 | −0.494 to 0.706 | 0.728 |
| Previous experience in clinical simulation | −0.84 | −1.379 to −0.301 | 0.002 |
| Work unit: Hospitalization floor | −0.038 | −0.748 to 0.671 | 0.915 |
| Work unit: Adult ICU/Emergency/ICU and emergency/High-dependency | 0.231 | −0.372 to 0.833 | 0.451 |
| Work unit: Operating room/Others: infectious disease, home, PADES, complementary equipment, blood bank, mental health | 0.019 | −0.925 to 0.961 | 0.969 |
| Work unit: Neonatal/PICU | 0 | – | – |
Abbreviations: ICU=intensive care unit, NICU=neonatal intensive care unit, β=parameter estimate, CI=confidence interval. Data are shown as estimated βs (95% CIs) of the explanatory variables. The β parameter estimate is defined as the degree of change in the stress level post for every one unit of change in the predictor variable. The p-value is based on the null hypothesis that all βs relating to an explanatory variable equal zero (no effect).
Adjusted R2=0.38.
Finally, we observed that, independently, the older the age, the higher the level of self-confidence in learning (β=0.157, p=0.020).
We found no links between overall satisfaction and the other variables.
DiscussionThis is one of the studies focusing on postgraduate nursing students who have direct contact with pediatric patients in clinical practice. One particularly novel finding is that greater professional experience is associated with lower stress levels after the CS. Another finding is that older participants had greater self-confidence in their ability to learn. While we did not measure participants’ learning, their self-reports of learning 25.0 (22–28) coincide with other studies in which an educational intervention based on simulation significantly improved clinical performance, time to start of key clinical tasks, teamwork during simulated pediatric resuscitation,28 knowledge score of the student before and after simulation-based CPR (values of 5.66 (SD: 1.97) pre versus 8.38 (SD: 1.30) post CS),29 knowledge and skills related to immunization in nursing (12.5 (SD: 2.56) pre-test versus 17.4 (SD: 2.38) post-test),21 safety practices in implementing medication30 and in the pediatric end-of-life context.31 They also align with findings by Clephane et al. in the 202320 and Aiham et al. in 2019,10 in which participants rated their acquisition of knowledge and technical and non-technical skills after CS as high. At the same time, a recent systematic review focusing on pediatric emergency team training found an improvement in clinical performance and technical skills for at least 2–6 months and an apparently inconclusive improvement in patient survival.32
Among our participants, the overall mean anxiety score was 2.5 points lower after the CS than before, coinciding with research by Martínez-Arce et al. (2021),18 who noted a significant decrease of 12.5 (SD: 8.4) when comparing state anxiety scores before and after SC, as in other studies.17,33 The presence of anxiety before CS may be related to the fact that CS requires participating actively, performing in front of peers, and handling unfamiliar equipment in an unfamiliar setting.19,34,35 To alleviate students’ discomfort, strategies can be established prior to the CS, such as clarifying objectives, roles and expectations and expressing calmness, commitment, and respect toward all participants.36
Considering that anxiety and stress are reactions that prepare us for action, they have negative effects such as nervousness. However, this activation also has benefits in that it encourages motivation for learning and increases the degree of retention of what has been learned.37 Similarly, an increase in anxiety during CS has been shown to lead to an increase in student self-confidence during clinical practicums and, by extension, during their professional activities.34 Our study supports this finding by showing that moderate anxiety and stress coincided with adequate self-confidence in learning.
Although participants experienced anxiety, they perceived CS as useful to their learning, coinciding with research performed by Cantrell et al. de 201738 and reported a high degree of satisfaction. This is also in line with the research by Boling et al. conducted with nurses in an adult cardiothoracic ICU, who described an increase in both knowledge (48.18 (SD: 14.7) vs. 60.9 (SD: 22.6); p<0.05) and self-perception (20.8 (SD: 5.17) vs. 25.9 (SD: 3.3); p<0.05) before and after the implementation of a training plan with CS.39 Smallheer et al. and Ballangrud et al. found similar results in their research with critical care nurses, finding that CS helped them to increase their confidence, knowledge and therefore satisfaction with the methodology.40,41 These results can be extrapolated to the context of pediatric intensive care. A study conducted in 2022 with 24 new nurses also found an improvement in professional confidence, with high self-perceived competence at the end of CS in relation to different clinical management tasks,42 similar to another conducted with 500 participants.43
In our case, satisfaction was 4.3 (SD:0.8) out of 5, which coincides with another study in which satisfaction values between 4.06 (SD:1.01) and 4.92 (SD: 0.31) were obtained for all aspects valued44 and with that of Alconero et al. (2020), in which 87% of items had a mean score of at least 4 out of 5.45
The main limitations of the research are the small sample size, the fact that it was conducted in a single center, the lack of validated scales for some measures, particularly perceived stress, and the lack of a control group.
ConclusionsParticipants presented anxiety and stress before CS, which decreased after CS. At the same time, they showed a medium level of satisfaction and self-confidence in learning. Faculties and pediatric intensive care units should also consider the variables of age and experience to design CS experiences that are effective while minimizing anxiety and stress.
Ethical considerationsPermission was granted from the administration and two department heads of the Faculty of Nursing.
FundingThis work was supported by the University of Barcelona Research in University Teaching Program (REDICE 22-3305).
Conflict of interestThe authors declare no conflict of interest.