To identify the relationship between women’s knowledge, beliefs, and behaviors and human papillomavirus (HPV) transmission prevention.
MethodThis was a cross-sectional study with a convenience sampling technique. The samples were from 649 women of reproductive age who either were married or who had once been married. Data were analyzed using the Pearson and Spearman correlation tests.
ResultsThe results showed a statistically significant relationship between knowledge, beliefs and sexual behaviors, and the prevention of HPV transmission. Knowledge was the most dominant variable affecting the prevention of HPV transmission (r=0.174) with p value < 0.001; the better the women’s knowledge, the higher the prevention effort.
ConclusionsBeliefs regarding HPV transmission, healthy sexual behavior, and knowledge of prevention could reduce the prevalence of HPV transmission and would improve women’s health in general. In addition, providing education, avoiding the risk factors, early detection, and performing a regular screening of reproductive organs are the key factors in preventing HPV transmission.
Cervical cancer (CC) is primarily caused by persistent infection of human papillomavirus (HPV), including type 16, 18, 31, and 45, among sexually active women1,2. CC is a major disease burden among women, especially in low and middle income countries (LMIC)3. More than 85% of deaths due to CC occur in LMIC, including Indonesia3,4.
Indonesia is the fourth most populous country in the world after China, India and the United States, with more than 257 million people inhabiting the largest archipelago on earth5. CC control is a tremendous issue in this country. Due to a variety of elements, including the characteristics of its population, its geography, the education system, economic and sociocultural factors, and the health care system. There are some regions in Indonesia, which report the highest CC morbidity rate. The National Health Survey in 2013 by the Ministry of Health of the Republic of Indonesia reported that CC cases are most prevalent in three particular provinces: East Java (21,313 cases), Central Java (19,734 cases), and West Java (15,635 cases)6.
Poor knowledge is the predominant factor impeding preventative measures against cervical cancer7. Another barrier, especially among Asian women, is sociocultural factors8. Knowledge and beliefs strongly affect women’s perception and behavior in performing cervical cancer prevention and early detection9. These conditions eventually lead to a low coverage rate of CC screening; as low as 5% in Indonesia10.
Many studies have examined the knowledge, beliefs, and behaviors related to the prevention of cervical cancer11–16. This interrelated subject is no longer new; however, it remains vital to assess this fundamental issue for problem mapping and policymaking in cancer control. Therefore, in this present study, we identified the women’s knowledge, beliefs, and behaviors regarding HPV transmission prevention in the three most CC-prevalent regions in Indonesia.
MethodThis was a correlational research with a cross-sectional design. Using a convenient sampling method, we recruited 649 consenting women who had been sexually active (married or once married) in three different regions in Indonesia. These regions were selected due to their high incidence of cervical cancer. The Ethical Committee of the Faculty of Nursing University of Indonesia reviewed and approved this study. Careful considerations of ethical conduct were applied throughout the study, from the design and implementation through to the completion of the study.
We used a questionnaire (the Awareness of HPV and Cervical Cancer Questionnaire) developed by Jenkins et al17. This tool contains 55 questions and statements to measure the knowledge, beliefs, and sexual behavior, in the prevention of HPV transmission. We conducted reliability tests in different populations prior to data collection and got the score of 0.916; 0.921, and 0.894 for the knowledge, beliefs, and behavior, respectively. The validity test also showed that this tool is valid.
We added the Cervical Cancer Knowledge Prevention 64 Questionnaire to assess the cervical cancer prevention acts in our respondents18. The pilot test yielded validity and reliability scores of 0.448-0.727 and 0,888.
Data analysis was conducted through univariate, bivariate, and multivariate analysis. We used frequency distribution and central tendency for the univariate analysis; Pearson and Spearman correlations for the bivariate analysis, and linear regression for the multivariate analysis.
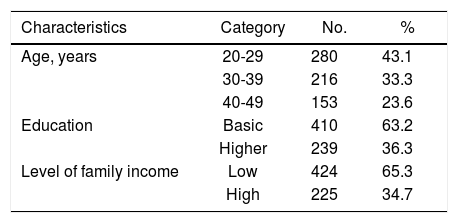
ResultsThe characteristics of all respondents in this study are summarized in Table 1. The respondents were evenly distributed across different age spans with a slight majority being in the age group of 20-29 years-old (43.1%). Most respondents had a lower education level (63.2%) and came from a poorer economic background (65.3%).
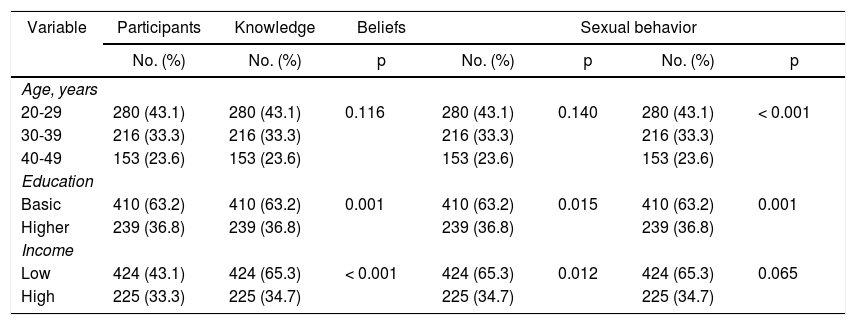
Table 2 summarizes the distribution and bivariate analysis to identify the relationship between knowledge, beliefs, and sexual behavior and the prevention of HPV transmission.
Women’s knowledge, beliefs, and sexual behavior according to their age group, education, and income level.
| Variable | Participants | Knowledge | Beliefs | Sexual behavior | |||
|---|---|---|---|---|---|---|---|
| No. (%) | No. (%) | p | No. (%) | p | No. (%) | p | |
| Age, years | |||||||
| 20-29 | 280 (43.1) | 280 (43.1) | 0.116 | 280 (43.1) | 0.140 | 280 (43.1) | < 0.001 |
| 30-39 | 216 (33.3) | 216 (33.3) | 216 (33.3) | 216 (33.3) | |||
| 40-49 | 153 (23.6) | 153 (23.6) | 153 (23.6) | 153 (23.6) | |||
| Education | |||||||
| Basic | 410 (63.2) | 410 (63.2) | 0.001 | 410 (63.2) | 0.015 | 410 (63.2) | 0.001 |
| Higher | 239 (36.8) | 239 (36.8) | 239 (36.8) | 239 (36.8) | |||
| Income | |||||||
| Low | 424 (43.1) | 424 (65.3) | < 0.001 | 424 (65.3) | 0.012 | 424 (65.3) | 0.065 |
| High | 225 (33.3) | 225 (34.7) | 225 (34.7) | 225 (34.7) | |||
This study found a statistically significant relationship between knowledge, beliefs, sexual behavior and the prevention of HPV transmission. A larger sample size in the present study might lead to consistency of statistical and practical significance, despite the need to render true representation of the population of women being studied. Previous studies suggested a marked relationship between knowledge and cancer prevention behavior11,19,20. Consistent study results were shown by previous studies in Tanzania and Indonesia21,22. These studies found that the women with higher a level of knowledge tend to perform cervical cancer preventive measures and screening. Meanwhile, McRae et al. revealed that most women knew about HPV infection and vaccination yet were inadequately informed about cervical cancer early detection23. Therefore, it is worth noting that in spite of being a critical entry point for public awareness, knowledge is less likely to affect prevention and early detection behavior unless it is very thorough.
Health beliefs, on the other hand, are an inherent compelling factor upon which an individual may take action for disease prevention as outlined by Strecher and Rosenstock’s Health Belief Model24,25. In this study, the median value (34, out of min-max 27-47) reflects the typical health beliefs of the respondents. Further analysis yielded conflicting results between statistical and clinical significance. Hence, this finding must be interpreted with care.
A recent study captured the health beliefs of older women in the Mid-Atlantic Section of the United States26. It was reported that even though they regarded cervical cancer as a serious illness, they did not perceive themselves as being vulnerable to cervical cancer and its precursor. Knowledge and health beliefs are significantly related, in that women with less knowledge regarding HPV and cervical cancer have less awareness of the seriousness of their risk of developing recurrent HPV infection and cervical cancer26. As a consequence, they would also lack the anticipatory behavior required to prevent the threat of that particular illness.
As their age increases, women in this study are less likely to perform preventive measures against HPV infection. Similar results were found in previous studies among populations of Asian descent27,28. Even though there was one study that mentioned no association between age and attitude and cervical cancer prevention behavior29, overall cervical cancer screening uptake is significantly higher among younger women, particularly those aged 20-35 years old27,28. Despite being at increased risk for developing sexually transmitted diseases and cervical cancer, women aged 40 and older tend to perceive cervical examination as a taboo, as well as having less knowledge and more misleading health beliefs regarding cervical cancer26,30.
Women with better knowledge and beliefs regarding HPV and cervical cancer prevention, and safer sexual behaviors, are more likely to carry out preventive practices against HPV transmission. Knowledge is the most important factor to affect prevention of HPV transmission, which eventually aims at cervical cancer prevention.
Emphasis should be placed on raising public awareness of this issue. Nurses should play a role in educating women to prevent sexually transmitted diseases, to avoid early sexual debut (in women under 20 years old), and to perform routine screening for cervical cancer. As well as targeting women of reproductive age, the older population of women also needs to have special attention paid to them, as they are highly prone to cervical cancer while having more barriers against its prevention. Further studies may address strategies or innovations to improve public awareness, beliefs, and practices of cervical cancer prevention, particularly in Indonesia.
We wish to thank the Directorate of Research and Community Service, Universitas Indonesia, for their financial support, and the Director of the Persahabatan Hospital and the staff in the gynecology outpatient unit, for technical and other support.
Conflicts of interestThe authors have no conflicts of interest to declare.