This study aims to develop the maternal blues scale of the antepartum period through bonding attachment, and the closeness of the mother to the fetus.
MethodsDesign of the development items of maternal blues scale is cross-sectional. The number of research samples is 450.
ResultsThe number of statements had produced from the maternal blues scale through absolute measurements, incremental appropriateness measurements, construct validity (CR), and variant extraction (VE) were 24 items had been declared valid and reliable. The maternal blues suryani model's (MBS) scale has been grouped into two variables; internal variables (maternal roles and tasks) eight items and external (cultural, social support) 16 items.
ConclusionsThe MBS scale through bonding attachments had been valid and reliable to predict postpartum blues.
One factor that can affect that mother condition is pregnancy. Where physical changes during pregnancy have been triggering various things including psychological problem.1 Several factors can affect the psychological condition of the mother during pregnancy, which is a wrong understanding of physical changes, unrealistic expectations, support, culture, and economy. That condition affects the emotional and mood of the mother at risk of rejection of her pregnancy.2
Depression is one of the complications that often occur during pregnancy from the mild phase (maternal blues) to advanced stages (depression) and causes of disability both for the growth of children and mother.3–6 Depression during antepartum varies, 7.4% in the first trimester, 12.8% in the second trimester and 12 percent in the third trimester.7 Twelve point seven percent of pregnant women who have depression are major depression.7 The incidence of maternal blues in Indonesia in 2004 at Persahabatan Hospital was 37%, in 2013 it was 56.7% in Bogor.8,9 The condition of stress experienced by Indonesian women during pregnancy has increased the risk of depression after childbirth.10 Antepartum blues is one of the predictors of postpartum depression.5,11 Blues that occur since antepartum will develop and reach severe blues conditions on the fifth day postpartum.11 That information has illustrated that there was a relationship between antepartum and the incidence of postpartum depression.11 Before the blues develop into depression, early detection of maternal blues is a preventive effort in reducing incidents of disability in children and mothers. Some how to detect blues is to see changes in emotions and mood associated with maternal and fetal interactions. Where previous information states that blues has a negative influence on mother and fetal bonding. The blues mother correlates with the poor bonding relationship between mother and fetal.12,13
Emotional and mood changes of the mother toward mother and fetal interactions are influenced by several factors, such as the mother's role and tasks, culture, economy and social support.14 That happens when the mother views that the role and task of being a mother is something difficult, difficulty in implementing, internally the mother has shown emotional and mood changes, which has been shown by the reduced interaction between the mother and fetal, rejection, irritability.15,16 The influence of external factors also contributes to the style of maternal bonding attachment and fetal namely culture, economy and social support.17,18
The scale that previous predicts the maternal blues was the Kennerley scale, Pitt and Stein.19,20 The scale explores the mother's mood and emotions in general, including anger, anxiety, easy crying, erratic feelings.19 Based on previous information had stated that the psychological condition of the mother during pregnancy, emotional and mood changes during the transition phase is at risk of rejection and termination of her pregnancy, absence of attachment to the fetal.14,21,22 Based on the background of the information the researchers had developed a scale based on the relationship between mother and fetal interaction (bonding attachment fetal) to predict postpartum blues. The originality of the maternal blues scale in pregnant women that postpartum blues prediction had developed at that time with the previous one is (1) scale according to Indonesian cultural background (2) developed based on the mother's emotional and mood conditions on the relationship of maternal and fetal interactions (bonding attachments) during pregnancy (3) the scale is specifically for predicting postpartum blues (4) written in Indonesian has not been the result of cultural adaptation.
The developed scale has been grouped into two factors; internal and external factors. Internal factors are information that provides an overview of the emotional and mood changes of the mother in interacting with the fetus. External factors are information that provides an overview of supporting factors that influence the occurrence of emotional and moods changes in interacting with the fetal. It is expected that maternal and infant welfare will increase.
This study aims to develop items the scale of maternal blues of antepartum period through bonding attachments in predicting postpartum blues. The research hypothesis is to prove (1) the scale of maternal blues in pregnant women is valid and reliable in predicting postpartum blues. (2) The scale of maternal blues in pregnant women that predicting postpartum blues has correlated with the Kennerley maternity blues scale. (3) The maternal blues scale can be a screening tool in predicting postpartum blues.
MethodDevelopment items of maternal blues scale in the antepartum period had been designed to identify behavior blues is a psychological test. So that the design of the study is cross-sectional. Where data collection for each subject had been carried out at one time and once.23
The place of research is at public health services (PHSs) in South Jakarta. The selected PHSs were Jagakarsa, Pasar Minggu, Tebet, West Cilandak, Kebayoran Lama sub-districts health services. The reason for choosing the PHSs as the research location is that the PHSs have a high birthrate monthly (± 50deliveries/month), a heterogeneous population with various economic, ethnic and religious backgrounds. Data collection has been done by distributing questionnaires to respondents.
The data collection tool used was the draft of maternal blues scale of antepartum of the Suryani's model and the Kennerley maternity blues scale. Before using the Kennerley maternity blues scale has obtained informed consent on December 3, 2015. Kennerley's model of the maternity blues has been adapted into the Indonesia language. The maternal blues Suryani's model (MBS) scale of the antepartum period had been prepared on a Likert scale with positive and negative statements. The answer option consists of very appropriate, appropriate, lack of appropriate, inappropriate, very inappropriate.
The population who were respondents in the study were a pregnant woman. The inclusion criteria of respondents who to be sampled were a normal pregnancy, third trimester of pregnancy, living children, absence complications. Determination of the sample size for the construct validity of measuring instruments and sensitivity measurements have been adjusted to the number of developed items of statements namely 5–10: 1 (items) built.24 The initial draft of the MBS scale had been constructed 55 items of statements. The sample had been taken by the researcher was 450 respondents. The sampling method has been done by non-probability sampling technique by purposive sampling (judgmental sampling). Where samples have been taken according to the specified inclusion criteria.
The applied ethical principle during this research was the beneficence principle. Before the questionnaire had been distributed to respondents, prior informed consent had been given; namely, an explanation of the study and respondents signed an agreement. Respondents had also been given the opportunity to refuse and give approval as respondents. The collected data has been anonymized and used only for research. Data storage has been done by internet media files which can only be opened by researchers. Previous research activities have been approved through ethical tests from the ethics committee of the Faculty of Nursing Universitas Indonesia with number 0538/UN2.F12.D/HKP.02.04/2016.
The data will then be processed with several measurement methods; the model equation, parallel test, and diagnostic test. The model equation (structural equation modeling/SEM) through explanatory factor analysis (EFA) and confirmatory factor analysis (CFA).23 EFA uses software SPSS 22 and CFA uses software the LISREL 8.7 program. SEM is used to assess measurable variables of indicators in describing validity and reliability.23 Some model validity indicators are t value, standardized loading. Indicators to test data reliability are used variance extracted (VE) and construct reliability (CR).
Parallel tests are a correlation analysis, which compares the measurement results of the MBS scale with the standard instruments (Kennerley maternity blues scale) that have been adapted into Indonesia language.25 Then compare between internal and external factors of MBS scale. The used analysis is Spearman's analysis. ROC analysis had been carried out in the diagnostic test to obtain value the area under the curve (AUC) with a value between 50% and 100%.
ResultsParticipated respondents in this study as many as 450 people from five PHSs; Tebet, Cilandak, Kebayoran Lama, Pasar Minggu, Jagakarsa health services, with normal deliveries. The collected answers from 450 respondents to 55 item statements, from the results of EFA measurements, had been obtained eleven factors (latent variables) with 38 item statements (indicator variables). The evaluation criteria for these items have the value of Barlett Test of Sphericity with Chi-Square 8550.751 (df 703) and a significant t value (<0.05) with criteria for loading factors ≥0.4 (0.50–0.886) and internal consistency (Alpha Cronbha) 0.498–0.877. Selected modeling toward of latent variables and indicator variables is then carried out measurement models by CFA analysis.
The estimation results of the model at 38 item statements CFA, so selected variables indicator are 24 item statements of latent variables; F1, F2, F3, F4, F5, F7. Selected internal laten variables are F4, F5. Selected external laten variables are F1, F2, F3, F7. The measurement results can be seen in Tables 1 and 2.
Validity and reliability of latent variables (internal factors) antepartum maternal blues scale (n=450).
| Latent variable | Indicator variables (statement items) and statement item numbers | Standardized Loading Factor (SLF)≥0.50 | T value | CR≥0.70 | VE≥0.50 |
|---|---|---|---|---|---|
| F4(The role and tasks of the mother) | Feeling ashamed of the movement of the baby in the womb seen from clothes (11). | 0.75 | 12.59 | 0.89 | 0.67 |
| The movement of the baby in the womb is painful (10). | 0.64 | 13.08 | |||
| the Movement of the baby in a disturbing womb (12). | 0.84 | 13.28 | |||
| Not ready to accept the responsibility of being a mother (31). | 0.58 | 10.37 | |||
| Say hello to the baby by saying good words(25) | 0.63 | 13.91 | |||
| F5(The role and tasks of the mother) | Nice to feel the baby's movements in the womb (9) | 0.58 | 13.49 | 0.89 | 0.74 |
| Feel happy every stimulate the baby in the womb through my stomach (14). | 0.75 | 11.34 | |||
| Happy when the baby in the womb responds to my swab on the stomach (15) | 0.87 | 11.69 | |||
Validity and reliability of latent variables (external factors) antepartum maternal blues scale (n=450).
| Latent variable | Indicator variables (statement items) and statement item numbers | Standardized Loading Factor (SLF)≥0.50 | T value | CR≥0.70 | VE≥0.50 |
|---|---|---|---|---|---|
| F1(Cultural and social support) | Feel calm accompanied by parents during pregnancy (52) | 0.67 | 12.3 | 0.93 | 0.60 |
| Happy with parents’ choice name for my future baby (35) | 0.79 | 13.35 | |||
| Happy, parents give names to prospective babies (32) | 0.68 | 12.19 | |||
| Glad to get help from parents during pregnancy (53) | 0.55 | 10.30 | |||
| Trust in Parents makes me more confident to be a mother (47). | 0.69 | 12.33 | |||
| Feel happy the family accepts a prospective my baby (36). | 0.70 | 12.51 | |||
| Glad my husband chose the name for my future baby (33). | 0.67 | 12.10 | |||
| Glad to get attention from a parent while pregnant (45). | 0.70 | 12.52 | |||
| F2(Social support) | Happy my husband helped me during pregnancy (48) | 0.63 | 14.48 | 0.94 | 0.85 |
| Glad my husband took care of me during pregnancy (49) | 0.90 | 14.45 | |||
| Parental affection strengthens me to face labor (46) | 0.88 | 13.83 | |||
| F3(Social support) | Stress carry out parental rules during pregnancy (42). | 0.75 | 11.96 | 0.92 | 0.78 |
| Feeling pressured against a parental advice in caring for pregnancy (43). | 0.95 | 17.78 | |||
| Stress activity is restricted during pregnancy (44) | 0.73 | 15.68 | |||
| F7(Social support and cultural) | I am angry that my husband says I have not been able to become a mother (55).Sad for not carrying out the baby welcoming ceremony during pregnancy (39). | 0.63 | 5.87 | 0.46 | 0.30 |
| 0.50 | 11.96 | ||||
Table 1 shows that four latent variables (internal factors) with eight indicator variables (statement items) have good validity and reliability with several criteria. T value loading factors are greater than the critical value (≥1.96) and standardized loading factor≥0.50, the value of CR≥0.89 and VE≥0.67–0.74. Based on these measurements it can be stated that the indicator variable (statement item) is consistent and valid in measuring latent variables (internal factors); the role and tasks of the mother in interacting with the fetal.
Table 2 shows that four latent variables (external factors) with 16 indicator variables (statement items) have had good validity and reliability with several criteria. The value of loading factors is greater than the critical value (96>1.96) and the standard loading factor≥0.50, the values of CR≥0.46–0.94 and VE≥0.30–85. Based on these measurements, it can be stated that the indicator variable (item statement) is consistent and valid in measuring latent variables (external factors), namely in making the behavior of mothers interacting with fetal while the latent variable F7 with two indicator variables (item statement) has not passed the validity and reliability test.
Based on the measurement results then the MBS scale has been requiring measurement of the model, by including the six latent variables (internal and external factors) in seeing the correlation with the postpartum blues construct. The following is presented in table three (Table 3).
Validity and reliability of the variable indicators (internal and external factors) against the latent variable antenatal blues (N=450).
| Latent variable | Indicator variables (statement items) and statement item numbers | Standardized Loading Factor (SLF)≥0.50 | T value | CR≥0.70 | VE≥0.50 |
|---|---|---|---|---|---|
| Maternal Blues | F1 (cultural and social support))/factor external | 0.90 | 12.89 | 0.83 | 0.50 |
| F2 (social support) external Factor | 0.58 | 9.45 | |||
| F3 (social support)/external Factor | 0.54 | 9.60 | |||
| F4 (The role and tasks of the mother)/internal Factor | 0.68 | 10.36 | |||
| F5 (The role and tasks of the mother)/internal Factor | 0.70 | 9.74 | |||
| F7 (social support)/external Factor | 0.68 | 6.41 |
The results of the analysis had obtained CR values for each construct of the model 0.83 and VE≥0.50. That analysis has shown the selected indicator variables that consistency in measuring latent constructs namely postpartum blues so that the selected indicator variables are F1, F2, F3, F4, F5, F7 (Table 3).
The degree of Model Appropriateness SizeThe degree of compatibility is used to describe the suitability of the model on all the indicators variables F1, F2, F3, F4, F5, F7 is the criteria of the absolute measure, incremental fit measure. All variables have met the criteria; the absolute measure value (RMSEA=0.10 (marginal fit), GFI=0.80 (marginal fit)). The meaning is good enough). Incremental fit measure value (NFI=0.90 (good fit), NNFI=0.90 (good fit), CFI=0.89 (marginal fit)). That indicator can be expressed well in describing blues empirical data.
Correlation analysisThe scores correlation antepartum of MBS scale between internal and external factors with Kennerley maternity blues has had a significant relationship (p<0.001). The magnitude of the correlation value of the MBS scale with the Kennerley maternity blues scale, internal factors 0.40 (moderate correlation) and external factors 0.41 (moderate correlation). While the correlation between the internal and external factors of MBS scale score has had a significant relationship (p<0.001). The value of the MBS scale correlation internal factors with external factors is 0.70 (strong correlation).
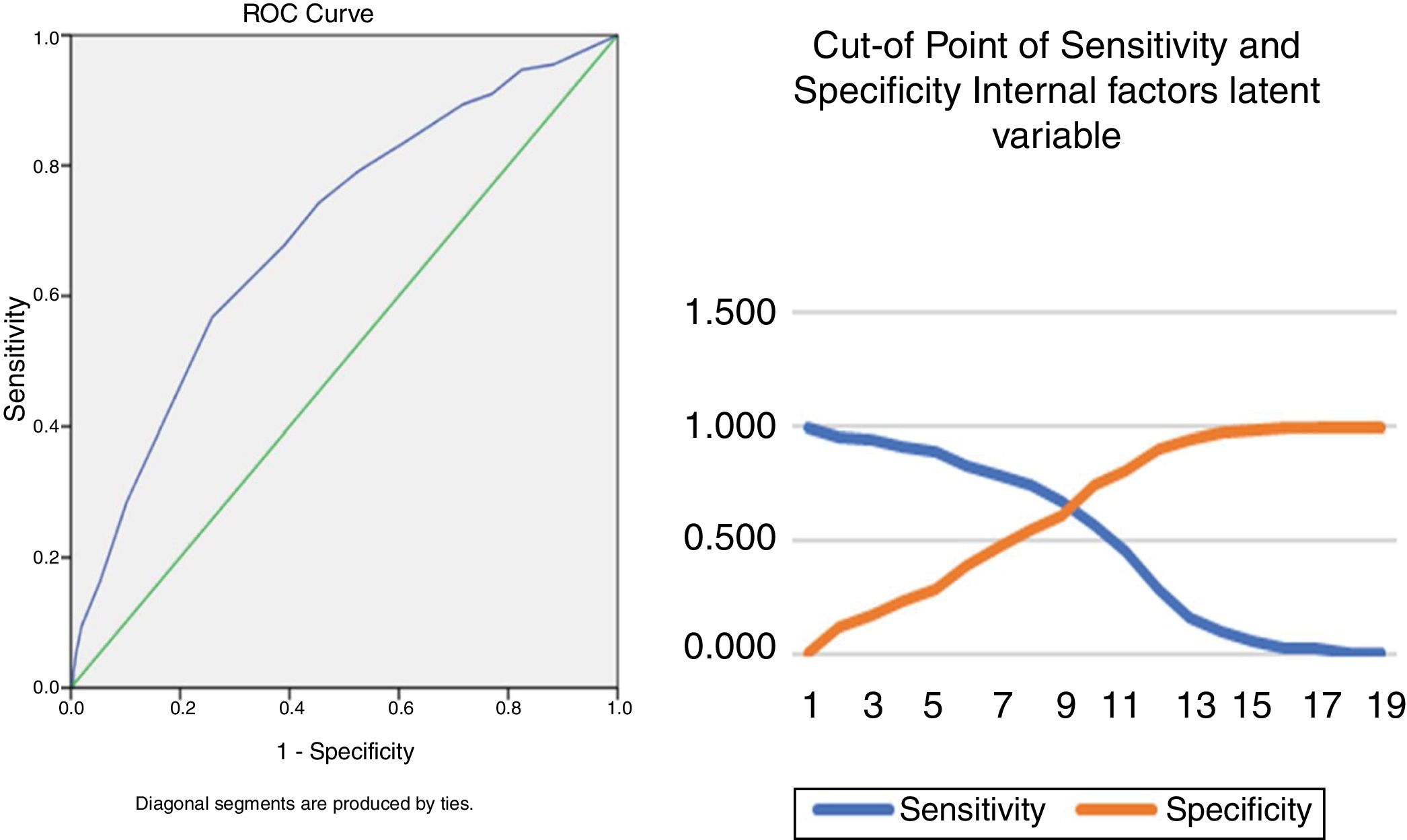
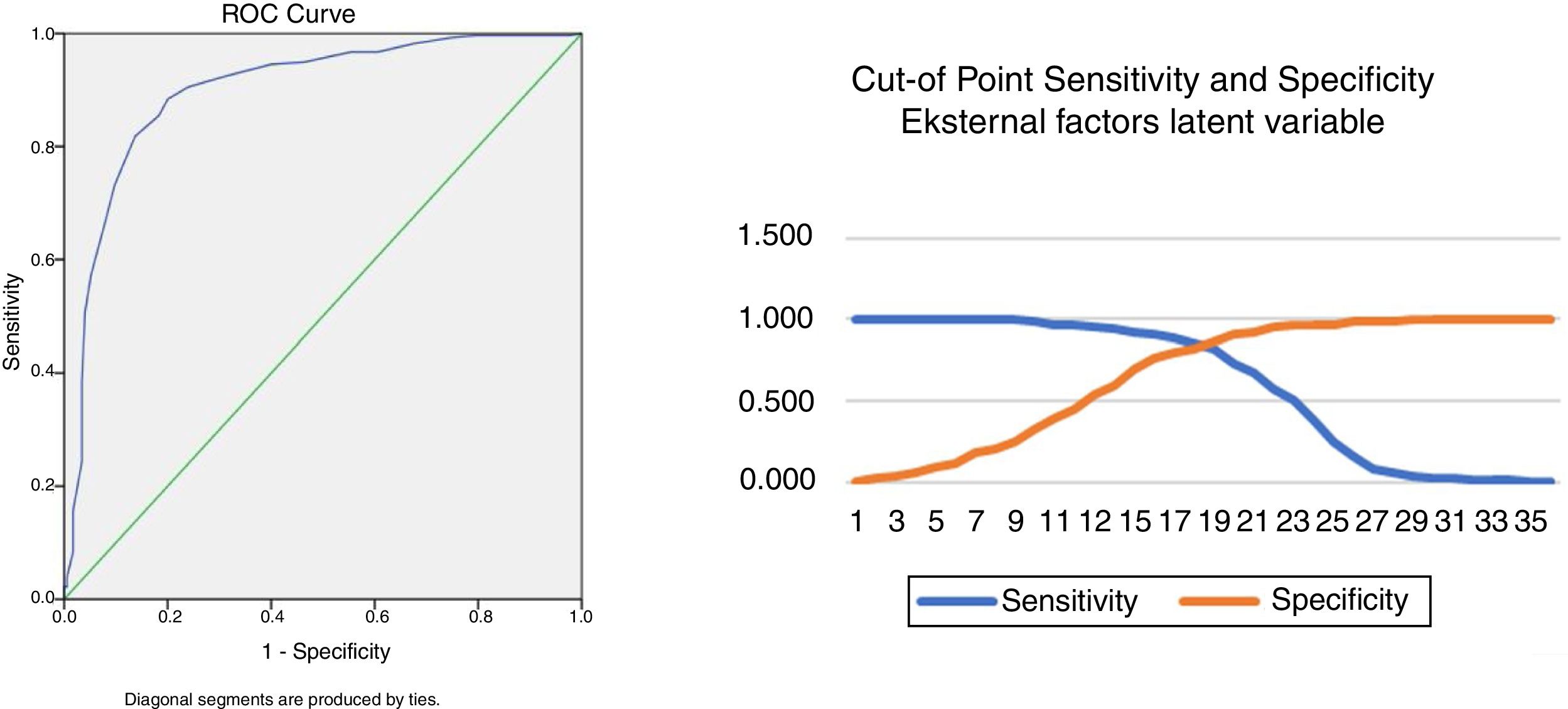
Analysis of Receiver Operating Characteristic (ROC) curvesROC analysis has produced an area under the curve (AUC) and cut-off values of internal and external variables on the antepartum MBS scale. The MBS scale cut-off values have been set for screening purposes, so the value has been based on high sensitivity values (Figs. 1 and 2).
Fig. 1, the AUC value of internal factors was 70.0% (95% CI 65.0–74.3%) p<0.05. The MBS scale was able to screen for 100 pregnant women by 70%. Based on the confidence interval, the score that has experienced maternal blues at risk in the antepartum population ranged from 65% to 74.3%. The score was significantly different from the 50% AUC score. The cut-off point for screening purposes with a sensitivity value of 74.3% is the value of 14.5 (rounding 15). So the internal antepartum MBS scale score at risk of experiencing blues is ≥15.
Figure 2, the AUC value for external factors was 89.8% (95% CI 86.7–93%) p<0.05. The MBS scale instrument was able to screen for 100 pregnant women by 89.8%. Based on the confidence intervals, scores that experienced maternal blues risk in the antepartum population ranged from 86.7% to 93%. The score was significantly different from the 50% AUC score. The cut-off point for screening purposes with a sensitivity value of 85.5% is a value of 32.5 (rounding 33). Thus the external factor of antepartum of MBS scale score at risk for blues is ≥33.
DiscussionThe development of the MBS scale in pregnant women through bonding attachments has produced a scale that can be used to predict postpartum blues. That is evidenced by the discovery that the MBS scale has validity and reliability that has been tested as a measuring of postpartum blues risk. The obtained results in support of the statement include indicator validity criteria; t value, standardized loading and indicator criteria to test the reliability of the data, namely VE and CR, all of these criteria have values that are appropriate or above standard values. Likewise, the degree of suitability of the model, the obtained value can be stated that the MBS scale both in describing the empirical blues data and has a significant correlation with the Kennerley maternity blues scale, has a significant correlation between internal and external factors of the MBS scale. In addition, the sensitivity of the MBS scale as a tool for predicting postpartum blues is quite high. Therefore variables that have been declared valid and reliable in building the scale are delivered in scale specifications.
The built specifications of the MBS scale based on the emotional and mood of the mother in interacting with the fetal are the variables of maternal roles and tasks, economic culture and social support that produce 24 item statements. Statement items are grouped into two factors, eight items internal factors (mother's role and task in interacting with the baby) and sixteen items external factors (cultural, economic, and social support that affect maternal interactions). The specifications, which have been built on the MBS scale of the antepartum period, inform that maternal role and task variables will be difficult to accept and implement when mothers experience emotional and mood changes.26 Difficulties in carrying out the role and duties of the mother during the antepartum period can be manifested by emotional and mood changes when interacting with her fetus such as reduced contact and communication.27,28 Variables of external factors (culture, social support) affect the mother's internal self in carrying out their roles and duties, one of which is fetal attachment bonding.17,27,29 Previous researchers also stated that ecological factors influence the quality of mental health and the quality of interactions between mothers and their babies.29 These factors include social support systems, family income, cultural traditions run by the family.17 Economic problems can also trigger maternal emotional and mood changes in interacting with the fetal.17
Another test that proves that the MBS scale that can predict the blues based on correlation test with the scale of maternity blues of the Kennerley's model. Based on the statistical test the strength of the relationship between the two scales is not very strong, but clinically there are effects of emotional and moods changes that experience blues with maternal interaction behavior since pregnancy.22,28 This had also been tested by previous researchers who had stated that the change in the emotional relationship between mother-to-child bonds in mothers who experience postnatal depression is the impact of depression that occurs during pregnancy and experiences changes in emotions and moods and interest power from mother to fetal.28
Other evidence that the MBS scale can predict postpartum blues is based on sensitivity tests. That is evidenced by the AUC statistical results that the scale can screen for 100 antepartum mothers above 70%. That measurement has informed that if the AUC value is above the standard 50%, it means that this instrument can be accepted as a screening tool.24 Statistical results support the MBS scale through bonding attachment as a screening tool.
The originality of the MBS scale development at this time was the observation of blues behavior through bonding attachment between mother and fetal during pregnancy. While observing blues behavior through emotional and mood changes in general for all transitional phases from pregnancy to delivery.30
This study is to a minimum of avoided errors in the selection of samples and measurements due to research limitations. The sample selection is not done randomly but is done by purposive sampling (judgmental sampling). That had been decided because of the limited time of the study to get respondents who were in accordance with the inclusion criteria. So that the technical decision to take samples with the time available during the study can meet the number of respondents according to size in the construction of measuring instruments that refer to the inclusion criteria.
Measurements have only been done based on statistical values, not referring to the gold standard or reference standard such as oxytocin levels in measuring attachments and cortisol levels, estriol which describes the emotional and mood changes of the mother. That hormone is the gold standard in the diagnostic test so that the measuring instrument becomes more accurate.
This study has produced a scale of maternal blues of the Suryani's model through bonding attachment of the antepartum period to predict the postpartum blues. This scale is called the scale of maternal blues of the Suryani's model of the antepartum period. The scale validation results that the scale is valid and reliable as a scale that predicts the postpartum blues. MBS scale has a significant relationship with the Kennerley's model of the maternity blues that has been adapted into Indonesia Language. The specifications of the MBS scale of the antepartum period are Likert scales with positive and negative statements and alternative answer choices one to five. The scale has two parts, namely statement items from internal factors and external factors. Internal factors are maternal emotional and mood conditions in carrying out roles and tasks when interacting with the fetus (bonding attachment). External factors are something that affects the emotional and mood of the mother in interacting with the fetus. The score of the MBS scale antepartum in predicting blues or not based on internal factors is 15 and the external factor is 33.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by Hibah TADOK 2018 funded by DRPM Universitas Indonesia No. 1259/UN.R3.1/HKP.05.00/2018.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.