To determine the most effective orientation program for new graduate nurses (NGNs) in hospital settings.
MethodA systematic review of existing literature was conducted following a search of the electronic databases Science Direct, PubMed, EBSCOhost, ProQuest, and Wiley Online (2008–2018). Searches utilized the following keywords nurse orientation, new nurse orientation, practical orientation, nurse transition, and nurse transition program.
ResultsA total of fourteen studies met our review criteria. Evidence from these studies showed that current orientation protocols consist of preceptorship, classes, and simulations of patient care. The most efficacious orientations had well-established goals and utilized proven learning materials, support systems such as preceptorship and mentorship, learning methods, and evaluation instruments within the organization.
ConclusionWell-designed orientation programs will result in positive effects on NGNs and patient care in the hospital.
Newly graduated nurses (NGNs) undergo a difficult transition period from student to professional nurse following graduation. NGNs are both mentally and emotionally challenged as they adjust themselves to their new profession and organization.1 Existing literature outlines several stressors on NGNs including waiting for National Council Licensure Examination (NCLEX) results, moving away from home to live independently, and adjusting to the new demands of their work environment.2 All of these new responsibilities often produce stress and anxiety.3
NGNs also face certain personal difficulties during the transition period. Studies have shown that lack of confidence, high workloads, orientation issues, fear, frustration, and being overwhelmed are frequent transition difficulties for NGNs.2,3 These can lead to transition-precipitated shock that must be recognized and addressed by nurses and hospital management. A lack of management involvement in overcoming shock can lead to negative emotions4 that can affect an NGNs’ intention to remain in nursing. Other hurdles include gaps in education, burnout, and negative experiences.5
Ideally, hospitals should be proactive when tackling these issues. Well-prepared orientation programs can help prevent shock by helping NGNs to assimilate into their new work environments and providing tools to help them adapt to their new workloads. Supportive orientation increases NGNs’ job satisfaction in the ward.6 Successful orientation programs can go a long way toward overcoming the problem of transition shock in NGNs. Hospital support of NGNs throughout the full first year of practice can promote the development of professional confidence.7 Despite this data, however, only 50.6% of nurses interviewed reported a structured orientation program at their hospitals.6 A review of existing orientation programs for NGNs could provide evidence-based strategies to improve NGN retention as well as the quality of nursing care. The study aims to determine the most effective orientation program for new graduate nurses (NGNs) in hospital settings.
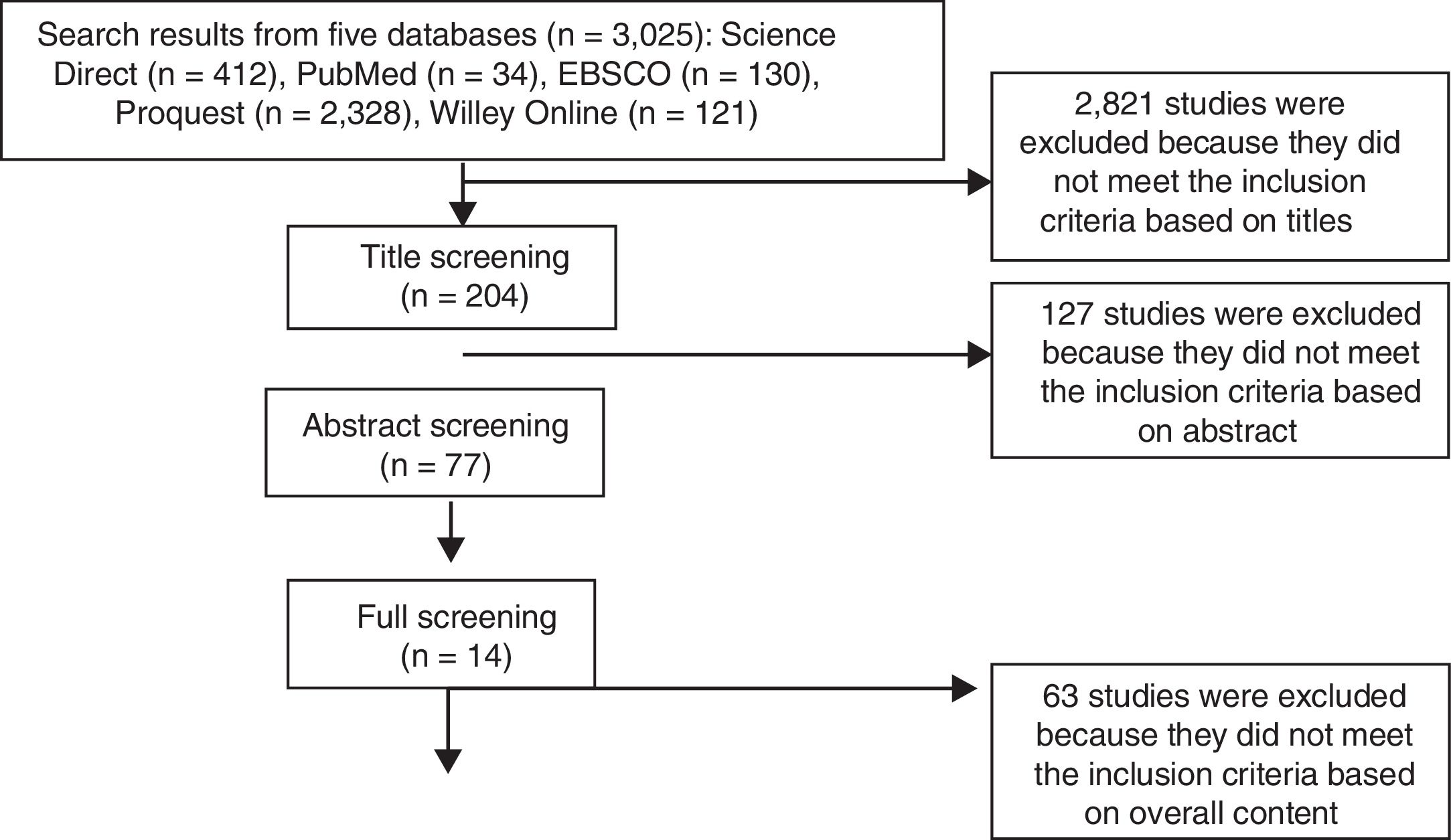
MethodSearch strategyThis systematic review was conducted by gathering data from five databases, Science Direct, PubMed, EBSCO, ProQuest, and Wiley Online, from 2008 to 2018. Data collection was performed on studies gleaned from a search using the following keywords: nurse orientation, new nurse orientation, practical orientation, nurse transition, and nurse transition program (Table 1). Suitability was determined by reviewing the title, abstract, and overall content, and fourteen studies were aligned with our selected theme. Specific inclusion and exclusion criteria are detailed in Table 2.
A database search results.
| Database | Keywords | N |
|---|---|---|
| Science Direct | “nurse orientation”“effective orientation” AND nurse“new nurse orientation”“nurse orientation program”“nurse transition” | 412 |
| PubMed | “nurse orientation”“effective orientation” AND nurse“new nurse orientation”“nurse orientation program”“nurse transition program” | 34 |
| EBSCO | “nurse orientation”“effective orientation” AND nurse“new nurse orientation”“nurse orientation program”“nurse transition” | 130 |
| ProQuest | “nurse orientation”“effective orientation” AND nurse“new nurse orientation” | 2,328 |
| Willey Online | “nurse orientation”“effective orientation” AND nurse“nurse transition program”“nurse transition” | 121 |
| Total | 3,025 |
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
| New graduated general nurse from the hospital | New graduated specialist nurseNurse practitionerPublic health nurseNurse student |
| Orientation program in hospital | Orientation program in specialized units such as the operating room, ICU, emergency department, etc. |
| Quasi ExperimentalPilot ProjectCohort Study | Opinion/DiscussionDissertation |
We employed an adapted PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) model; data selection proceeded through four stages. The keyword search in the five databases yielded 3025 studies. The first step is the identification of the studies from five databases; the second step is exclusion stage was based on the title (n=204); the third step is exclusion stage based on abstract (n=77); and the fourth is exclusion stage on overall content (n=14). This process is described in Fig. 1. The analysis was carried out specific to the orientation program for NGNs in the hospital using a narrative, descriptive method.
ResultsData search and selection was performed in fourteen studies corresponding to the inclusion criteria. The target samples from those studies were NGNs with sample sizes ranging from three to 521. One of the studies did not specify sample size, and reported only use of a total sampling method.8 All studies covered implementation of an orientation program either developed by the study authors or based on existing theory and then assessed the results thereof. Research designs varied, and included pilot project,9–13 quasi-experimental,14,15 mixed method,8,16 non-experimental mixed method,17 cohort,18–20 and quasi-experimental pre-test/post-test.15
Orientation program lengths ranged from six days to one year; one study did not report the length of the orientation program investigated.10 Activities in these orientation programs included preceptorship9–11,13–18,20,21; class-based activities8–10,12,13,18,21; laboratory simulations10,12,13,18,21; patient care simulations8,11,13–16,18,19,21; bedside learning8; and clinical practice days.10,16 Preceptorship and mentorship programs were carried out according to existing practice and modifications introduced by the given preceptor or mentor. One of the studies detailed collaboration with retired nurses referred to as VNAs (volunteer nurse ambassadors) to act as additional mentors for the NGNs.12 Another described the implementation of pathway orientation to help NGNs and their preceptor begin the preceptorship prior to the commencement of the orientation period.10
Class activities such as sharing journal assignments,11,16,21 peer group discussions,19 role-playing,21 and review of materials provided by the hospital were parts of the orientations investigated for this review. Basic orientation courses included human resources and nursing policies,10,17 environmental and safety culture,10,11,16 infection control,10 emergency procedures,10 conflict resolution,18 incident reporting,18 stress management,18 professional development,20,21 service excellence,16 ethics, quality,16 patient rights,16 and communication.16
Learning materials were provided regarding the end of life care,20 therapy and blood transfusion policies,10 use of medical equipment (such as fluid pumps),10 human organ systems and their relevant departments (e.g., cardiology, respiratory, neurology, hepatobiliary),11 sepsis,11 and trauma.11 New technologies were implemented into certain orientation programs, including a human patient simulator called Laerdal Sim-Man®,15 computer-based learning,12,19 and online materials.8
A variety of measuring tools were used to evaluate the orientation programs, including the Advisory Board's Critical Thinking Diagnostic,11 the New Graduated Nurse Learning Behavior Rating Guide14, the Casey-Fink Graduate Nurse Experience Survey,8,9,17,18,20,21 the Health Sciences Reasoning Test™ (HSRT), the Clinical Decision-Making in Nursing Scale (CDMNS),15 and the Halfer-Graf Job/Work Environment Nursing Satisfaction Survey.16 Certain studies employed instruments designed by the investigators to evaluate the orientation programs. Aspects evaluated were wide-ranging, including satisfaction,9,10,14,16,17 cost savings,10,13,18,19 time effectiveness,10,19 critical thinking,11,15 retention and turnover,9,12,14,16–21 performance,14 effectiveness,8,19 confidence,17,21 and engagement (Table 3).9,16,17
Description of included studies.
| No | Author/year | Method | Sample | Measurement tool | Length of orientation | Program | Result |
|---|---|---|---|---|---|---|---|
| 1 | Allen/2011 | Pilot project | 60 | A self-designed tool | • 8hours for basic hospital orientation• 8hours for nursing orientation• 4hours for clinical lab• Continue with preceptorship (not stated) | • Preceptor• Orientation pathway• Basic hospital orientation• Nursing policies• Clinical lab | Satisfaction: increase 1%Cost saving: $62,000Time-effectiveness: complete one week earlier |
| 2 | Bittner/2016 | Pilot project | 24 | Advisory Board's Critical Thinking Diagnostic | 400hours | • Simulation• Learning activities• Reflective journaling• FGD• Preceptorship | Critical thinking: improved at 6 and 12 months interval |
| 3 | Roche/2013 | Quasi experimental pilot study | 24 | New Graduated Nurse Learning Behavior Rating Guide | Five weeks | HPS simulation case for the intervention groupPreceptorship for both group | Satisfaction: 4.25 (Likert scale 1–5)Retention: all participant still employed one year after hirePerformance: no significant differences between intervention and control group |
| 4 | Rush/2013 | Mixed methods study | Not stated | • Casey-Fink Graduate Nurse Experience Survey• Orientation to the employer/nursing unit• General transition• The specific new graduate nurse transition program | One year | • Written materials• Classroom/theory• Simulation/theory• Hands-on/bedside learning• In service programs/workshops• Website/online materials | Helpfulness: 57.6% |
| 5 | Maneval/2012 | Quasi-experimental: Pretest–posttest design | 26 | Health Sciences Reasoning Test™ (HSRT) and the Clinical Decision-Making in Nursing Scale (CDMNS) | Ten weeks | • Experimental: Standard new nurse orientation, and six high-fidelity patient simulation experiences with the Laerdal Sim-Man®, a fidelity human patient simulator.• Control: Standard new nurse orientation• Preceptorship for both group | Critical thinking: pretest score of 20.92 (SD=3.43) compared with a mean posttest score of 21.89 (SD=2.52) |
| 6 | Hillman/2011 | Cohort | 251 | Casey-Fink Graduate Nurse Experience Survey | 16 weeks | • Centralized class day• Unit-specific class day• Preceptorship• Simulation lab | Retention: 100%Cost saving: 4 million dollarHelpfulness: Yes |
| 7 | Murphy/2017 | Cohort | 521 | A self-designed tool | 6 days | • Corporate orientation• Computer training• Experiential learning | Turnover: 12.28%Cost saving: $156,000Time-effectiveness: shortened 8hours/day |
| 8 | Olson-Sitki/2012 | Non-experimental mix method design | 31 | Casey-Fink Graduate Nurse Experience Survey | Three months | • New employee onboarding and central nursing orientation• Unit-based orientation• The nurse residency program | Confidence: increase in 12 monthsSatisfaction: overall yesEngagement: highly engaged |
| 9 | Phillips/2014 | Quasi-experimental | 4 | Casey-Fink Graduate Nurse Experience Survey | 12 months | • Graduate Nurse• Internship Program (GNIP)• Preceptorship• Adult learning | Competency: improve at 6 and 12 monthsRetention: 11.5% better than control group |
| 10 | Anderson/2009 | Mix qualitative-quantitative | 90 | Halfer-Graf tool/Work Environment Nursing Satisfaction Survey | One year | • Interactive Nurse Residency• Preceptorship• Peers | Satisfaction: yesEngagement: yes |
| 11 | Baldwin/2016 | Pilot project | 3 | A self-designed tool | 18 weeks followed mentoring for one year | VNA (volunteered nurse ambassador) from a retired nurse | Retention: 100% |
| 12 | Horwarth/2016 | Pilot project | 5 | A self-designed tool | Eight weeks | • A Collaborative Model• Preceptorship• Simulation | Cost saving: over $19,000 |
| 13 | Kowalski/2010 | Cohort | 55 | • A self-designed tool• Pagana's clinical stress questionnaire• Spielberge's state-trait anxiety inventory• Casey-Fink Graduate Nurse Experience Survey | One year | • Nurse Residency Program• Preceptorship | Retention: 78% |
| 14 | Maxwell/2014 | Cohort | 18 | • Casey-Fink Graduate Nurse Experience Survey• Graduate nurse residency program evaluation | One year | • UHC/AACN New Graduate• Nurse Residency Program• Preceptorship | Engagement: yesSatisfaction: yesRetention: before 40%, after 100% |
Orientation time given to NGNs is a critical feature for analysis, as the length thereof can affect costs incurred and results derived from the program. The shortest orientation time in the study was six days, while the longest was twelve months. Comprehensive orientation processes correlated significantly to the length of orientation22; research suggests that the NGN orientation period should be at least four weeks long.23 All articles reviewed for this study met this guideline except for one, wherein the period was six days.19
Most researchers reported a support system comprised of a preceptor, classes, and simulations. Although the role of the preceptor is challenging, many studies suggested that a successful preceptorship can increase NGN job satisfaction and retention of NGNs leading to decreased turnover.24 One successful support system included mentoring by a VNA; NGNs reported high rates of satisfaction with the program.12 In this system, retired nurses are recruited to shadow the NGNs while they provide nursing care to their patients. In addition to good mentorship, classes and simulations are also an essential part of the orientation process to provide a safe and productive learning environment. Research shows that simulations of common clinical events in a group setting help NGNs to develop clinical reasoning and decision making skills.25
Classroom materials could be categorized into hospital and nursing policies, anatomical and physiological systems reviews, and international accreditation standards, with the goal of bringing theory into practice. Studies have intimated that NGNs feel underprepared for practice because expectations of registered nurses are much greater than those of students, prioritization of care is difficult to put into practice, and the workload can impede focus.26 Classroom materials detailing the human body systems as they relate to clinical practice help NGNs connect their education to real-life situations. Specific information about standards of accreditation and hospital nursing policies help NGNs to better assimilate into the hospital culture. Education about safety, quality improvement, patient-centered care, communication, and teamwork, all included in the standard of accreditation, resulted in fewer reported patient care errors, and fewer unsafe practices.27
All orientation programs in all studies examined for this review reported positive impacts such as increased retention and reduced turnover, and increased job satisfaction among NGNs during their transition phase. Research shows that the orientation program is essential to NGN job satisfaction and increased retention rates.28 Other studies report other positive effects of orientation, to include better support, improved socialization, and a positive clinical learning environment.29 Established orientation programs were associated with higher retention rates, higher competency levels, better job satisfaction, and lower stress levels.27 Orientation geared toward improved competency can also build good perceptions of interpersonal (72.4%), technical (53.4%), and critical thinking skills (58.6%) in newly hired nurses.30
In addition to planning activities carried out during orientation, it is important for the hospital to establish specific objectives for the orientation program. Determining goals can be done together by the preceptor and NGNs in the form of orientation pathways.10 In a pathway, the objectives and means by which goals can be achieved during the orientation process are written down. This is done so that the NGNs and preceptors can remain focused on the objectives that must be achieved. It is also essential to evaluate orientation activities during the orientation process, by comparing results with stated objectives. Hospitals can design their evaluation instruments or use one that is already available. In studies analyzed for this review, four of the fourteen studies used the Casey-Fink Graduate Nurse Experience Survey in the evaluation process.8,9,17,18,20,21 Instruments that have been tested for validity and reliability can help to ensure usable data.
ConclusionNursing managers should design and manage orientation programs aligned with evidence-based research. Modifications can be made as necessary with regards to the hospital's available budget and existing technology. Orientation length should be determined in accordance with orientation goals and activities. Components of a successful orientation program are learning materials, support systems, and learning methods with proven efficacy. Nursing managers must also design measurable goals for the program and NGNs to enable evaluations in real time of orientation programs so managers can make continuous improvements to existing systems.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by Hibah PITTA 2018 funded by Directorate of Research and Community Services Universitas Indonesia No. 5578/UN2.R3.1/HKP.05.00/2018.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.