This study aimed to assess the relationship between knowledge of antiretroviral therapy (ART) and stigma regarding adherence to ART.
MethodThis cross-sectional study used a purposive sampling technique and involved 175 men who have sex with men (MSM), all of whom have HIV/AIDS. Levels of knowledge, stigma, and adherence were measured using the ART knowledge instrument, the Berger HIV Stigma Scale, and the Medication Adherence Questionnaire (MAQ), respectively.
ResultsMost of the respondents had a high level of ART knowledge (76.6%), HIV-related stigma (51.4%), and non-adherence to ART (52%). The study showed a statistically significant negative correlation between stigma and adherence to ART (p=0.043; α=0.05). In addition, ART knowledge correlated positively with adherence to ART (p=0.010; α=0.05). Regression analysis showed that ART knowledge is an important factor influencing ART adherence (OR=2.817).
ConclusionsIt was found that as the level of ART knowledge increased, self-motivation and attitudes toward adherence to treatment increased.
People who have been infected with Human Immunodeficiency Virus (HIV) may often be asymptomatic initially. However, if the condition is left untreated, most of those infected with HIV go on to develop acquired immune deficiency syndrome (AIDS). Since 1996, considerable progress has been made with antiretroviral (ARV) drugs, which can lengthen the duration between HIV infection and AIDS diagnosis.1
Worldwide epidemiological data on HIV/AIDS showed that the number of people living with HIV/AIDS (PLWHA) in 2016 had reached 36.7 million, with a total of 1.8 million new infections. The number of deaths from AIDS remained high, at 1.1 million. However, while the global rate of deaths from AIDS is declining due to the use of antiretroviral therapy, this reduction is still far from the target. In the Asia-Pacific region, antiretroviral therapy (ART) availability reduced AIDS deaths by an estimated 240,000 in 2010 to 170,000 in 2016. While new infections from AIDS declined by 52% in Myanmar during this period, they increased in Indonesia by 68%. In the Asia-Pacific region, Indonesia is ranked third for new HIV infections after India and China.2
Men who have sex with men (MSM) accounted for 13% of new HIV infections globally in 2015. Based on the risk factors, MSM is 24 times more likely to be HIV-positive than the rest of the population.3 It is predicted that in 2020, the number of new HIV infections in the MSM group will increase by 42% according to the UN Commission on AIDS in Asia. Further data from 2012 to 2016 showed an increase of 25.8% HIV-positive cases among MSM in Indonesia.4 This places MSM second in terms of risk factors after heterosexuals.5 Medan is the capital of North Sumatra province in Indonesia and is one of the country's largest metropolitan areas; according to data from the Public Health Office in Medan, 46.34% of the PLWHA are homosexuals. This makes the risk of HIV transmission greater.
The administration of ART is aimed to reducing morbidity and mortality rates and improving quality of life for PLWHA.6 However, missed doses of ARV drugs may ultimately lead to non-adherence to treatment.7 Although the rate of ART users is increasing, adherence to therapy has become an important issue, since non-adherence to the medication can cause resistance to the virus. It is possible that the problem of non-adherence may also be influenced by a low level of knowledge about ART. In previous studies, particular beliefs about therapy might prevent PLWHA from being positive about treatment, which may, in turn, affect their adherence to ART. When questioned, 33% of the respondents were unsure of their HIV status and thought that ARV drugs were not necessary, while 34.9% of the respondents believed that lifelong ARV drug use weakened the body.8
The stigma encountered by MSM groups often leads to internal stigma, feelings of doubt, and self-loathing.9 Internal stigma may cause psychological disorders such as depression, which may then affect adherence.10 The stigma generally associated with perceived high-risk sexual behavior in MSM often prevents those at risk from undertaking HIV testing, counseling, and other preventive care.11 Among those who experience the effects of stigma, 32% are less likely to adhere properly to ART. However, adherence to ART is vital for the successful treatment of PLWHA.12 Thus, there is a need to understand the relationship between knowledge of ART and stigma about adherence to ART among people in the MSM group living with HIV/AIDS (PLWHA MSM), so that appropriate intervention can be introduced.
MethodStudy design and settingThis cross-sectional study used a purposive sampling technique and was conducted in Central General Hospital H. Adam Malik, Pirngadi Hospital, Teladan Public Health Center, and Padang Bulan Public Health Center in Medan, Indonesia. The study duration was from May to June 2018, and study settings were selected from among government-owned health facilities with voluntary counseling and testing services.
Data collectionEligible respondents included PLWHA MSM aged >18 years who were receiving ART. There were a total of 175 respondents. Informed consent was written in Indonesian, and the instruments used were ART knowledge, the Berger HIV Stigma Scale, and the Medication Adherence Questionnaire (MAQ).13,14 The questionnaires were reviewed by experts using the back-translation method and were eligible for validity and reliability tests. Cronbach's alpha was used to obtain ART knowledge (α=0.56). Stigma was measured using the HIV Berger Stigma Scale, which was already translated into Indonesian, along with Cronbach's alpha (α=0.94). Validity and reliability tests were performed on the MAQ using Cronbach's alpha (α=0.66), and the data were analyzed using statistical software. Relationship analyses on knowledge of ART and stigma regarding adherence to ART were carried out using the Chi-square and Mann–Whitney U tests. Logistic regression analysis was also performed in this study.
Ethical considerationEthical approval was obtained from the ethics committee of the Faculty of Nursing Universitas Indonesia with the approval number 156/UN2.F12.D/HKP.02.04/2018. Written consent was obtained from the respondents before they filled out the questionnaires. To safeguard their privacy, each respondent filled out the questionnaires in a private room.
ResultsRespondents’ characteristicsTable 1 shows the characteristics of the respondents. The average age of the PLWH MSM in the study was 29.39 years, which is typically an active period of sexual activity with partners in MSM groups. Risky sexual behavior is likely to increase the level of HIV among this group. The majority of the respondents were found to have a high level of education who had attended senior high school or college. The higher level of education suggests better ability to access information about the disease, treatment of the disease, and related health services. However, respondents who have a job were found to have a low income based on North Sumatra's Provincial Minimum Wage (PMW).
Characteristics of the respondents.
| Variable | Mean | SD |
|---|---|---|
| Age | 29.39 | 6.459 |
| Length of diagnosis | 19.10 | 15.923 |
| Duration of ART | 17.99 | 15.897 |
| n | % | |
|---|---|---|
| Education | ||
| Elementary | 2 | 1.1 |
| Junior high | 6 | 3.4 |
| Senior high | 103 | 58.9 |
| College | 64 | 36.6 |
| Occupation | ||
| Unemployed | 14 | 8 |
| Employed | 161 | 92 |
| Income (acc. to PMW North Sumatera) | ||
| Low | 89 | 50.9 |
| High | 86 | 49.1 |
| Adherence to ART | ||
| Yes | 84 | 48 |
| No | 91 | 52 |
| ART knowledge | ||
| High | 134 | 76.6 |
| Low | 41 | 23.4 |
| Stigma | ||
| Low | 85 | 48.6 |
| High | 90 | 51.4 |
Factors significantly associated with adherence to ART were ART knowledge (p<0.010; OR=2.817) and stigma (p<0.043; OR=0.510). Knowledge of ART and stigma were the most influential factors in regression modeling. Knowledge of ART became the dominant factor after analyzing all variables. People with a high knowledge of ART were 2.817 times more likely to adhere to treatment. Most respondents with high adherence to ART had high ART knowledge and low stigma (Table 2).
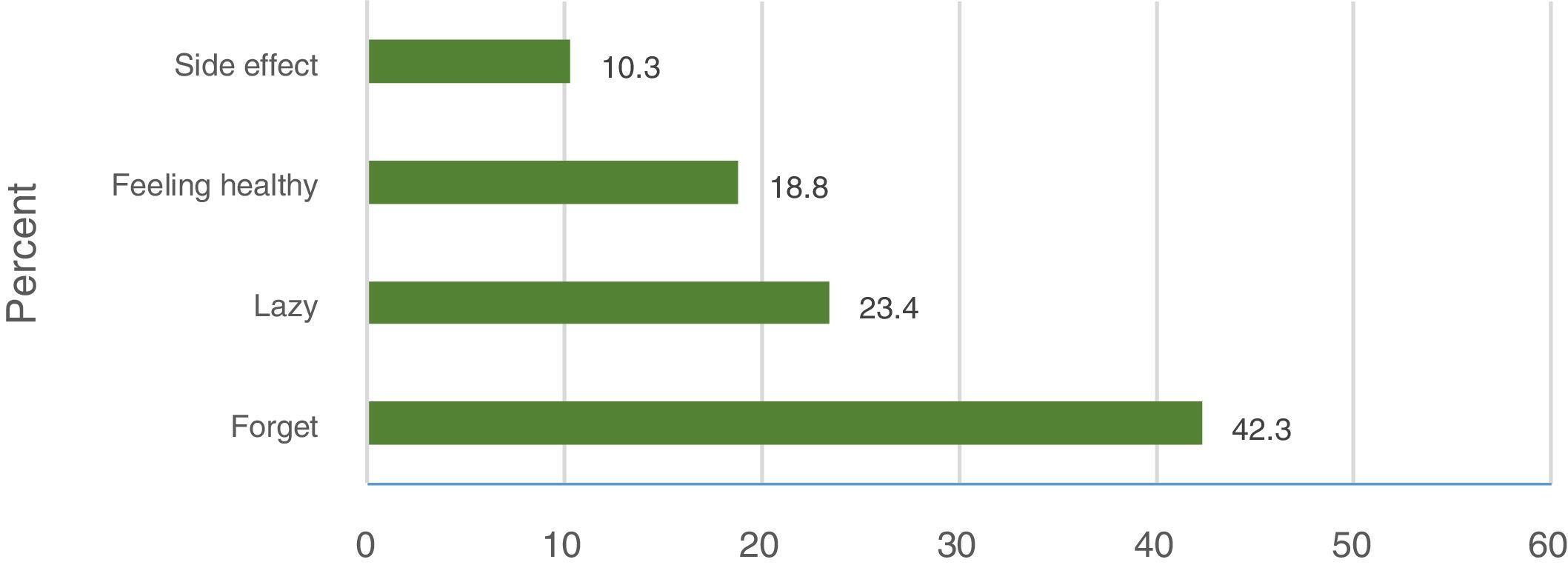
Non-adherence to ARTNon-adherence to ART had various causes (Fig. 1). Mostly, the patients forgot to take the medication due to work or sleep. Non-adherence also occurred because respondents were too lazy to take medicine. They became bored with taking medicine once or twice a day and being on treatment for months or years. Respondents who felt better and had low ART knowledge may have stopped treatment without notice. In the beginning, side effects were estimated to be the most frequent reason for non-adherence. Side effects of ART may cause non-adherence, but as the respondents are informed of these effects from the start, this does not become a major barrier.
DiscussionAdherence to ART was assessed from self-reports in the previous month. Based on the results, 52% of respondents did not adhere to ART. This result is the same as a previous study which also showed high non-adherence to ART.15 It is also supported by previous studies which showed that MSM are 0.6 times less likely to adhere to ART than other groups.16 In this study, the most common reason for non-adherence forgot to take medicine. This was similar to other studies which found that forgetting was the most likely reason for non-adherence, known as unintentional non-adherence.17–19
No demographic data were found to be significantly correlated with adherence to ART. In contrast to previous studies, there was no significant association between length of ART and ART adherence.20,21 Conceptually, it has been mentioned that the longer the treatment, the more difficult to patients maintaining adherence and following treatment advice.20 This finding concludes that the length of ART is no longer linear with ART adherence if patients continue to have routine counseling or still have a short length of diagnoses.
ART knowledge significantly associated with adherence to ART. These results are consistent with previous studies.22,23 In multivariate modeling, ART knowledge remained a factor associated with adherence to ART and became the most dominant factor after analyzing other confounding factors (OR=2.817). This result is similar to previous studies, which stated that the dominant factor associated with adherence to ART was knowledge because higher ART knowledge stimulated better self-motivation and attitude toward adherence to treatment.24–26
Stigma showed a significant relationship with adherence to ART. These results are similar to previous studies that showed a negative association between these variables.27,28 Respondents with low stigma were more likely to have good adherence, while respondents with high stigma were more likely to have non-adherence. These results are consistent with previous studies which showed cross-tabulations of stigma and discrimination against adherence to ART and determined that respondents with low stigma and discrimination had good adherence.29
A double stigma in MSM has negatively established internalizations of stigma and shame.9 Stigma about HIV reduces the urge of individuals to access health services and makes them more likely to conceal their status.30 Stigma may become a barrier that prevents respondents from visiting health services and results in non-adherence to treatment. This stigma is related to the fear of HIV status becoming public knowledge when the patient takes ARV drugs or visits a health care facility.
PLWHA MSM has unique characteristics compared with the other groups. However, this study also has some limitations. ART adherence was measured only by a self-reported questionnaire. Other limitations are that only patients who received health services were included in this study. Simple random sampling would be a better technique, but it could not be applied because this study was conducted during the month of Ramadhan. Many respondents did not visit health services facilities or requested two months of ARV drugs during that period.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by Hibah PITTA 2018 funded by DPRM Universitas Indonesia No. 1830/UN2.R3.1/HKP.05.00/2018.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.