We present the case of a 75-year-old male, resident in a rural area in southern Andalusia, who came to the Dermatology department with a six-month history of a persistent painless ulcer on his penis. He denied risky sexual behaviour. He had no fever, weight loss or other systemic symptoms. After the ulcer appeared, he was prescribed various topical treatments, including corticosteroids, antifungals and antibiotics for 6-8 weeks, without improvement. His medical history included a circumcision performed by the Urology department in 2021 due to lesions suggestive of candidiasis.
On physical examination, a 3×1-cm ulcer with raised edges was seen on the dorsal aspect of the patient’s penis (Fig. 1). No inguinal lymphadenopathy could be palpated. No other skin or mucosal lesions were detected. Blood tests were performed, which revealed monoclonal IgM lambda hypergammaglobulinaemia. Liver function tests were normal. VDRL, HIV, HCV and HSV serology tests were negative. There was evidence of a past HBV infection. As squamous cell carcinoma was initially suspected, a biopsy was performed.
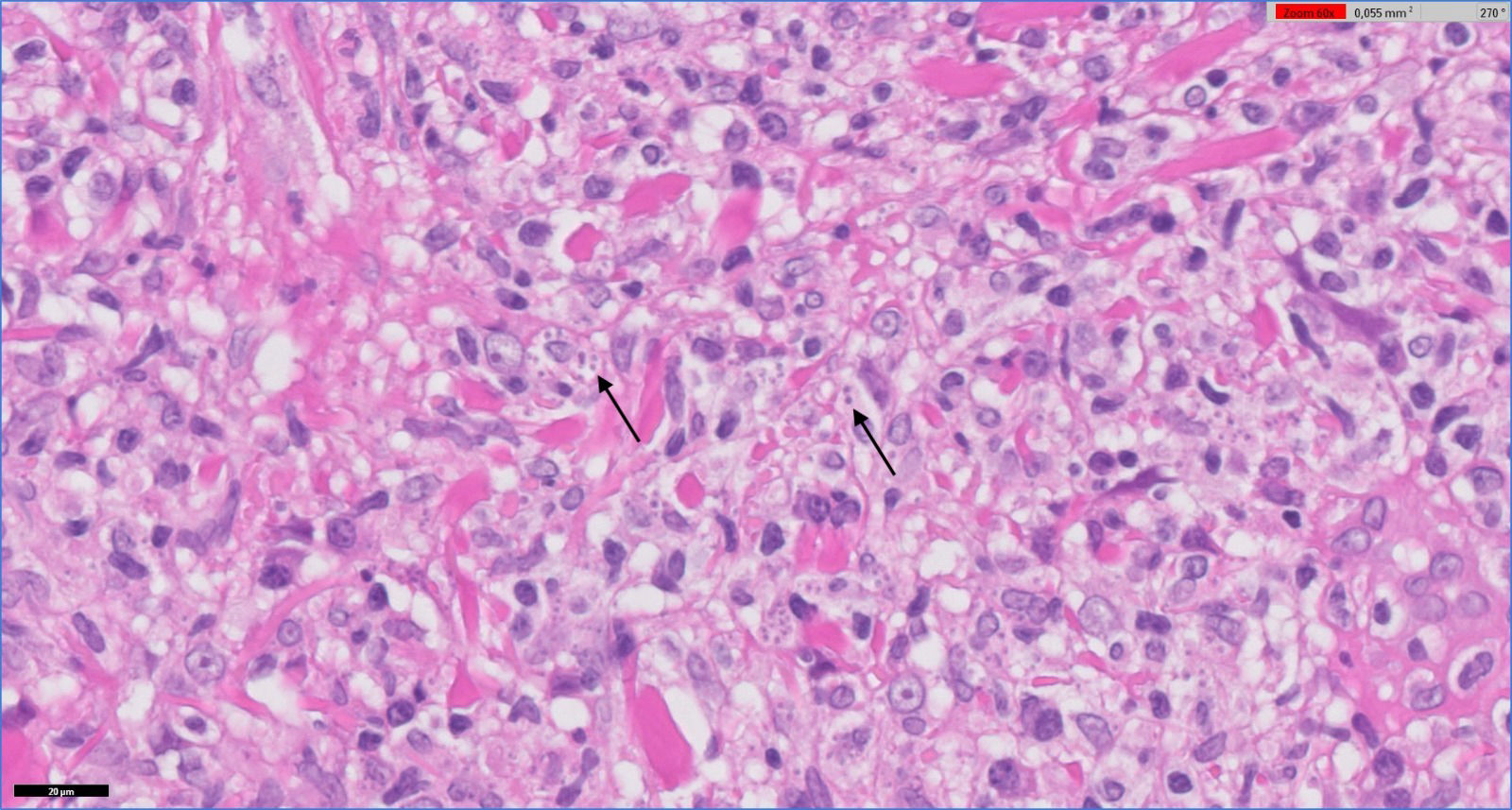
Clinical course and diagnosisHistopathological analysis confirmed ulcerated lymphohistiocytic dermatitis of the foreskin (balanoposthitis) with a marked plasma cell component, secondary to active Leishmania infection (Fig. 2). PCR of the leishmania genome was positive. To type the Leishmania species (most likely infantum), it was necessary to extract DNA from the remaining sample and send it to a reference centre. Given the urgency of starting treatment, it was decided not to wait for the results of the exact typing.
In a case conference with the Infectious Diseases Department, it was decided to treat the patient as visceral leishmaniasis, given the time since onset and risk of spread, with intravenous liposomal amphotericin B at a dose of 5mg/kg on days 1, 5, and 10 (total dose 15mg/kg),1 according to the protocol used in the hospital. The patient responded well, with no evidence of recurrence at the six-month follow-up.
Leishmaniasis is a tropical infectious disease caused by protozoan parasites of the genus Leishmania, transmitted by the bite of infected sandflies. The ability of these parasites to evade the human immune system and reside in macrophages, coupled with the clinical variability of the disease, poses significant challenges for diagnosis and treatment. Genital leishmaniasis is a rare clinical condition compared to other forms of the disease. It has been reported in various tropical and subtropical regions, including Latin America, Africa, the Middle East and Asia.2 Genital lesions may appear near sandfly bites or be the result of the infection spreading through the bloodstream. Conditions such as disseminated cutaneous leishmaniasis and HIV infection may be associated with genital involvement.3 Our patient had no immunosuppression or other recognised risk factors associated with atypical presentations.
Symptoms of genital leishmaniasis are variable, although they generally include persistent genital ulcers, nodular lesions and inguinal lymphadenopathy. These manifestations can be confused with other sexually transmitted infections or genital cancers, which often leads to a late diagnosis,3 as in the case we have reported here.
According to WHO guidelines,1 the treatment of cutaneous leishmaniasis (CL) caused by Leishmania infantum depends on the severity of the disease and the patient’s comorbidities. For mild disease (fewer than four lesions, each less than 4cm in size, non-immunocompromised patients), treatment includes wound care with dressings, cleansing with disinfectants, intralesional antimonials or superficial cryotherapy, and ointments containing paromomycin. Moderate disease (up to four lesions, each less than 4cm in size, in potentially disfiguring areas) is treated with a combination of superficial cryotherapy and intralesional antimonials, or antimonials alone if cryotherapy equipment is not available, with thermotherapy as an alternative method. Severe disease (lesions larger than 4cm in size, more than four lesions, periorificial or near small joints, significant lymphatic spread, immunosuppression or severe comorbidities) requires systemic treatment with intramuscular or intravenous pentavalent antimonials (20mg Sb5+/kg for 10–20 days) or miltefosine (50mg three times daily for 28 days). Early and appropriate treatment is essential to reduce morbidity and prevent serious complications.
Sources of fundingThere was no funding for this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Informed consentConsent was obtained for publication of all patient photographs and medical information.
AI usage statementDuring the preparation of this article, the authors used ChatGPT-4 (OpenAI, California, USA), with human review to improve the writing. After using this tool, the authors reviewed and edited the contents where necessary and declare themselves responsible for the content of this publication.
Data availability statementData supporting these findings are available on reasonable request from the corresponding author. The corresponding author had full access to all the data in this manuscript and takes responsibility for its integrity.