This was a 39-year-old male patient with no comorbidities or relevant medical history who attended the Accident and Emergency department with odynophagia and fever for three days. He had previously consulted his primary care physician, who had prescribed symptomatic treatment. No rapid test was performed. The physical examination showed bilateral pharyngeal–tonsillar exudate, bilateral lateral-cervical lymphadenopathy, and in the right lower limb, greater consistency was evident in the abductor, with an extension of 10cm in maximum diameter, which contributed to an increase in the perimeter with respect to the other limb. There was no history of trauma, nor did he report pain in the limb. A group A streptococcus rapid antigen test was performed with a positive result.
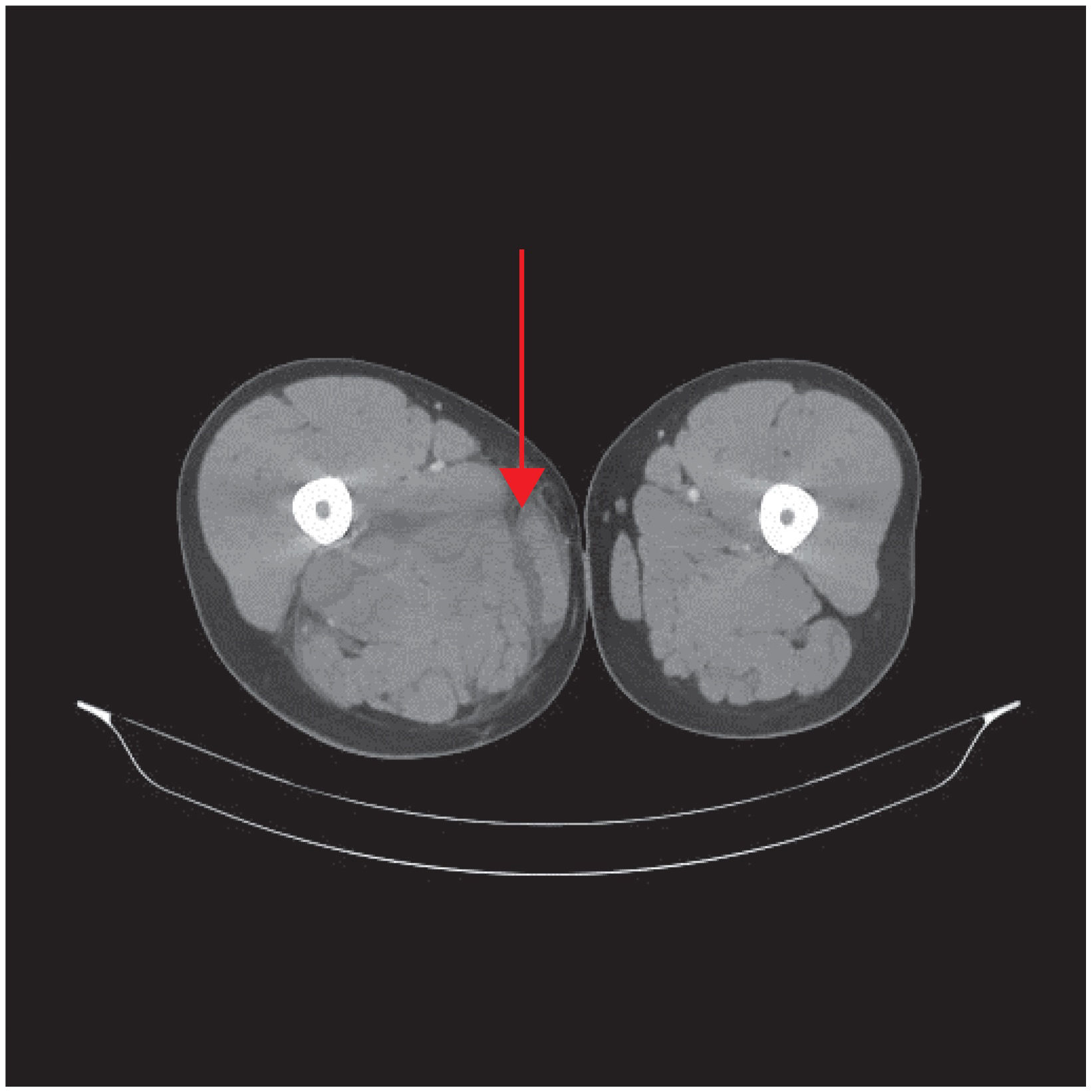
Clinical course and diagnosisVital signs: blood pressure 98/78, heart rate 110bpm, temperature 36.7°C. Bloods: leucocytes 21.4×103/μl, CRP 18mg/dl, lactic acid 5.9mmol/l, prothrombin activity 55%, procalcitonin 4.98ng/ml, CK 842IU/l. The chest-abdomen-limb computed tomography (CT) was reported as packing and fluid layers surrounding the right pectineus muscle, extending to the beginning of the adductor muscles and into the quadratus femoris. Hypodensity, extending caudally and affecting the internal rectus muscles, biceps in the anterior short head and long head, semimembranosus and semitendinosus muscles. Layers of fluid and trabeculation of intermuscular fat to the popliteal fossa (Fig. 1).
Blood cultures were obtained, and the patient was prescribed meropenem, linezolid and volume (30ml/kg) in the first three hours; no vasopressors were required due to mean arterial pressure. >65mmHg and diuresis greater than 0.5ml/kg/h. Within less than three hours, limb drainage was performed, with the release of cloudy, non-malodorous amber fluid and extensive debridement of all muscle groups, with loss of colour. The surgical wound was left open.
After admission to the ICU, the patient required noradrenaline, dopamine and continuous venovenous haemodiafiltration. Streptococcus pyogenes was isolated in the cultures of the pharyngeal swab, muscle biopsy and blood samples. The strain was sensitive to penicillin, clindamycin, erythromycin and tetracycline. Two isolates from different locations (pharyngeal exudate and muscle biopsy) were sent to Spain’s National Microbiology Centre (Majadahonda, Madrid), and were characterised as serotype M89, speB, speC, speF, speG, speH, speJ. The pathology examination showed necrosis of the superficial muscular fascia, with polymorphonuclear infiltration and the presence of microorganisms. Clindamycin (due to its antitoxin effect) was added to the treatment with the diagnosis of streptococcal toxic shock syndrome (STSS) associated with necrotising fasciitis. Transoesophageal echocardiogram showed no signs of endocarditis. Twenty-four hours later, the patient went into refractory shock, despite treatment with terlipressin, and then asystole, which did not respond to attempts at resuscitation.
In December 2022, the WHO reported an increase in the incidence of invasive infections due to Streptococcus pyogenes or group A β-haemolytic streptococcus (iGAS), with cases in Europe and the United States.1 The prevalence of these invasive forms is established in two cases per 100,000 population, and of them, 12% are complicated by STSS, with a mortality rate as high as 84%.2
Although there are networks in different countries that monitor the incidence of iGAS, the studies do not determine the reasons for the aggressive resurgence. No relationship has been found with classic factors such as socioeconomic conditions and lack of medical care. In Spain, in 2022, the PedGAS-net (multicentre network for studying iGAS in patients ≤16 years old) warned of a significant increase in iGAS cases, and it was speculated that this could be related to the lack of exposure to respiratory pathogens in children due to their social isolation during the pandemic.3
Although great efforts have been made to understand and determine the virulence factors, all that has been found so far is a certain association with certain serotypes which produce M protein, toxin production and expression of the capsular polysaccharide. However, taking into account that there have been no reports of either an increase in antibiotic resistance or a new type of the emm gene sequence (associated with the production of M protein and responsible for the most invasive forms), the WHO currently considers that the risk of iGAS for the general population is low.1
Ethical considerationsInformed consent was obtained from the patient to use the images in accordance with the centre’s regulations. The ethical standards established in the Declaration of Helsinki and its later amendments or comparable standards have been respected.
FundingThis article did not require funding.
Conflicts of interestThere are no conflicts of interest.
This case is an example of multidisciplinary participation. Given the impossibility of mentioning all of them, we would like to highlight the participation of the Accident and Emergency, Intensive Care, Traumatology, Radiology, Microbiology, Haematology, Pathology and Cardiology departments, as well as the characterisation of the strains sent to Spain’s National Microbiology Centre.