Aspergillus infection is a significant cause of morbi-mortality in an at-risk population. The Study Group of Fungal Infections (GEMICOMED) from the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC) has reviewed announcements made in invasive aspergillosis management. We have organized our recommendations in such a way as to provide a guide in resolving different clinical situations concerning the entire spectrum of invasive diseases caused by Aspergillus in various populations. Diagnostic approach, treatment and preventions strategies are outlined. It is not our aim that these guidelines supplant clinical judgment with respect to specific patients; however, it is our objective to perform a comprehensive summary of quality of care evidence for invasive aspergillosis management in different settings.
Las infecciones causadas por Aspergillus causan una elevada morbimortalidad en la población susceptible. EL Grupo de Estudio de Micología Médica de la Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica (GEMICOMED/SEIMC) ha revisado las novedades más importantes sobre el manejo de las infecciones invasoras causadas por Aspergillus. Hemos organizado nuestras recomendaciones en 3 apartados: diagnóstico, tratamiento y profilaxis en diferentes grupos de pacientes susceptibles de padecer estas infecciones. Se revisan distintas situaciones clínicas que pueden estar causadas por este hongo. Nuestro objetivo no es que estas guías de tratamiento suplanten el juicio clínico de los médicos ante un determinado paciente; sin embargo, sí deseamos poder ofrecer un resumen comprensible sobre las evidencias que existen para realizar un óptimo manejo de la infección invasora causada por Aspergillus en diferentes situaciones clínicas.
The relationship between Aspergillus and the host ranges from saprophytic colonization to life-threatening infections, mainly affecting immunocompromised hosts. Advances in oncohematological patient care have increased long-term survival of such patients, and the new immunosuppressive drugs for different populations have lead to span the spectrum of populations at risk of this infection so the incidence of aspergillosis is expected to rise in next years. Consequently, physicians from different specialties face the challenge of treating these patients.
New diagnostic tools and treatment for this infection have been recently published. For that reason, and considering the relevance of the infections caused by Aspergillus, the Study Group of Fungal Infections (GEMICOMED) from the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC) has decided to perform a new document with the main objective to provide update recommendations on the management of aspergillosis. The guidelines have been divided into three sections: definitions and diagnostic, treatment, and prophylaxis of acute and chronic forms of invasive diseases caused by Aspergillus. These guidelines are addressed to professionals of infectious diseases specialists, microbiologist, hematologist, pediatricians and all other health professionals responsible of treating fungal infections. The 2018 revised recommendations for the management of these infections are summarized below. The whole document is available in the online version1 (Table 1).
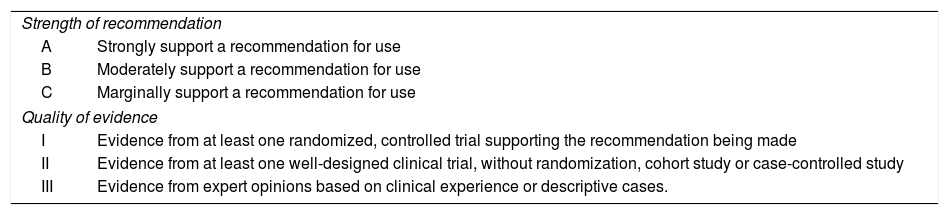
Definitions of strength of recommendation and quality of evidence.
| Strength of recommendation | |
| A | Strongly support a recommendation for use |
| B | Moderately support a recommendation for use |
| C | Marginally support a recommendation for use |
| Quality of evidence | |
| I | Evidence from at least one randomized, controlled trial supporting the recommendation being made |
| II | Evidence from at least one well-designed clinical trial, without randomization, cohort study or case-controlled study |
| III | Evidence from expert opinions based on clinical experience or descriptive cases. |
1. – What are the diseases caused byAspergillusand how is invasive pulmonary aspergillosis (IPA) defined?
Searched Keywords: Aspergillosis; Aspergillus; Invasive aspergillosis
Executive summary
- 1.
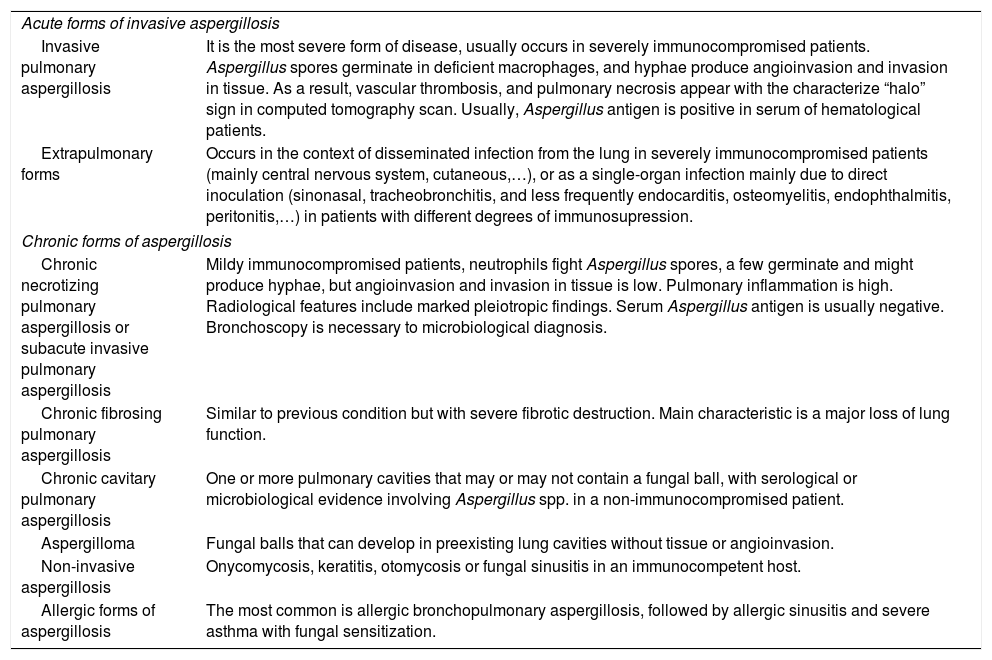
Different forms of aspergillosis have been described and associated with different clinical symptoms (See Table 2).
Table 2.Diseases caused by Aspergillus.
Acute forms of invasive aspergillosis Invasive pulmonary aspergillosis It is the most severe form of disease, usually occurs in severely immunocompromised patients. Aspergillus spores germinate in deficient macrophages, and hyphae produce angioinvasion and invasion in tissue. As a result, vascular thrombosis, and pulmonary necrosis appear with the characterize “halo” sign in computed tomography scan. Usually, Aspergillus antigen is positive in serum of hematological patients. Extrapulmonary forms Occurs in the context of disseminated infection from the lung in severely immunocompromised patients (mainly central nervous system, cutaneous,…), or as a single-organ infection mainly due to direct inoculation (sinonasal, tracheobronchitis, and less frequently endocarditis, osteomyelitis, endophthalmitis, peritonitis,…) in patients with different degrees of immunosupression. Chronic forms of aspergillosis Chronic necrotizing pulmonary aspergillosis or subacute invasive pulmonary aspergillosis Mildy immunocompromised patients, neutrophils fight Aspergillus spores, a few germinate and might produce hyphae, but angioinvasion and invasion in tissue is low. Pulmonary inflammation is high. Radiological features include marked pleiotropic findings. Serum Aspergillus antigen is usually negative. Bronchoscopy is necessary to microbiological diagnosis. Chronic fibrosing pulmonary aspergillosis Similar to previous condition but with severe fibrotic destruction. Main characteristic is a major loss of lung function. Chronic cavitary pulmonary aspergillosis One or more pulmonary cavities that may or may not contain a fungal ball, with serological or microbiological evidence involving Aspergillus spp. in a non-immunocompromised patient. Aspergilloma Fungal balls that can develop in preexisting lung cavities without tissue or angioinvasion. Non-invasive aspergillosis Onycomycosis, keratitis, otomycosis or fungal sinusitis in an immunocompetent host. Allergic forms of aspergillosis The most common is allergic bronchopulmonary aspergillosis, followed by allergic sinusitis and severe asthma with fungal sensitization. - 2.
Invasive pulmonary aspergillosis (IPA) is a systemic infection caused by Aspergillus that occurs in immunocompromised patients. It is the most severe form of aspergillosis.
2. – What microbiological methods can be used to diagnose invasive aspergillosis (IA)? Are all diagnostic methods useful in all populations?
Searched Keywords: Diagnosis; Aspergillosis; Aspergillus diagnostic tests; Galactomannan; Glucan; BDG; Aspergillus LFD; Aspergillus PCR.
Executive summary
- 1.
Diagnosis of IA in patients with suspected infection is mainly based on culture (AI), galactomannan antigen quantification (GM) (AII) and techniques based on the amplification of fungal DNA by the polymerase chain reaction (PCR) (AII).
- 2.
Sensitivity of cultures is usually low but provides information on epidemiology and antifungal susceptibility (AII).
- 3.
GM serum quantification is recommended in neutropenic and hematological patients who are not in prophylaxis (AII).
- 4.
The PCR-based techniques have been extensively used and might improve diagnosis in hematological and ICU patients (AII) albeit an effort in standardization and harmonization of the techniques is still needed.
3. – What is the recommended diagnostic approach for patients with suspicion of IA…
a) …in oncogical and hematological patients?
Searched Keywords: Invasive Aspergillosis; Oncologic patients; Haematologic patients; Neutropenia; Diagnostic.
Executive summary
- 1.
1. – In neutropenic patients with suspicion of IPA the recommended approach is: (a) chest computed tomography (CT) scan (AII), (b) serum and/or BAL GM detection (AII), and (c) bronchoscopy (AII). Bronchoscopy allows for performing fungal culture, GM and PCR determinations that increase the probability of ruling in IPA diagnosis and ruling out other infections (AI).
- 2.
2. – Histopathologic examination of tissues and fluid specimens are recommended whenever possible (AI), particularly to rule out other infections or diseases in patients with pulmonary nodules and negative biomarkers results (BII).
- 3.
3. – For oncologic, non-neutropenic patients, specially those with solid lung tumors or pulmonary metastatic disease in whom chronic form of aspergillosis would be rule out, the recommended approach is: (a) to take into account nonspecific clinical presentation, (b) chest CT scan, and (c) bronchoscopy with fungal culture and BAL GM detection (AIII).
b) …in solid organ transplantation (SOT)?
Searched Keywords: Aspergillosis; Diagnosis; Non-neutropenic; SOT (lung; renal; kidney; liver; intestinal).
Executive summary
- 1.
Bronchoscopy plays a key role to approach IA diagnosis. Check visual images on bronchoscopy, BAL fungal culture and GM in BAL are strong recommended (AII).
- 2.
CT scan has a limited value as most of the classic radiological findings are rarely found in these patients (BII).
- 3.
Serum GM detection has less sensitivity than in BAL (BIII).
c) …in patients receiving mold antifungal prophylaxis?
Searched Keywords: Aspergillosis; Diagnosis antifungal prophylaxis; Breakthrough fungal infection.
Executive summary
- 1.
The following investigation (some combined or all as clinically indicated) has suggested: CT scanning (AIII), bronchoscopy with culture, GM and PCR on BAL fluid (AIII).
- 2.
The use of serum GM or PCR is not recommended in patients receiving antifungal prophylaxis (BII).
- 3.
If any abnormality is detected on CT scan and all microbiologic tools are negative, biopsy is recommended for IA diagnosis and ruling out other diseases (AIII).
d)…in intensive care unit (ICU) patients?
Searched Keywords: IA; Diagnostic approach for IA; ICU patients.
Executive summary
- 1.
We recommend performing a bronchoscopy with fungal cultures and GM in BAL in critically ill patients with suspicion of IA (AII).
- 2.
A CT scan may be done. For the diagnosis of IA in non-neutropenic critically ill patients typical signs (halo and air crescent signs) are rarely observed (CIII).
- 3.
Serum galactomannan (GM) is of little value for the diagnosis of IA in non-neutropenic critically ill patients (CIII).
4. – When should we use a IA diagnosis-driven approach?
Searched terms: Diagnostic-driven Antifungal therapy, Galactomannan screening,AspergillusDNA detection
Executive summary
- 1.
The application of a diagnostic-driven approach may be considered only as an alternative strategy for high-risk hematological patients unable to receive anti-mold prophylaxis (BIII). There is no evidence to support such an approach in other high-risk populations, such as SOT recipients (BII).
- 2.
Diagnostic-driven antifungal therapy may be based on the screening (at least on a twice-a-week basis) for serum GM antigen or Aspergillus DNA detection at regular intervals throughout the entire at-risk period (AII). This surveillance should be initiated at the start of the high-risk period (i.e., first cycle of chemotherapy) and continued until no longer at risk. If patient enters subsequent high-risk periods, the surveillance strategy should be reinitiated (AII).
- 3.
Screening for serum GM antigen or Aspergillus DNA detection should not be routinely performed in asymptomatic high-risk patients receiving anti-mold prophylaxis (AII).
4. – How should we improve the growth ofAspergillusin culture?
Searched Keywords: Specimen collection; Aspergillus growth; Calcofluor; Aspergillus culture; Aspergillus culture media.
Executive summary
- 1.
The growth of bacteria presenting in respiratory and other non-sterile samples must be reduced by processing the sample within 2–4h (or refrigerate until processing) and using antibiotic-supplemented media (AII).
- 2.
Microscopic examination of sterile samples and BAL fluid by optical brightener methods (calcofluor or Blankophor) is recommended (AI).
- 3.
In patients with neutropenia or leukemia the isolation of Aspergillus is highly predictive of invasive pulmonary aspergillosis (AI).
- 4.
An incubation temperature of 35–37°C and use of specific media (cornmeal, oatmeal, potato dextrose and Czapek-Dox agar) can encourage growth, sporulation and may permit identification of Aspergillus (AII).
5. – When shouldAspergillusresistance to antifungals be suspected and what are the recommended methods to assess antifungal drug susceptibility?
Searched Keywords: Aspergillus resistance; Azole resistance; Antifungal resistance
Executive summary
- 1.
Aspergillus resistance to antifungal drugs should be suspected in every therapeutic failure scenario and when cryptic species are identified as causative agents of invasive aspergillosis. However, we recommend testing for antifungal resistance in every isolate coming from an invasive infection for epidemiological and antifungal resistance purposes (AII).
- 2.
Commercially available test that have been standardized in multicenter studies can be used in clinical laboratories to screen for resistance; however, European Committee on Antimicrobial Susceptibility Testing (EUCAST) or Clinical Laboratory Standards Institute (CLSI) reference methods should be used to confirm antifungal resistance (AII).
1. – What is the treatment for IA in hematological patients?
a) Which drug has been associated with better outcomes?
Searched Keywords: Aspergillosis; Aspergillus; Treatment; Therapy; Guidelines
Executive summary
- 1.
Voriconazole and Isavuconazole should be considered drugs of choice for primary treatment of IA in hematological patients (AI).
- 2.
Liposomal amphotericin B is an alternative for primary or salvage treatment for patients who are intolerant, had hepatitis or are refractory to voriconazole or isavuconazole. Also for patients with suspected or confirmed triazole resistance, or when triazole use is not desirable due to drug interactions (AII).
- 3.
Echinocandins and posaconazole are not recommended as primary treatment of IA in oncohematological patients (AII), but they are an alternative as salvage therapy when other azoles and liposomal amphotericin B cannot be used (BII).
b) When should we use combination therapy and what are the best regimens?
Searched terms: Aspergillosis,Aspergillus, Combination therapy, Treatment
Executive summary
- 1.
Antifungal combination therapy should not be generally recommended for primary treatment of IA, but it could be consider in selected hematological patients with documented IA (BI).
- 2.
Regarding class of antifungal compounds to be combined, combinations including triazole and echinocandin are the most commonly recommended and specifically voriconazole with anidulafungin would be the best regimen (BI).
- 3.
For salvage treatment of refractory IA, the addition to another agent to initial therapy is in general not recommended, although combination therapy may be consider in individual patients (CIII).
c) Should we monitor treatment response? How?
Searched terms: Aspergillosis,Aspergillus, Response
Executive summary
- 1.
Response assessment of antifungal therapy should be based on a composite of clinical, radiological and mycological criteria in an appropriate period evaluation (AI).
- 2.
A follow-up chest CT scan is recommended to assess the radiological response of invasive aspergillosis to treatment after a minimum of 2 weeks of treatment (CIII).
- 3.
Monitoring of serum galactomannan titers can be used in patients with hematological malignancies and hematopoietic stem cell transplantation recipients to assess therapeutic responses earlier and predict outcomes (AII).
2. – When should we use antifungal empirical treatment for IA in hematological patients?
Searched terms: Preemptive antifungal therapy, Galactomannan screening, Empirical antifungal therapy
Executive summary
- 1.
Due to the poor diagnostic specificity for IA during the presence of persistent or recurrent fever in spite of broad-spectrum antibiotic therapy, empirical antifungal therapy should not be administered in high-risk patients receiving anti-mold prophylaxis or low-risk patients (AII). If indicated, antifungal options include a lipid formulation of amphotericin B (AI), caspofungin or micafungin (AI), or voriconazole (AII). Antifungal treatment different than those used in prophylaxis is recommended (BII).
3. – What is the treatment of IA in patients receiving solid organ transplantation?
Searched terms: Solid organ transplantation, Aspergillosis, Antifungal therapy, Immunosuppression, Voriconazole, Drug-to-drug interaction, Posaconazole, Lung transplantation, Nebulized amphotericin B, Cutaneous squamous cell carcinoma
Executive summary
- 1.
It is recommended initiate early antifungal therapy in SOT patients with high suspicion of IA. Further diagnostic work-up is mandatory to confirm post-transplant IA (AII).
- 2.
Antifungal treatment should be individualized taking into account the type of transplant, the severity of IA, and the immunosuppressive regimen used (AII). The first-line treatment for IA in SOT recipients is voriconazole (AII). When the use of voriconazole may be problematic (increased risk of hepatotoxicity, relevant drug-drug interaction, intolerance or allergy to azoles), a lipid formulation of amphotericin B (L-AmB) is recommended, although potential nephrotoxicity should be taken into account (particularly in kidney transplant recipients) (AIII).
- 3.
The overall amount of immunosuppression should be reduced as an adjunct to antifungal therapy, but without threatening graft outcomes (AII). Most likely, the preferred approach should be based on reducing steroid doses (CIII).
- 4.
In SOT recipients with severe forms of IA (i.e., central nervous system [CNS] involvement or disseminated disease), initiating treatment with antifungal combination therapy should be considered, at least until therapeutic concentrations of voriconazole are achieved (BII).
- 5.
Special considerations for lung transplant recipients include prompt treatment of both Aspergillus colonization of the lower respiratory tract, and nodular or ulcerative forms of Aspergillus tracheobronchitis. Bronchoscopy and high-resolution CT scan should be performed to rule out dissemination (BII).
4. – What antifungal drugs should be used in case of breakthrough aspergillosis (BrA)?
Searched terms: Breakthrough aspergillosis, Breakthrough fungemia, Posaconazole, Micafungin, Caspofungin, Amphotericin B.
Executive summary
- 1.
In patients with BrA is recommended initiating empirical treatment with an alternative class of antifungal with Aspergillus activity until the diagnosis is established and a response to treatment can be documented (BIII).
5. – What is the treatment for IPA in ICU patients?
Searched terms: Aspergillosis, ICU, Treatment
Executive summary
- 1.
Voriconazole is the recommended first-line agent for critically ill patients with invasive pulmonary aspergillosis IPA (BII). Monitoring of serum levels is recommended, even though this triazole is administered intravenously (BII). Isavuconazole iv is the recommended alternative in those patients with severe renal disfunction (BII).
- 2.
Liposomal AmB is the alternative (BII). Echinocandins can be used as salvage therapy preferably in combination therapy (CIII).
- 3.
We do not recommend nebulized AmB as adjunctive therapy in patients with API (CIII).
6. – What is the treatment for chronic pulmonary aspergillosis?
Searched terms: Chronic pulmonary aspergillosis, Aspergilloma,Aspergillusfungal ball, Chronic cavitary pulmonary aspergillosis, Subacute invasive aspergillosis, Treatment, Therapy, Surgery
Executive summary
Treatment forAspergillusfungal ball (Aspergilloma)
- 1.
Asymptomatic patients with stable single aspergillomas may be kept in observation (BIII).
- 2.
Single aspergillomas should undergo surgical resection if there are no contraindications (AIII).
- 3.
If surgery is not feasible, long-term antifungal therapy is recommended. Instillation of antifungal agents in an aspergilloma cavity could be considered in patients with recurrent hemoptysis (CIII).
- 4.
If there is a moderate risk of surgical spillage of the aspergilloma, antifungal therapy with triazoles or an equinocandin should be given peri-/postoperatively (CIII).
Treatment for chronic pulmonary aspergillosis (CPA)
- 5.
In symptomatic patients or with progressive disease, oral antifungal therapy for a minimum of 6 months is the recommended approach (BII).
- 6.
Oral itraconazole (BI) or voriconazole (BII) are the first-line agents. Oral posaconazole is a potential alternative treatment (BIII).
- 7.
In patients who fail therapy, who are intolerant, or develop triazole resistance, intravenous therapy with equinocandins (BI) or amphotericin B (CIII) are alternatives to triazoles.
- 8.
Surgical resection may be necessary in patients with localized disease and intractable hemoptysis, destroyed lung, or azole resistance (BIII).
7. – What is the treatment for central nervous system (CNS) aspergillosis?
Searched terms: Aspergillosis,Aspergillus, Central nervous system
Executive summary
- 1.
Voriconazole is currently considered the standard of treatment of CNS aspergillosis (AIII) and liposomal amphotericin B is the best alternative in cases of intolerance or those refractory to voriconazole (AIII).
- 2.
Clinical experience with posaconazole is scarce in CNS aspergillosis; experimental studies suggest that posaconazole is equivalent to amphotericin B and superior to itraconazole and caspofungin (CIII).
- 3.
The evidence to recommend a combination therapy is weak; however, voriconazole in combination with liposomal amphotericin B has been superior to other combinations or monotherapy in experimental CNS aspergillosis (CIII)
- 4.
Surgical approach should be proposed for therapy, mainly in located lesions, and for diagnosis if conservative procedures have resulted no-conclusive (AIII).
- 5.
Intrathecal or intralesional antifungal chemotherapy and corticosteroids use is currently not recommended for treatment of CNS aspergillosis (CIII).
8. – What is the treatment for other forms of extra-pulmonary IA (intravascular infections, osteomyelitis, septic arthritis, ocular infections and others)?
Searched terms: Extra-pulmonary aspergillosis,Aspergillusendocarditis,Aspergillussinusitis,Aspergillusosteomyelitis,Aspergillusendophthalmitis
Executive summary
- 1.
The treatment of extra-pulmonary forms of IA must include antifungal therapy plus adjunctive surgery (Table 7, supplementary material) (AIII). The preferred regimens are the same as those previously discussed for IPA.
9. – When and how often should we use therapeutic drug monitoring (TDM) for antifungal drugs in aspergillosis? Which levels of antifungals have been related with better outcomes in IA?
Searched terms: TDM, Antifungal exposure, Drug concentration, Amphoterycin B, Voriconazole, Itraconazole, Posaconazole, Isavuconazole, Caspofungin, Micafungin Andifulafungin.
Executive summary
- 1.
TDM of antifungal agents is generally recommended (AII), especially where non-compliance, non-linear pharmacokinetics, inadequate absorption, a narrow therapeutic window, suspected drug interaction or unexpected toxicity are encountered (AI).
- 2.
First sample (trough sample) for TDM must be obtained once the steady state has been reached (3–7 days depending on the antifungal) (AI) and then repeated at least once per week after dose stability is achieved (CIII).
- 3.
A therapeutic range to treat IA between 1mg/L and 6mg/L has been defined for voriconazole (AII). Trough levels >0.7mg/L for prophylaxis and >1.0–1.25mg/L for treatment may be predictive of efficacy for posaconazole (AII). A new target needs to be defined for new posaconazole formulations (BIII). Regarding itraconazole, a trough concentration of 0.5–1mg/L (measured by HPLC) is recommended (AII). TDM for isavuconazole is not currently recommended (BIII).
- 4.
When trough concentration does not reach or exceed the target established, drug dosage should be increased or decreased consequently (AIII).
10. – What is the best treatment forAspergillusinfections caused by azole-resistant isolates?
Searched terms: Azole resistance, Antifungal treatment, Manage azole resistance,Aspergillus lentulus.
Executive summary
- 1.
Therapy of Aspergillus infections caused by cryptic or resistant species should be selected per in vitro susceptibility data, site of infection, and patient characteristics (AIII).
- 2.
Isolates resistant to voriconazole (MIC >2mg/L) are recommended to be treated with amphotericin B (AIII) or the combination of voriconazole with an echinocandin (CIII).
- 3.
In areas with a rate of azole resistance >10%, azole monotherapy should be avoided in empirical primary treatment of severe cases of IA (BIII).
11. – What is the role of adjunctive therapy in IA (including surgical resection and granulocyte transfusion therapy?
Searched terms: Aspergillosis, Adjuvant therapy, Surgery, Granulocyte Transfusion therapy, Interferon-γ
Executive summary
- 1.
Doses of immunosuppressive agents should be reduced as much as possible as an adjunct to antifungal therapy (AII).
- 2.
Granulocyte transfusion therapy may be considered for neutropenic patients with refractory forms of IA and an anticipated duration of neutropenia >7 days. There is no indication for this type of adjunctive therapy in other populations (BII).
- 3.
The administration of recombinant interferon (IFN)-γ may be considered in patients with refractory forms of IA, although its benefit as adjunctive therapy is unclear and must be weighed against the potential consequences of enhancing alloimmune responses (CIII)
- 4.
Adjunctive surgery is recommended in patients with massive hemoptysis, endocarditis, pericardial involvement, invasive sinusitis, or infection of large vessels, bone, subcutaneous tissue, or central nervous system during treatment (BII).
12. – What drugs interact with IA treatment?
Searched terms: Aspergillosis, Drug interaction
Executive summary
- 1.
Antifungal agents may be associated with significant drug-to-drug interactions, leading to sub-therapeutic antifungal drug concentrations and poorer clinical outcomes (AI).
13. – When should we stop treatment for invasive aspergillosis?
Searched terms: Aspergillosis,Aspergillus, Neutropenia, Solid organ trasplant immunosuppression, Treatment, Therapy
Executive summary
- 1.
Treatment for IA should be continued for a minimum of 6–12 weeks. The duration of the antifungal therapy should be individualized, depending on the degree and duration of neutropenia and other immunosuppressive conditions, the site of the disease, and evidence of disease improvement (BIII).
14. – What are the specific recommendations for IA in pediatric population (diagnostic approach, therapy and prophylaxis)?
Searched terms: IA, Children, Diagnosis, Treatment, Prophylaxis
Executive summary
- 1.
The authors recommendation diagnostic approach for pediatric population is the same a that for adults (BII).
- 2.
Voriconazole (AI), and liposomal amphotericin B (BI) are the preferred options for IA treatment. Primary antifungal combined therapy is not routinely recommended in children (CIII). For salvage treatment, voriconazole (AI), liposomal amphotericin B (BI) and caspofungin (AII) are the drugs of choice.
- 3.
High-risk patients (expected IFD incidence >10%) should receive mold active prophylaxis (AII). The drug of choice depends on the studied population.
1. – Does anti-mold prophylaxis reduce the incidence of IA in high-risk populations, and what are the best drugs?
Searched terms: IA, Prophylaxis, Hematologic malignances, Hematopoietic stem-cell transplantation, Organ solid transplantation, Kidney transplantation, Pancreas transplantation, Heart transplantation, Lung transplantation, and Small bowel transplantation
a) Prophylaxis in patients with hematological malignancy and hematopoietic stem-cell transplantation.
Executive summary
- 1.
Prophylaxis with an anti-mold agent is recommended for IA prevention in patients with acute leukemia and prolonged and profound neutropenia; allogeneic HSCT recipients during the neutropenic phase; and those with moderate to severe graft versus host disease (GVHD) and/or intensified immunosuppression (AI).
- 2.
Several antifungal drugs can be used to reduce the incidence of IA in high-risk patients, including posaconazole (AI), voriconazole (AI), itraconazole (BII), micafungin (BIII), caspofungin (CIII), aerosolized L-AmB (BI), and intravenous lipidic formulations of AmB (CII).
b) Prophylaxis in solid organ transplantation.
Executive summary
- 1.
Prophylaxis with an anti-mold agent is recommended for prevention of IA only in high risk patients with organ solid transplantation. Our recommendations and evidence level are summarized in Table 12 (supplementary material).
- 2.
Is there indication for secondary prophylaxis to prevent IA relapse?Search terms: Secondary prophylaxis, antifungal agents, Invasive aspergillosis
Executive summary
- 1.
Secondary prophylaxis aimed at preventing relapse of a previous IA is recommended in immunosuppressed patients, such as allogeneic HSCT in the early phase and with acute or extensive chronic GVHD; with severe and prolonged neutropenia; or undergoing T-cell suppressing therapy, and should be based on treatment response to initial antifungal therapy (AII).
Carolina Garcia-Vidal has received honoraria for talks on behalf of Gilead Science, Merck Sharp and Dohme, Pfizer, Jannsen and a grant support from Gilead Science. She is a recipient of a INTENSIFICACIÓ Grant from the “Strategic plan for research and innovation in health-PERIS 2016–2020”, a research grant from the Ministerio de Sanidad y Consumo, Instituto de Salud Carlos III [FIS PI15/00744] and belong to FungiCLINIC Research group (AGAUR); Ana Alastruey-Izquierdo has received honoraria for talks on behalf of Gilead Science and grant support from Gilead Science, F2G Ltd. and Scynexis; Jordi Carratalà has received honoraria for lectures from Gilead and Merck Sharp and Dohme; Mario Fernández-Ruiz has received honoraria for talks on behalf of Gilead Science, Astellas and Pfizer; JM Aguado has received honoraria for speaking at symposia organized on behalf of Pfizer, Astellas, Merck Sharp & Dohme (MSD), Angelini, and Gilead Science and has sat on advisory boards for antifungal agents on behalf of Pfizer, Astellas, MSD, Angelini, and Gilead Science; Jesús Fortún has received honoraria for speaking at symposia organized MSD and Astellas and a grant support from MSD; José Garnacho-Montero has participated in conferences sponsored by MSD and Astellas and a grant support from Astellas; Jesus Guinea has received funds for educational activities organized on behalf of Astellas, Gilead, MSD, Scynexis, and United Medical. He has also received funds for research from Fondo de Investigación Sanitaria, Gilead, Scynexis, and Cidara; Carlota Gudiol has received honoraria as a speaker from Gilead Science and Merck Sharp; Patricia Muñoz has received honoraria as a speaker from Gilead Science, Merck Sharp and Dohme, Astellas, and Pfizer; Javier Pemán has received honoraria as a speaker from Gilead Science, Merck Sharp and Dohme, Astellas, and Pfizer; Montserrat Rovira has received honoraria for talks on behalf of Gilead Science, MSD-Merck and Pfizer; Isabel Ruiz-Camps has received honoraria for talks on behalf of Gilead Science, MSD-Merck, Astellas, Celgene and Pfizer and has sat on advisory boards for Pfizer and Celgene; Manuel Cuenca-Estrella has received grant support from Astellas, bioMerieux, Gilead Sciences, Merck Sharp & Dohme, Pfizer, Schering Plough, Soria Melguizo, Ferrer International, CIDARA, F2G, Basilea, Amplyx and Scynexis