Colletotrichum spp. are common plant pathogens worldwide. Fruit rots (anthracnose) are often attributed to C. gloeosporioides.1
Colletotrichum spp. have been reported as unusual cause of ophthalmic infections in several countries as United States,2 Japan3 and India.4 Recently, two cases have been reported in our country (Spain).5,6
We present a case of keratitis due to C. gloeosporioides aggravated with herpes virus reactivation and antifungal therapy failure.
A 75-year-old man attended Ophthalmic Outpatient Department (OPD) with a sudden loss of visual acuity after trauma with an orange tree branch (genus Citrus). Slit lamp examination revealed an old walleye secondary herpes infection, corneal oedema and high intraocular pressure (IOP 50). Treatment was initiated with antiglaucoma agents, prophylactic antibiotic (tobramycin) and dexamethasone (1mg/mL plus 3mg/mL, one drop every 4h). Ten days later, the patient presented with aggravation. Biomicroscopic examination showed corneal ulcer and associated hypopyon. Corneal scraping of the ulcer was sent for bacterial culture that was negative. The patient was treated with topical application of antiglaucoma agents, moxifloxacin (5mg/mL, four times a day) and ciprofloxacin ophthalmic ointment (3mg/g, at night) for 4 weeks. Two weeks later there was no enhancement and descemetocele appeared. Given the history of Herpesvirus infection, real-time PCR detection of Herpesvirus DNA was requested (positive to Herpes simplex-1). Topical acyclovir (30mg/g, five times daily for 1 month) and valacyclovir (1g every 8h during 2 months) were added to treatment. Nevertheless, the patient did not respond to therapeutic changes. Corneal scrapings were sent to bacterial and fungal culture and inoculated into usual culture media. Hyphal elements were detected on Gram stain. Thus, the patient received oral (400mg/12h loading dose and 200mg/12h maintenance dose), topical (10mg/mL daily for 7 weeks), intravitreal (100mcg/0.1mL), and intrastromal (1%) voriconazole treatment.
A rapidly growing fungus produced colonies on Sabouraud-chloramphenicol culture media. Lactophenol-cotton blue (Merck Millipore®, Madrid, Spain) mount of the smear, showed unbranched hyphae with cylindrical conidia typical of the genus Colletotrichum. Molecular studies were utilized to species identification.7 The isolate was identified as C. gloeosporioides using the Basic Local Alignment Search Tool (BLAST) program. The nucleotide sequence showed 98% homology match with accession number KC341915.
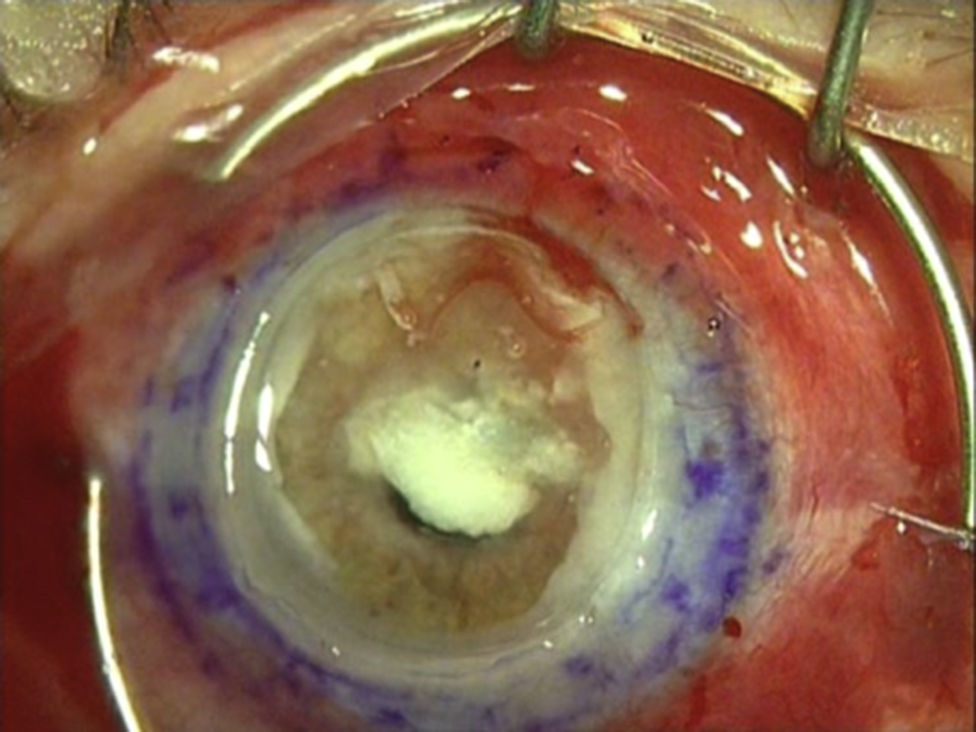
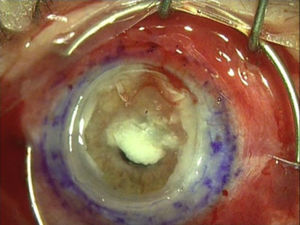
The patient did not respond to the 7 weeks voriconazole treatment and suffered corneal melting (Fig. 1). Therapeutic penetrating keratoplasty was performed. New fungal recurrence was seen after surgery with melting of donor corneal button. Due to poor prognosis and lack of response to therapy, eye evisceration was performed.
Colletotrichum spp. are an uncommon cause of keratitis. The species implicated in human infections include C. dematium, C. coccodes, C. graminicola, C. gloeosporioides, C. crassipes and C. truncatum.8 They have mainly been involved in keratitis, although subcutaneous and systemic infections among immunosuppressed patients have also been reported.9,10 A Pubmed search using “Keratitis” and “Colletotrichum” as keywords revealed 18 reports, including 64 patients with ophthalmic infections. Colletotrichum spp. eye infections are increasingly reported, even though the rate of isolation is still low (from 1.9% to 2.8%).2,4
Fernandez et al. described principal risk factors associated to Colletotrichum keratitis; they reported that ocular trauma followed by diabetes mellitus and corticosteroid use were the principal characteristics of a series of patients with Colletotrichum keratitis.2 Our patient fulfilled these main risk factors. The route of entry was through trauma with an orange tree branch, similar to that of other cases reported in our country.5,6
Due to the difficulty of morphological identification, molecular techniques are the most suitable method for isolates identification to the species level.8
There is a lack of consensus in the literature regarding the optimal therapy against Colletotrichum spp. ophthalmic infection. Most articles reported successful therapy with topical natamycin.2,4 Combination therapy with natamycin plus other antifungal agents have shown resolve on infection in several cases too.3,11 Our patient received oral, topical, intravitreal and intrastromal voriconazole showing no improvement of eye lesion, as well as Navalpotro et al. reported recently.5 The unsuccessful treatment and fatal outcome of our patient may possibly be due to diagnostic and surgical delay procedures along with Herpes simplex-1 virus reactivation in an already compromised cornea. Combination therapy may be more effective than monotherapy. Moreover, natamycin and voriconazole could be a good treatment as suggested by Shiraishi et al.3