Arthrobacter creatinolyticus is a Gram-positive aerobic coccobacillus, catalase-positive, belonging to the family Micrococcaceae, order Actinomycetales, usually found in soil and in the environment. This organism produces urease, an extracellular enzyme with many industrial applications and a potential use in anti-cancer therapy due to its cytotoxic effect.1
We have only found in the literature one case of bacteremia due to this microorganism, and none confirmed as a cause of urinary tract infection. We present a case of urinary tract infection due to A. creatinolyticus.
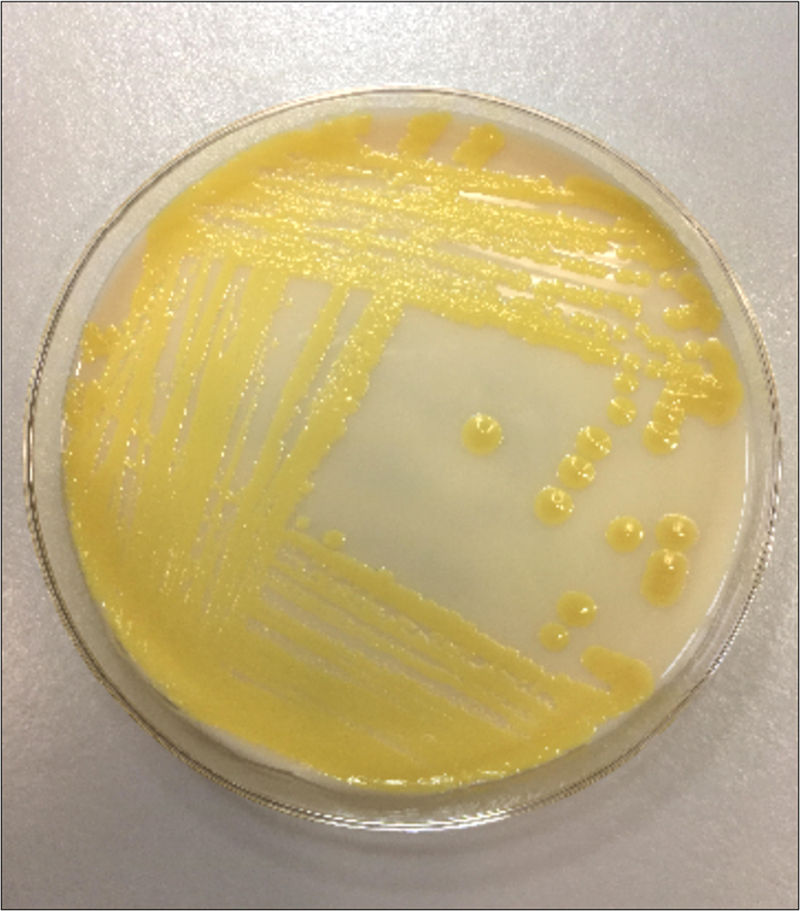
A woman, in her ninety, came to the primary care with signs of agitation. The patient presented several pathologies as hypertension, diabetes, Parkinson's disease and vascular dementia. She was aggressive at the time of consultation and the exploration was complicated as well as the anamnesis that was unable to stablish the presence of urethral syndrome. In addition no urine test strip or sediment analysis was done. The caregiver confirmed that the patient did not had fever but she had been agitated for the past four days. On the suspicion of urinary infection, the doctor ordered a urine culture and prescribed fosfomycin empirically. After 24h of incubation in the chromogenic medium UTIR (Oxoid LTD, UK), >100,000CFU/mL of A. creatinolyticus were isolated (Fig. 1).
The identification of the microorganism was performed by mass spectrometry using the MALDI-TOF Biotyper 3.1 (Bruker Daltonic GmbH, Bremen, Germany), resulting in A. creatinolyticus with a score of 2.3. This identification was confirmed by sequencing the 16 rRNA gene. To our surprise, the result was different: Glutamicibacter creatinolyticus. In fact, this is the same microorganism, being A. creatinolyticus its basonym (Hou et al., 1998),2 which has recently been reclassified into a new genus. The sequence was 99% indentical to G. creatinolyticus type strain KY814694.1 using the NCBI 16S rRNA gene database.
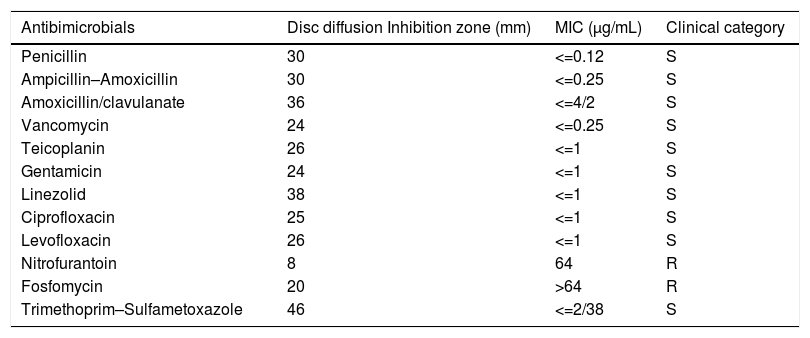
The susceptibility to antimicrobials was performed by disc diffusion test and also by broth microdilution method using the automated system MicroScan Walkaway (Beckman Coulter, USA) using the Pos MIC Panel Type 33. The interpretation of the minimum inhibitory concentrations (MICs) was performed according to the breakpoints for Corynebacterium spp. and related groups established by the Clinical and Laboratory Standards Institute (CLSI) (Table 1).
Antimicrobial susceptibility profile of Arthrobacter creatinolyticus.
| Antibimicrobials | Disc diffusion Inhibition zone (mm) | MIC (μg/mL) | Clinical category |
|---|---|---|---|
| Penicillin | 30 | <=0.12 | S |
| Ampicillin–Amoxicillin | 30 | <=0.25 | S |
| Amoxicillin/clavulanate | 36 | <=4/2 | S |
| Vancomycin | 24 | <=0.25 | S |
| Teicoplanin | 26 | <=1 | S |
| Gentamicin | 24 | <=1 | S |
| Linezolid | 38 | <=1 | S |
| Ciprofloxacin | 25 | <=1 | S |
| Levofloxacin | 26 | <=1 | S |
| Nitrofurantoin | 8 | 64 | R |
| Fosfomycin | 20 | >64 | R |
| Trimethoprim–Sulfametoxazole | 46 | <=2/38 | S |
CLSI criteria: S, susceptible; R, resistant.
After knowing the pattern of antimicrobial susceptibility, the treatment was changed to oral levofloxacin 250mg daily for five days. One week after the end of treatment and due to the persistence of the agitation, the doctor ordered a new urine culture. Again, the same microorganism was isolated (>100,000CFU/mL), and a new treatment was prescribed, with ciprofloxacin 250mg bid for two weeks.
In a third urine culture taken 3 weeks later, A. creatinolyticus was isolated once again in a lower count (less than 10,000CFU/mL) and the antimicrobial susceptibility profile remained unchanged. At this point, the clinical status of the patient had improved but she had developed a cystocele, and we considered that the organism was colonizing the urinary tract.
As we have previously mentioned, there is only one reported case of bacteremia due to this microorganism in an elderly person with diabetes and acute cholangitis.3 On the other hand, another case reported describes the isolation of A. creatinolyticus strains found in the urine of patients with neuroblastoma4 and low levels of creatinine in serum and urine. The authors emphasized that this bacterium possesses creatinase, an enzyme able to hydrolyze creatinine, but they did not find any clinical evidence of urinary infection caused by this organism.
In our patient, the existence of urinary tract infection based on the recent change on her clinical or functional status (acute confusional disorder, discomfort or agitation)5 was confirmed twice by the presence of significant bacteriuria due to A. creatinolyticus. The patient clinical status improved but finally developed a cystocele due to the weakening of the pelvic muscles indicating that the organism was colonizing the bladder of the patient.
Another species of this bacterium have also been described6,7 as the etiologic agents of urinary tract infection (A. albus, A. aurescens, A. cumminsii, A. protophormiae), and according to our case, we must include G. creatinolyticus (bfn. Arthrobacter) as an emerging pathogen causing urinary infection in the elderly.