Introducción: La colangiopancreatografía retrógrada endoscópica en pacientes con estenosis del conducto biliar es la mejor opción de tratamiento. Nuestro objetivo fue evaluar los resultados en un seguimiento a largo plazo de los pacientes con estenosis biliar no asociados a procedimientos quirúrgicos.
Material y métodos: Análisis retrospectivo de los datos. Se incluyeron pacientes con estenosis biliares no asociadas a los procedimientos quirúrgicos.
Resultados: Siete pacientes fueron incluidos: 6 (85,7%) pacientes eran hombres y 1 (14,3%) era una mujer, con una edad media de 69 (rango 29-92) años. Cinco (71,4%) pacientes tenían estenosis secundarias a coledocolitiasis, un (14,3%) paciente con colangiopatía portal, una (14,3%) colangitis esclerosante primaria. El tiempo de seguimiento después de la CPRE fue de 15,9 (3-68,9) meses. Todos los pacientes fueron tratados con éxito inicial, pero uno presentó recurrencia de la estenosis al final del seguimiento. Se observó un caso de pancreatitis aguda leve. Un paciente fue sometido a tratamiento quirúrgico después de tres meses de seguimiento.
Conclusión: El tratamiento endoscópico es una opción eficaz y segura para los pacientes con estenosis biliar no asociados a procedimientos quirúrgicos.
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is the best treatment option in patients with bile duct strictures. Our aim was to evaluate the long-term outcome in a follow-up study of patients with biliary stricture not associated to surgical procedures.
Material and Methods: a retrospective analysis of data was made. Patients with biliary strictures not associated to surgical procedures were included.
Results: Seven patients were included: six (85.7%) patients were male and one (14.3%) female; median age was 69 (range 29-92) years. Five (71.4%) patients had strictures associated with choledocholithiasis, one (14.3%) patient due to portal cholangiopathy and one (14.3%) with primary sclerosing cholangitis. The time of follow-up after the last ERCP procedure was 15.9 (3-68.9) months. Initial success was 100%, but there was one recurrence at follow-up. One case of mild acute pancreatitis was observed. One patient was sent for surgery after three months of follow-up.
Conclusion: endoscopic treatment is an effective and safe option for patients with biliary strictures not associated to surgical procedures.
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) in patients with bile duct strictures associated with surgical events is the best treatment option.1 Symptoms in these patients are often associated with cholestasis, recurrent cholangitis, ductal stones, or secondary biliary cirrhosis. Management was traditionally surgical, the favorite option being Roux-en-Y choledochojejunostomy, with a successful outcome in 76%-90% of cases, but significant associated morbidity (18%-51%) and mortality (4%-13%)2,3Endoscopic treatment is a useful procedure in this group of patients that has shown good results in previous studies.4
Our aim was to evaluate the long term outcome during follow-up of a group of patients with biliary stricture not associated to surgery.
Patients and methods (patients, data collection, interventions and follow-up)
Patients
Data about endoscopic management and outcome of benign biliary strictures, not-associated to laparoscopic or open cholecystectomy, referred to our tertiary-care medical center between January 2005 and December 2007, was collected retrospectively. In every case, before the first procedure, complete blood count, INR, and prothrombin time were obtained for all patients to minimize the risk of bleeding. An experienced endoscopist in ERCP performed the ERCP in all cases. All follow-up procedures for an individual patient were performed in the same endoscopic center by the same team. Written informed consent was obtained for each patient and all procedures were performed under deep sedation with midazolam, propofol and phentanyl by an anesthetist.
A TJF-160F duodenoscope (Olympus, American Corp., Melville, NY, USA). Supplemental oxygen was provided by means of nasal catheter. All patients were hospitalized after the procedure for at least two hours for surveillance of possible complications. Inclusion criteria were as follows: post-sphincterotomy stricture; extrinsic compression secondary to chronic pancreatitis; primary sclerosing cholangitis; and stricture associated to bile duct stones.
Data collected included patient characteristics, laboratory results, endoscopic interventions, surgical management, immediate and long term morbidity and mortality. All patients were followed as outpatients. The duration of follow-up was calculated from the date of the last ERCP. We evaluated the outcome according to early complications after ERCP (perforation, pancreatitis, post-sphincterotomy bleeding and acute cholangitis), laboratory results, stricture recurrence, development of abdominal pain, fever or jaundice, episodes of acute cholangitis and mortality.
Stricture classification and management
The strictures were graded according to the following classification:4 type I, low common bile duct stricture more than two cm from the hepatic duct confluence; type II, middle common bile duct stricture less than two cm from the hepatic duct confluence; type III, stricture of the right hepatic duct; type IV, stricture of the left hepatic duct and type V, stricture of the hepatic duct confluence. The rule followed by all endoscopists was that stents were electively exchanged every three months for a one year period or more if necessary, based on ERCP features. However, in some cases stents were removed earlier and not exchanged if the strictures was considered to be adequately dilated based on the following criteria: (1) dilation of the stricture on cholangiography was complete; (2) drainage of contrast from the biliary tree and complete; and (3) an inflated extraction balloon could be passed through the stenosis without significant resistance. At the time of biliary stent exchange, all biliary stents were generally removed, the stricture was evaluated and endoscopic stricture dilatation and/or an increasing size or number of plastic stents were placed until complete morphologic resolution of the stricture was observed. The initial endoscopic procedure consisted of the insertion of polyethylene stents bridging the stricture. There was no standardized protocol for all endoscopists regarding the diameter or the number of stents but each one followed their same approach. If the stricture was too tight to allow stenting, dilation using a bougie or hydrostatic balloon was performed. The diameter and number of stents introduced during each ERCP were tailored to the size of the bile duct, but there was no systematic intent to maximize the number of stents inserted. Long-term success of endoscopic treatment was evaluated with periodic liver function tests. Failure to adequately dilate the biliary stricture resulting from inability to pass the stricture with guidewires were considered early failures; late failures were considered when there was stricture persistence or recurrence during follow-up. In these patients, elective surgery with end-to-side Roux-en-Y hepaticojejunostomy was performed.
Statistical analyses
Descriptive statistics for nonparametric distribution (median and ranges, relative frequencies and absolute frequencies) was used.
Results
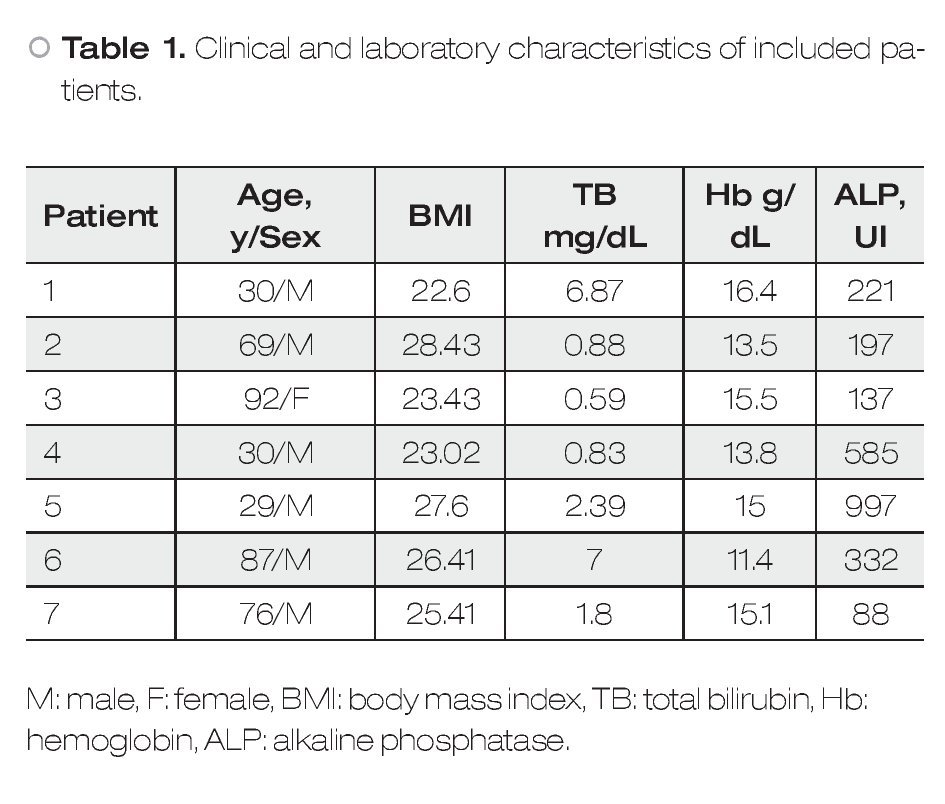
In 36 months, 32 patients were identified; twenty-five had a biliary stricture associated to cholecystectomy and they were excluded from this analysis. We included seven patients with biliary strictures not associated to surgery: 6 (85.7%) patients were male and 1 (14.3%) female; median age was 69 (range 29-92) years. Five (71.4%) patients had stricture due to cholecholithiasis, one (14.3%) patient to portal hypertension (portal cholangiopathy), and one (14.3%) due to primary sclerosing cholangitis. The clinical and demographic features of the included patients are shown in Table 1.
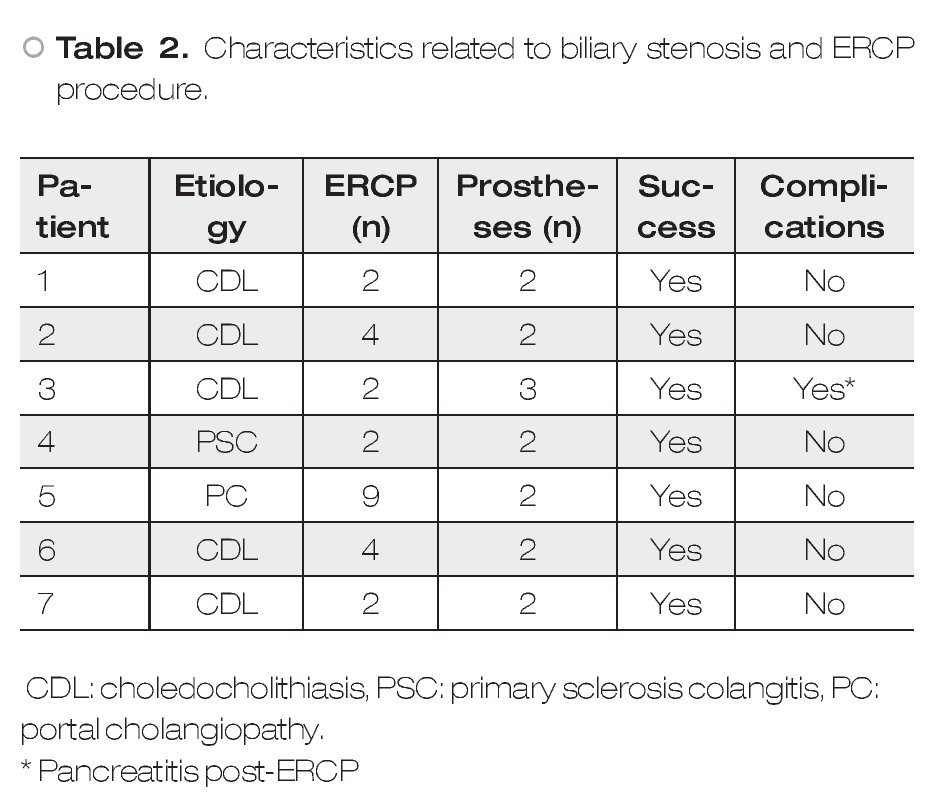
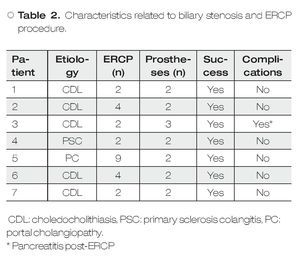
The time of follow-up after the last ERCP procedure was 15.9 (3-68.9) months. Table 2 shows the features of the ERCP procedures. Two patients were treated with pneumatic endoscopic balloon dilation (EBD) besides the stents. All patients were treated with initial success but one had recurrence after follow-up. Only one patient presented a complication associated to ERCP (mild acute pancreatitis). One patient underwent surgery after three months of follow-up.
Discussion
In this study a good response rate with endoscopic treatment was observed in patients with biliary strictures not associated to surgical procedures.
Currently, few trials have investigated the outcomes of endoscopic management of benign strictures not associated to surgery .4 Therapeutic ERCP may be beneficial for patients with recurrent pyogenic cholangitis who have mainly extrahepatic disease, or those felt to be poor surgical candidates. Studies in these patients have shown an approximate 70% success rate at two year follow-up following endoscopic intervention.5 In this work, the success rate was similar to previously reported studies. However, patients with intrahepatic duct strictures are more difficult to treat, and surgical bypass drainage may be more appropriate. According to previous studies4 it is also unclear if there are any benefits of therapeutic ERCP in other entities, such as portal vein cavernous transformation or portal biliopathy due to biliary varices. In our series, we included only one patient with this pathology and the clinical result at follow-up was good.
Regarding patients with PSC and dominant strictures, endoscopic management has led to promising results.6,7 However, existing trials have been small, retrospective, and uncontrolled, so it is difficult to draw definitive conclusions from them. In this work we included one patient with PSC and the results with endoscopic treatment were good. It is in agreement to previous reports in which the endoscopic management of dominant strictures in the setting of PSC leads to favorable outcomes. However, it is still not clear whether dilatation, stent insertion, or both are the most appropriate option. Furthermore, in the case of stent insertion, the optimal duration and frequency of stent change remain to be determined. In the absence of randomized trials, dilatation with or without short-term stent insertion appears to be a reasonable approach.6,7
Some limitations in this study have to be mentioned: First, the small sample size and secondly, the retrospective design. However, it would be difficult to perform a large prospective study, and moreover a randomized controlled trial, due to the low frequency of these types of patients. Moreover, to our knowledge this series represents the first report from a Latin America center and because of this the results are useful for future comparisons.
In conclusion, endoscopic treatment is an effective and safe option for patients with biliary stricture no associated to surgical procedures.
Financial Disclosure
All authors have no conflicts of interest or financial ties to disclose.
Correspondence: Dr. Félix I Téllez-Ávila,
Department of Gastrointestinal Endoscopy, Instituto Nacional de Ciencias Médicas y Nutrición "Salvador Zubirán", Vasco de Quiroga #15, Col. Sección XVI, Del. Tlalpan, CP 14000, México City, México.
E-mail: felixtelleza@gmail.com