La elastografía examina las propiedades elásticas de los tejidos mediante la aplicación de una ligera compresión y la comparación de las imágenes obtenidas antes y después de la compresión. La elastografía es una nueva aplicación en el campo de la ecografía que parece ser capaz de diferenciar el tejido fibroso y lesiones benignas de las malignas. Mientras que nuestros resultados son muy alentadores, la investigación adicional será necesaria para definir mejor el papel de esta nueva técnica, así como posteriormente la evaluación con varios operadores en un ambiente cegado. La elastografía guiada por ecoendoscopia tiene el potencial para orientar en el diagnóstico y el tratamiento de trastornos gastrointestinales relacionados con tumores.
Elastography examines the elastic properties of tissues by applying a slight compression to the tissue and comparing the images obtained before and after this compression. Elastography is a new application in the field of endosonography that seems to be able to differentiate fibrous and benign tissue from malignant lesions. While our results are very encouraging, further research will be needed to further define the role of this new technique as well as subsequently assessing the technique using multiple operators in a blinded setting. EUS-guided elastography has the potential for further guiding the diagnosis and therapy of gastrointestinal-related tumours.
Introduction
It is well known that inflammatory conditions and tumors lead to an alteration of the normal tissue structure, causing changes in its elasticity. Because malignant tissues are generally harder than normal surrounding tissues, measurement of tissue elasticity might be useful for the differential diagnosis of masses. Endoscopic Ultrasound elastography or Sonoelastography (SE) is a real-time method used to assess tissue elasticity by applying a slight compression to the tissue and comparing images obtained before and after compression.1
Technical Specifications
Conventional ultrasound images (B-mode) are formed from the reflected ultrasound signals taken from the body. Ultrasound signals are attenuated according to the density of different tissues. The signals received back are reconstructed and displayed on the screen by way of ultrasound images. Occasionally, some tumors may have similar echogenicity to normal tissues and therefore are difficult to visualize with the B-mode. However, these tumors often have a change in hardness in relation to the surrounding tissue. SE is a technique that is capable of determining the tissue hardness which can provide the clinician with valuable information regarding the potential differential diagnoses. It is important to note that these measurements are performed using the surrounding tissue for comparison. The information obtained under normal conditions (no pressure) and after the application of gentle pressure is thus compared. In the living human body, the pressure from the arteries and/or the respiratory movements normally exert this pressure.
The foregoing principle is expressed more clearly if we consider the case of normal tissue when pressure is applied: the distance between the transducer and the reflection point will be shorter than without pressure. The transducer will then detect that there was a change in the ultrasound wave and therefore provides a measure ("X") of the elasticity of that particular tissue. In contrast, if the pressure and the measurements are performed on a hard tissue, the distance between the transducer and the point of reflection of the ultrasonic wave will be the same or very similar before and after compression. The transducer will detect that there was minimal or no change and therefore provides a measure of "Y" of elasticity of that tissue. The areas where tissue compression was easily applied will be reported as areas of high elasticity while areas with less elastic tissue will be reported as less elastic ("hard") or of low elasticity. Tissue areas adjacent to areas of interest can be analyzed by this system. In the case of highly elastic tissue, compression will tend to expand the compressed tissue laterally and thus induce an artifactual change in this surrounding tissue. For less elastic tissue this does not occur.
The mathematical basis of Elastography is based on the combined autocorrelation method described by Yamakawa and Shiina.2 The distribution of tissue elasticity is calculated by the finite element method described by Nitta.2 These concepts are beyond the scope of this review.
Results of studies using SE
Initial studies for the implementation of elastography were conducted in experimental models created from tissues consisting of 30% gelatin (tumor) surrounded by 10% gelatin (normal tissue). It was observed that during the conventional B-mode display, differentiation of both concentrations of gelatin (simulating two different tissues) was difficult. Larger differences in concentration facilitated differentiation. To make these differences clearer, color coding was added to represent degrees of elasticity. Less elastic tissue is shown in blue while harder tissue (such as fibrosis) is shown in green and fat is shown in red. Yellow is used for normal tissue.
Clinical Applications
Giovannini et al,3 made the first report of the clinical utility of SE in 2006 with data from 49 patients. This work showed that elastography had a promising future in the study of pancreatic lesions and the study of infiltration of lymph nodes. The possibility was raised that elastography could be appropriate to classify a tissue as malignant or not non-invasively.
Between March 2004 and April 2005, 49 patients underwent EUS examination with SE. Indications included evaluation of a pancreatic mass (n=24) and assessment of suspicious LN (n=25). The real-time elasticity imaging described in this study was performed with the SE module that was integrated into the platform of the HITACHI EUB-8500 system (Hitachi Medical Systems Europe, Zug, Switzerland®). Like color Doppler examinations, tissue elasticity imaging was performed with the EG 38-UT EUS-scope (Pentax Europe Gmbh, Hamburg, Germany®) and does not require additional instruments. The examination results are represented in color over the conventional B-mode image with malignant tissue appearing in blue, fibrosis in green, normal tissue in yellow and fat in red. A EUS FNA was performed in all cases using a 22-gauge needle (Cook Medical, Winston-Salem, NC®). Masses or LN that appeared mostly blue (harder) were considered malignant, with other results considered benign. Final diagnosis was based on histology from FNA and surgical, when available.
Pancreatic Masses
Twenty-four patients (median age 60 years (range 39-88) underwent EUS examination with SE for evaluation of a pancreatic mass (mean diameter 24.7-11.1mm). Masses were located in the pancreatic head (n=12), body (n=6) and tail (n=6). Final histology was based on FNA results in 21 cases and surgical pathology in three cases. Final diagnosis of malignant masses included; adenocarcinoma of the pancreas (n=14), metastatic renal cancer (n=2), sarcoma (n=1) and ovarian cancer (n=1). Benign masses consisted of chronic pancreatitis-related nodule (n=4), neuroendocrine tumor (n=1) and an IPMT (n=1). SE images of pancreatic masses were interpreted as benign in four cases and malignant in 20. Two masses were misclassified as malignant by elastography; the first was a neuroendocrine tumor and i the second a benign fibromyoblastic tumor of the pancreas. Sensitivity and specificity of SE in the diagnosis of malignant lesions was 100% and 67%, respectively.
Lymph Nodes
Twenty-five patients (median age 57 years (range 16-76) underwent EUS examination with SE of 31 LN. The mean diameter of the LN was 19.7-8.6 mm and were located in the cervical area (n=3), mediastinum (n=17), coeliac arterial trunk region (n = 5) and aortocaval region (n=6). Final histology was based on FNA and concluded the LN to be benign in 14 cases and malignant in 17. SE images of the LN were interpreted as malignant in 22 cases, benign in seven and indeterminate in two. While there were no false-negatives, there were five false-positives. The indeterminate cases were due to heterogenicity of the SE images and were both benign on final histology. The sensitivity and specificity of SE in the evaluation of malignant invasion of LN was 100% and 50%, respectively. Six patients had SE of more than one LN. In two of these cases, one LN was benign and the other malignant, and SE correctly differentiated between the two.
In general, the accuracy of EUS elastography for the differential diagnosis of benign and malignant LNs has been assessed in a series of studies, with the sensitivity ranging from 79%to 100% and specificity ranging from 50% to 96%.
Results of a Prospective Multicenter Study on Pancreatic Masses4
Between October 2006 and February 2007,121 patients (77 male and 44 female), mean age 63 years, underwent EUS for a pancreatic mass. Final diagnosis was obtained by EUS-FNA in 82 cases and by surgery in 39 cases. Final histology was pancreatic adenocarcinoma (72 cases), endocrine tumors (16 cases), benign nodule of chronic pancreatitis (30 cases), and pancreatic metastasis (three cases). Elastography showed malignant aspects (intense blue coloration) for all pancreatic adenocarcinomas, endocrine tumor and pancreatic metastasis as well as for pancreatic sarcoma. All nodules of chronic pancreatitis presented benign features (mixed green and low intensity of blue). A SE score for LN was divided into five categories (1-5). If categories 1 and 2 are considered as benign, and categories 3-5 as malignant, the sensibility, specificity, PPV and NPV of EUS SE to differentiate benign from malignant pancreatic masses were respectively: 80.6%, 92.3%, 93.3% and 78.1% with a global accuracy of 89.2%. The NPV for malignancy of categories 1 and 2 was 77.4% and the PPV for malignancy of categories 3-5 was 92.8%. An interobserver study on 30 patients, showed good concordance (kappa score = 0.7) for the diagnosis of malignant pancreatic masses using SE.
Results of a Prospective Multicenter Study on Lymph Nodes Staging4
During the same period, 101 patients (56 male and 45 female), mean age 61.1 years, underwent EUS FNA of LN for staging of lung cancer (26 cases), esophageal carcinoma (25 cases), gastric cancer (13 cases), pancreatic cancer (12 cases), for a suspicion of LN relapse of a kidney cancer (two cases) and of a breast cancer (eight cases). A EUS FNA was also performed in 15 cases for isolated LN. LN were located in the mediastinum (51 cases), the cervical area (four cases), the celiac or mesenteric area (44 cases) and perirectal space (two cases). The mean size of the lesion was 20.1 mm (range: 7-50 mm). Final histology was malignant LN (55 cases including 35 metastasis by adenocarcinoma, 13 by squamous cell carcinoma, three by endocrine tumor, one melanoma and five lymphomas) and inflammatory LN (44 cases including three cases of sarcoidosis). The LN SE classification was done in five categories as described above. If categories 1-3 are considered as benign and categories 4-5 as malignant, the sensibility, specificity, PPV and NPV of EUS SE to differentiate benign from malignant LN were respectively: 100%, 83.3%, 100% and 75%. But, if we consider categories 1 and 2 as benign and categories 3-5 as malignant, the sensibility, specificity, PPV and NPV of EUS SE to differentiate benign from malignant LN were respectively: 88.10%, 88.13%, 91.22% and 84.10% with an accuracy of this new technique between 88% and 89.10%.
Results of a Recent Meta-Analysis for Study The Diagnostic Yield of Elastography on Differentiation of Benign and Malignant Lymph Nodes1
The pooled sensitivity of EUS elastography for the differential diagnosis of benign and malignant LNs was 88% (95% confidence interval [CI] 0.83-0.92), and the specificity was 85% (95% CI, 0.79-0.89). The area under the curve was 0.9456. The pooled positive likelihood ratio was 5.68 (95% CI,2.86-11.28), and the negative likelihood ratio was 0.15 (95% CI, 0.10-0.21). The subgroup analysis by excluding the outliers provided a sensitivity of 85% (95% CI, 0.79-0.90) and a specificity of 91% (95% CI, 0.85-0.95) for the differential diagnosis of benign and malignant LNs. The area under the curve was 0.9421.(5-8)
Interpretation
Method based in colors
The classification or SE score for a pancreatic mass proposed by Giovannini et al, includes five categories:
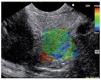
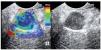
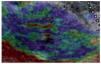
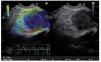
Category 1 is for a homogenous low elastography area (soft, green) and corresponds to the normal pancreas tissue (Figure 1). For images classified as category 2 (Figure 2) there is heterogeneity of the elastography but in the soft tissue range (green, yellow, and red) and corresponds to fibrosis. Category 3 (Figure 3) is for elastography images which is largely blue (hard) with minimal heterogeneity and corresponds to a small, early (less than 25 mm) pancreatic adenocarcinoma. In tumors assigned Category 4 (Figure 4) there exists an hypoechoic region with green appearance in the center of the tumor, surrounded by blue or harder tissue and corresponds to a hypervascular lesion, such as a neuroendocrine tumor or small pancreatic metastasis. Finally, Category 5 (Figure 5) is assigned to lesions which are largely blue on SE but with heterogeneity of softer tissue colors (green, red), representing necrosis, and is seen in advanced pancreatic adenocarcinoma. The elasticity of soft tissues depends to a large extent on their molecular composition (fat, collagen, etc.), as well as on the microscopic and macroscopic structural organization of these blocks. In the normal pancreas, for example, the glandular structure may be firmer than the surrounding connective tissue, which in turn is firmer than the subcutaneous fat. SE allows the hardness or stiffness of biological tissues to be estimated and imaged using conventional ultrasound instruments with modified software. It is known that certain pathologic conditions, such as malignant tumors, often manifest themselves as changes in the mechanical properties of tissue. We believe that the elastic properties of benign lesions are fairly uniform, such as throughout a benign tumor. Cancerous tumors, on the other hand, grow in a very disorganized way. Therefore, within a given malignant tumor, the elastic properties of one area of a tumor may be significantly different from those in another area. The concept relating to the measurement of these tissue changes is an extension of the basic principles associated with traditional medical ultrasonic imaging. The principle is based upon the fact that tissues are deformed slightly when a small displacement is externally applied
Figure 1. Category 1 is for a green area, which corresponds to normal pancreas tissue.
Figure 2. Category 2, area of heterogeneity in green, yellow and red, which corresponds to fibrosis.
Figure 3. Category 3, images that are largely blue (indicative of hard tissue) with minimal or no heterogeneity.
Figure 4. Category 4, green appearance for the central small area surrounded by blue (or hard) tissue, which corresponds to a hypervascular lesion, such as a neuroendocrine tumor or small pancreatic metastasis.
Figure 5. Category 5, lesions which are largely blue but are heterogeneous with softer tissue colors (green, red), representing necrosis; usually seen in advanced pancreatic adenocarcinoma.
Methods based in ratio-elastography
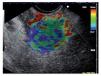
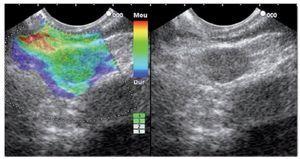
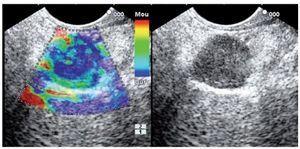
Representative areas from the mass (A) and soft reference areas (B) are analyzed. The result of the elastographic evaluation is defined by the quotient B/A (strain ratio). In Figure 6 a ratio-elastography of a pancreatic cancer is shown (ratio=25.27).
Figure 6. A ratio-elastography is shown. The ratio between measures in the small circle of normal tissue (A) and cancer tissue in the big circle (B) is over 10 (ratio=25.27).
In a study performed by our group (8), elasticity coefficient was calculated as the ratio between the elasticity coefficient of the lesion on the elasticity coefficient of the normal surrounding tissue.
Final histologic diagnosis was obtained by EUSFNA (n=66) or by surgery (n=20). Regarding pancreatic masses, using a cut-off of elastography ratio of 10, sensibility, specificity, PPV, NPV and accuracy for the diagnosis of, were respectively: 95.1%, 83.3%, 97.5%, 71.4, and 92.3%. Concerning LNs (using the same cut-off =10) sensibility, specificity, PPV, NPV and accuracy for the diagnosis of malignant LN, were respectively: 95.8%, 80%, 88.4%, 92.3, and 89.6%. Ratio-elastography (using a cut-off ratio > 10) can differentiate benign from malignant tissue in 90% of cases.
Limitations
Adequate and reproducible elastographic imaging of focal pancreatic disease is confined to lesions with a diameter of less than 30 mm. It is important to note that for optimal acquisition of elastographic images depends on examining the surrounding pancreatic parenchyma (ratio 1:1; for comparison). In the present, there is actually no validated classification or score of the different categories for the elastographic images that is universally accepted.
Conclusions
SE is a promising tool for the endoscopist regarding a particular patient with pancreatic mass or maybe in patients with enlargement of multiple LN. This new tool could help to make the decision about which lesions have to be biopsied or in case of a pancreatic mass, if the FNA could be obviated.
Correspondence: Marc Giovannini M.D.
Endoscopic Unit, Paoli-Calmettes Institute, 232 Bd St-Marguerite, 13273 Marseille cedex 9 France.
E-mail: giovanninim@wanadoo.fr