Ectopic secretion (ES) of adrenocorticotropic hormone (ACTH) occurs in approximately 10% of patients with ACTH-dependent Cushing's syndrome. Approximately 50% of cases are caused by intrathoracic tumors, most of which are small bronchial carcinoids (BCs) which are very difficult to locate and which are only found after years of search. Imaging techniques routinely used for BC localization include computed tomography (CT), magnetic resonance imaging (MRI), scans using somatostatin receptor analogues (OctreoScan®) and positron emission tomography with fluorodeoxyglucose (18FDG-PET), which is far less widely used.
We report a case where BC was located using the latter procedure 6 years after its presentation.
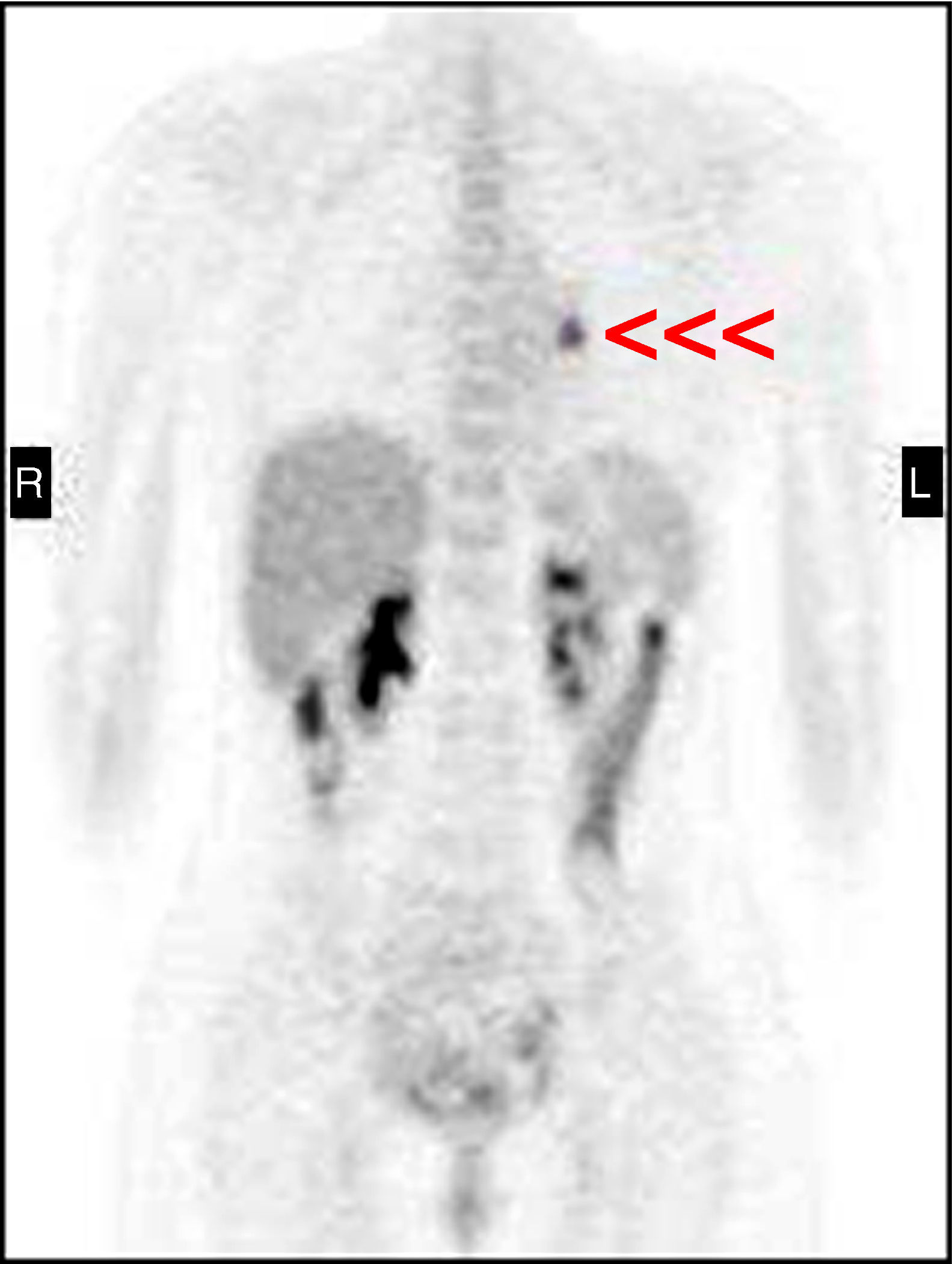
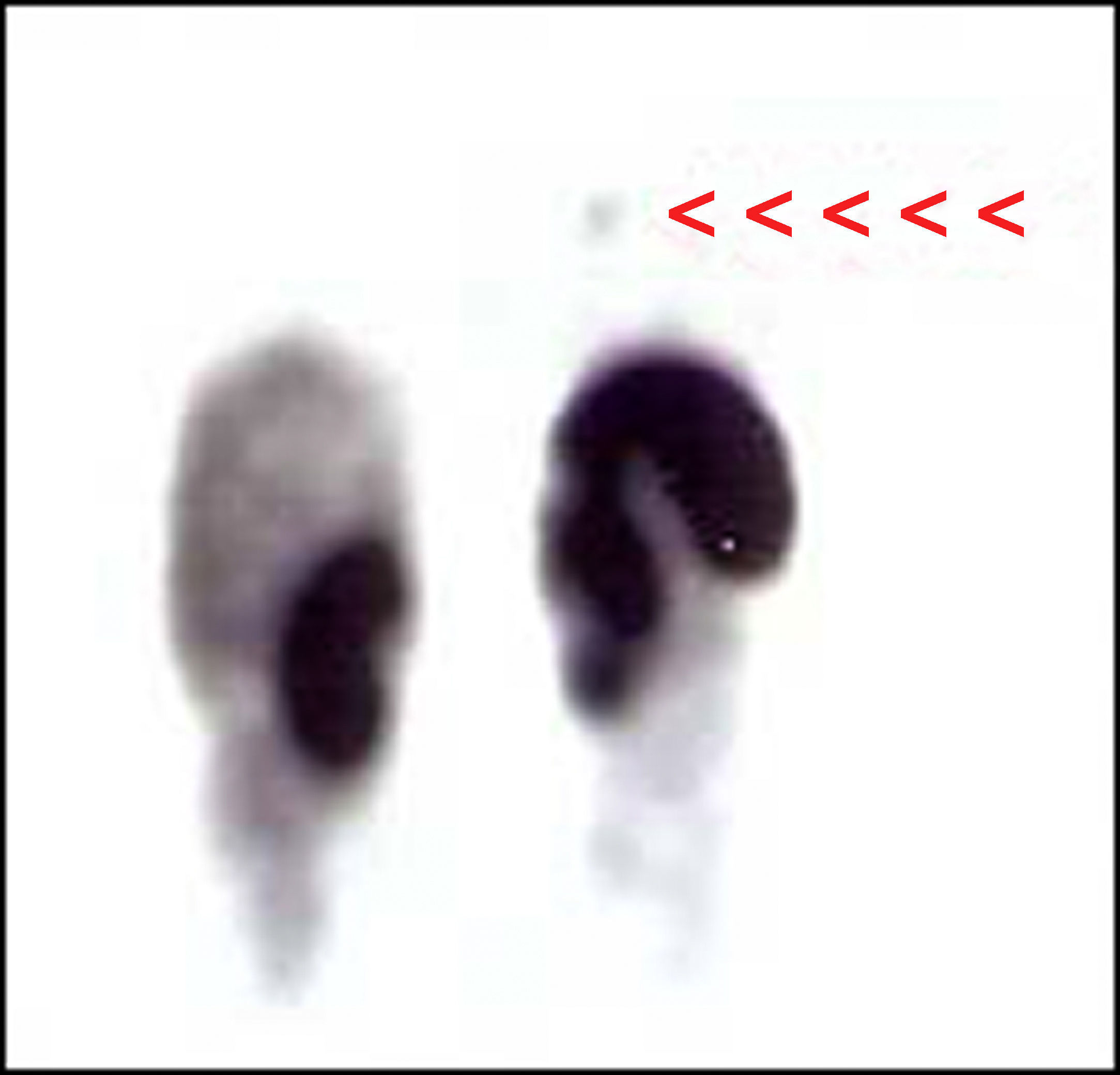
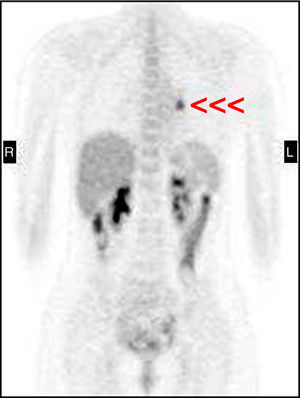
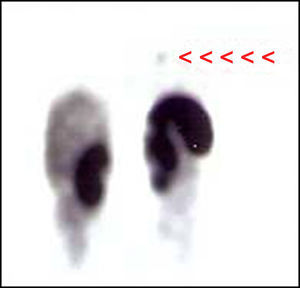
A 27-year-old female patient with an unremarkable personal and family history consulted in 2001 for hirsutism and acne over the previous 6 months. A physical examination revealed a moon face, abdominal striae, central obesity, and muscle atrophy with proximal weakness, all of these signs suggesting hypercortisolism. Supplemental tests showed hyponatremia (2.7mequiv./L), high urinary cortisol levels (947 and 19,746mcg/24h), an absence of plasma cortisol inhibition (17mcg/dL) after dexamethasone 1mg in the evening, a paradoxical response of plasma cortisol after the administration of dexamethasone 8mg as a single evening dose (33mcg/dL), and high ACTH levels (57 and 88pg/mL). Pituitary MRI revealed no lesion, and catheterization of petrosal sinuses showed no gradient. Based on these findings, an ACTH-dependent ectopic Cushing's syndrome (ECS) was considered as the most probable diagnosis. However, both the chest X-rays and pulmonary CT and OctreoScan® were normal. An abdominal CT scan only showed bilateral adrenal hyperplasia. Because of the severe clinical signs of the patient and the impossibility of detecting the origin of the condition, treatment was started with ketoconazole at increasing doses because of persistent poor control. Multiple radiographic examinations (planar OctreoScan®, CT and MRI of chest and abdomen, PET, vaginal US) were periodically performed, always with normal results. Three years later, after rejecting ketoconazole treatment (urinary cortisol 934 and 1321mcg/24h with ketoconazole 600mg/day), laparoscopic bilateral adrenalectomy was performed, resulting in decreased urinary cortisol levels (538–611mcg/24h) and ACTH levels ranging from 266 to 491pg/mL. Finally, in 2007, a 18FDG-PET scan (Fig. 1) showed a pathological 1.5cm deposit in the hilar region of the left lung, which was confirmed by a subsequent OctreoScan-SPECT (Fig. 2). CT and MRI (in STIR sequence) detected this same infrahilar, low uptake, a hyperintense 1-cm nodule suggesting a carcinoid tumor. Based on these findings, a left inferior lobectomy was performed which confirmed the presence of an atypical 1.1-cm BC and a hilar adenopathy with immunohistochemistry positive for ACTH. After surgery, ACTH levels decreased to less than 5pg/mL. The patient remains free of disease three years after surgery.
In the past, ES of ACTH was caused in most cases by small cell lung carcinoma. However, in more recent series BC has been the leading cause. These tumors often pose serious diagnostic1 and localization problems for the following reasons: (1) due to their slow growth, they induce a clinical picture virtually indistinguishable from CS of a pituitary origin, (2) laboratory results are equivocal (plasma cortisol suppression following dexamethasone administration in 50% of cases), the response to metyrapone, moderate ACTH elevations, and (3) most tumors are small (less than 2cm in size), indistinguishable from normal blood vessels, and are therefore difficult to visualize using conventional imaging techniques.1
Imaging techniques routinely used for ECS localization include CT of the chest and abdomen (with special attention to lungs) and MRI. However, these techniques do not achieve diagnosis in 30–50% of cases even after repeated scans over time, and an OctreoScan® is usually performed.2 Since the value of the OctreoScan® depends on the type and degree of expression of somatostatin receptors, on lesion size and location, and on the amount of radioactivity taken up by the lesion, this procedure is not always diagnostic and some tumors stay hidden.3 In the reported case, this could have been due to: (1) the small size of the tumor (although various studies have reported that this variable does not influence positivity in an OctreoScan®1), (2) the initial inhibition of somatostatin receptor expression by elevated hypercortisolism, which decreased following adrenalectomy to a level allowing for receptor expression (although positive results have been reported in some patients with severe hypercortisolism)1, or (3) low receptor expression due to tumor atypia.1
In order to achieve better results, planar OctreoScan® images should be combined with single-photon emission computed tomography (SPECT). This has been shown to clearly improve the sensitivity of planar OctreoScan®. Their association would therefore be useful in the event of a normal OctreoScan® when a neuroendocrine tumor is highly suspected (as occurred in our case) or planar images are difficult to assess.4
18FDG-PET is an essential procedure in oncology used for the detection and monitoring of lesions with intense metabolic activity,3 high proliferation activity, and which are usually poorly differentiated.1 However, since its sensitivity depends on the metabolic turnover of the tumor (which is lower in carcinoids and other slowly growing tumors), BCs have traditionally been considered as 18FDG-PET negative.2 The value of 18FDG-PET in these conditions is currently controversial. Thus, Pacak et al.,2 after analyzing a series of 17 patients with occult ECS (normal MRI/CT), concluded that 18FDG-PET provided no additional information as compared to conventional tests, as it did not detect any tumor not previously detected by CT or MRI. By contrast, there are several cases reported in the literature1,3,5–7 (in addition to our case) where 18FDG-PET (alone or combined with CT) was of value for the localization of occult ECS due to carcinoid tumor. Moreover, various studies have shown its value in detecting neuroendocrine tumors in general (secreting and non-secreting),8,9 mainly atypical ones (showing greater hypermetabolism).10
The development of new tracers for PET (Ga68-DOTA-peptides such as DOTATOC, DOTANOC, and DOTATATE) that specifically bind to somatostatin receptors in neuroendocrine tumors (type 2, type 5 and, to a lesser extent, type 3) will represent a significant change in the monitoring of these tumors.11 The reason for this is that because of their greater spatial resolution (when PET and CT are combined), they have a greater sensitivity for detecting well differentiated neuroendocrine tumors as compared to other imaging techniques. Moreover, Ga68 is a product obtained from a generator instead of a cyclotron, and is therefore easier to produce.
In conclusion, 18FDG-PET, and, in the near future, PET/CT Ga68-DOTA-peptides may be of value for the study of occult ECS when conventional techniques (CT, MRI, OctreoScan®) show normal images or lesions of uncertain significance.
Please cite this article as: Prieto-Tenreiro A, et al. Utilidad del PET-FDG18 en la búsqueda del síndrome de Cushing ectópico por carcinoide bronquial oculto. Endocrinol Nutr. 2011. Endocrinol Nutr. 2011;58(9):497–505.