The current guidelines for treatment of high blood pressure do not include any section dedicated to hypertension in children and adolescents or to cardiovascular disease (CVD) prevention strategies in that age group. Our study was aimed at identifying cardiovascular risk factors (CVRFs) in an adolescent sample.
Subjects and methodsA cross-sectional study of a sample of adolescents aged 12–17years (n=630), conducted from October 2014 to February 2015 in four schools in Cangas do Morrazo (Pontevedra). Sociodemographic variables: age, sex, personal and family history of hypertension and diabetes (DM). Anthropometric variables: body mass index (BMI, kg/m2), waist circumference (WC, cm), waist/height index (WHI), blood pressure (mmHg).
ResultsThe study sample consisted of 295 female and 335 male adolescents (mean age: 13.8±1.4). CVR-related conditions: hypercholesterolemia (7.1%), CVD (1.7%), hypertension (0.8%) and diabetes (0.3%). BMI (22.0±3,8) was higher in males (22.4±3.8 vs 21.0±3.2; p<.01). Overweight was greater in females (27.6% vs 19.7%; p<.05). Seven percent of subjects were obese, 63.8% had systolic BP>P90 and 23.7% had diastolic BP>P90.
Waist circumference positively correlated with age (r=0.1669; p<.0001) and was greater in males (75.4±10.9 vs 72.9±8.9; p<0.01); 27.1% of adolescents had a waist circumference>P75, and 7.5%>P90. Eighty-four (13.3%) adolescents had two CVRFs (overweight+another).
ConclusionsDespite their young age, more than 10% of school children had two CVRFs. Abnormal SBP levels were seen in more than 50%, 20% were overweight, and only 75% had normal waist circumference values.
La hipertensión arterial (HTA) en niños y adolescentes y las estrategias de prevención cardiovascular están poco estudiadas en ese grupo de edad. El objetivo del estudio es conocer los factores de riesgo cardiovascular (RCV) en una muestra de adolescentes.
Sujetos y métodosEstudio observacional transversal de una muestra de adolescentes de 12 a 17años (n=630), realizado entre octubre de 2014 y febrero de 2015 en 4 centros escolares de Cangas do Morrazo (Pontevedra). Variables sociodemográficas: edad, sexo, antecedentes personales y familiares de HTA y diabetes (DM). Variables antropométricas: índice de masa corporal (IMC) (kg/m2), perímetro de cintura (cm), índice cintura/talla (ICT); presión arterial sistólica (PAS) y diastólica (PAD) (mmHg).
ResultadosSe seleccionaron 295 mujeres y 335 hombres. Edad media: 13,8±1,4años. El 68% sin patologías. Patologías relacionadas con RCV: hipercolesterolemia (7,1%), enfermedad cardiovascular (1,7%), HTA (0,8%), diabetes (0,3%). IMC medio: 22,0±3,8, mayor en hombres (22,4±3,8 vs 21,0±3,2; p<0,01). Sobrepeso (IMC>P85) 23,3%, mayor en mujeres (27,6% vs 19,7%; p<0,05). Obesidad: 7%. El 63,8% PAS>P90 y el 23,7% PAD>P90.
El perímetro de cintura se correlaciona de forma positiva con la edad (r=0,1669; p<0,0001) y es mayor entre los hombres (75,4±10,9 vs 72,9±8,9; p<0,01). El 27,1% perímetro de cintura >P75 y el 7,5%, >P90. Un total de 84 (13,3%) adolescentes presentaron 2 factores de RCV (sobrepeso+otro).
ConclusionesPese a su corta edad, más del 10% de los escolares tiene 2 factores de RCV. Más del 50% presentaron valores anormales de PAS, el 20%, sobrepeso, y casi el 25%, valores anormales de perímetro de cintura.
Vascular disease is one of the leading causes of death in industrialized and developing countries.1 In 2012, three out of every 10 deaths worldwide were caused by cardiovascular disease (CVD). This represents 17.5 million deaths, a number equivalent to deaths caused by AIDS, tuberculosis, malaria, diabetes, cancer, and chronic respiratory diseases together.2
A similar situation occurs in Spain where, according to the 2013 national health survey, CVD continues to be the leading cause of death, causing 252 deaths per 100,000 population.3 CVD, infarction, and angina pectoris are the leading cause of death, but with a 3.9% decrease as compared to the previous year. Except in the Canary Islands, Catalonia, Madrid, Navarre, and the Basque Country, where tumors are the leading cause of death, CVD ranks first in all autonomous communities. Galicia is the second community with more deaths due to those conditions (372.8 per 100,000 population) after Asturias (392.7 per 100,000 population).4
Various studies have shown that CVD is a gradual process that starts during the first or second decades of life and eventually causes clinical manifestations at later ages.1
According to data from the last three epidemiological studies on obesity conducted in Spain, PAIDOS,5 RICARDIN,6 and enKid,7 body mass index (BMI) is increasing in children since 1984. In children aged 10years, BMI was 18.1kg/m2 in 1984, 18.5 in 1992, and 18.8 in 1998–2000. In children aged 13years, BMI was 18.4kg/m2 in 1984, 20.4 in 1992, and 21.1 in 1998–2000. This increase, similar to that reported in countries such as France or Switzerland,8 reflects the increase in obesity and overweight in the adolescent population, which is associated to greater cardiovascular risk (CVR).9 Therefore, intervention in children and adolescents may be decisive to prevent, delay, or modify this group of diseases.9
Few studies on CVR in children and adolescents are available in Spain. The most representative European guidelines, such as those of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC) for the treatment of high blood pressure (HBP), do not address this age group, despite the fact that the habits and lifestyles that will be maintained throughout the life of an individual are acquired during childhood and adolescence.9,10
This study, called Vascular Risk in Adolescents from Cangas (RIVACANGAS), is intended to provide relevant data on cardiovascular risk factors (CVRFs) in adolescents in order to implement educational intervention schemes on healthy habits at school.
ObjectivesGeneral objectivesTo ascertain CVRFs in a sample of adolescents from the Morrazo peninsula (Pontevedra).
Specific objectives- •
To collect the demographic characteristics and family history of a sample of adolescents in secondary education.
- •
To assess anthropometric data in relation to standard values.
- •
To identify CVRFs.
A multicenter epidemiological, cross-sectional study.
ScopeConducted from October to February of the 2014–2015 school year at four schools in Cangas do Morrazo (Pontevedra). Information sessions and anthropometric measurements were conducted in January and February 2015.
SubjectsInclusion criteria: adolescents aged 12–17years attending one of the four years of secondary education in any of the Cangas do Morrazo schools whose parents or legal guardians gave informed consent.
Exclusion criteria: non-school attendance on the day of intervention. Refusal to complete the questionnaire and/or anthropometric measurements.
Sample size calculationYoung people account for 5.3% of total population in Cangas (26,567 inhabitants, 13,099 males and 13,468 females). There are 693 males and 702 females aged 12–17years.4 Thus, in order to achieve a precision of 0.04 units in estimation of a mean using a two-sided 95% confidence interval with finite population correction, assuming a standard deviation of 0.50 units and a total population size of 1,395,420 subjects had to be enrolled into the study.
VariablesSociodemographic variables: age, sex, personal and family history of HBP and diabetes mellitus (DM). These were collected from adolescents using a survey.
Anthropometric measurements: weight (kg), height (m), and waist circumference (WC) (cm). BMI (kg/m2) and waist/height ratio (WHR) were calculated. Measurements were made in a separate room with no shoes and light clothes. Calibrated portable scales and stadiometers were used.
Overweight and obesity were defined as presence of BMI values higher than percentiles P85 and P97, respectively, for age and sex according to the reference standards for the general population defined in the Orbegozo Tables.11 To compare data with international studies, BMI was assessed according to the cut-off criteria of +1SD for overweight and from 2SD for obesity, which establishes for subjects aged 2–18years BMI values derived from the limits proposed for adults by the WHO (25kg/m2 for overweight and 30kg/m2 for obesity).12
Waist circumference was measured using a tape in contact with skin, exerting no pressure and with a relaxed abdomen, above the upper border of the iliac crest. The cut-off point corresponding to percentiles P75 and P90, the values best associated to insulin resistance, the underlying factor for type 2 diabetes mellitus and CVD in children, was used.13
The WHR was calculated. A WHR greater than 0.5 is a CVRF14 Percent fat was calculated based on WHR.16
Blood pressure (BP) measurement: recorded as systolic blood pressure (SBP)/diastolic blood pressure (DBP) (in mmHg). Two validated and calibrated Omron M3® oscillometric sphygmomanometers were used. After a 5-min rest, BP was measured two times with a 3-min interval and the mean was calculated.17 Altered BP levels or pre-hypertension were defined as BP values >P90 for age, sex, and height,18 while SBP and/or DBP values ≥P95 were considered HBP.
Results were anonymously recorded in an ad hoc form including all questionnaires administered.
ProcedureThe managers of all seven schools providing secondary education in Cangas do Morrazo were contacted in September 2014. They were proposed the conduct of the study and a complementary lecture on CVR and healthy lifestyle. Four schools (two public and two private) agreed to participate in the study. Their managers informed the parents about the project and requested their approval for participation of their children by signing an informed consent. Refusal of students to participate was respected.
On the day established by the manager to conduct the study, data collection forms were distributed to and anonymously completed by students. Anthropometric and BP measurements were taken at a different room in students who had already completed the survey.
In the weeks subsequent to the study, adequate hygienic and dietary habits were addressed in informative talks at the schools.
Data analysisG-Stat 2.0® software (GlaxoSmithkline) was used. Qualitative data are given as percentages, and quantitative data as mean±standard deviation (SD). Ninety-five percent confidence intervals (CIs) were calculated. A Chi-square test, or a Fisher test for small samples, was used to compare proportions. To compare means, a Student's t test was used for normally distributed variables (Kolmogorov test with Lilliefors corrections), and nonparametric Mann–Whitney U or Wilcoxon tests were used for normally distributed variables. Correlations were tested using Pearson's r or Spearman's rho depending on whether they were parametric or nonparametric. A value of p<0.05 was considered statistically significant.
ResultsSample characteristicsThe sample consisted of 630 students (295 girls and 335 boys), 5.5% of those attending the four schools participating and 56.7% of all students of the same age group in Cangas do Morrazo.
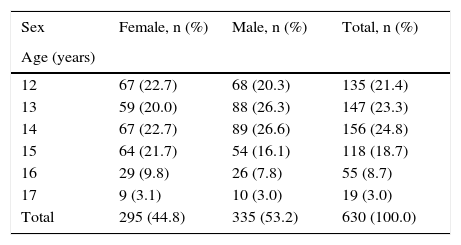
Mean age was 13.8±1.4years, with no difference between sexes. Table 1 shows distribution by age.
Age distribution of the sample.
| Sex | Female, n (%) | Male, n (%) | Total, n (%) |
|---|---|---|---|
| Age (years) | |||
| 12 | 67 (22.7) | 68 (20.3) | 135 (21.4) |
| 13 | 59 (20.0) | 88 (26.3) | 147 (23.3) |
| 14 | 67 (22.7) | 89 (26.6) | 156 (24.8) |
| 15 | 64 (21.7) | 54 (16.1) | 118 (18.7) |
| 16 | 29 (9.8) | 26 (7.8) | 55 (8.7) |
| 17 | 9 (3.1) | 10 (3.0) | 19 (3.0) |
| Total | 295 (44.8) | 335 (53.2) | 630 (100.0) |
Forty-five adolescents (31.8%) reported some health problem. Problems related to CVR included hypercholesterolemia in 45 students (7.1%), cardiovascular disease in 11 (1.7%), HBP in 5 (0.8%), and DM in two students (0.3%). History of HBP and DM in first-degree relatives was reported by 17.2% and 5.9% of students respectively. History of DM in second-degree relatives was reported by 18.3% of students.
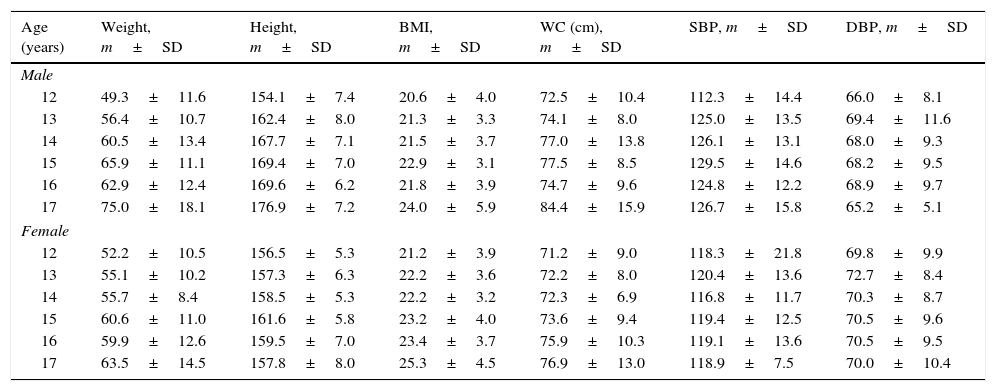
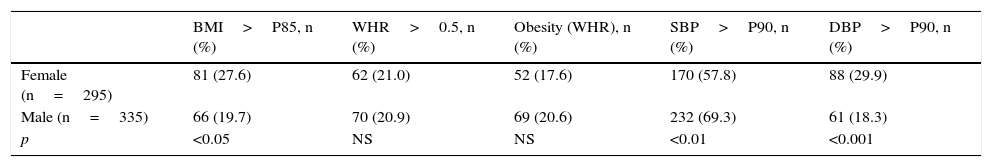
Anthropometric dataTable 2 shows the anthropometric measurements by sex and age. Table 3 shows the proportion of adolescents with abnormal anthropometric data.
Anthropometric measurements.
| Age (years) | Weight, m±SD | Height, m±SD | BMI, m±SD | WC (cm), m±SD | SBP, m±SD | DBP, m±SD |
|---|---|---|---|---|---|---|
| Male | ||||||
| 12 | 49.3±11.6 | 154.1±7.4 | 20.6±4.0 | 72.5±10.4 | 112.3±14.4 | 66.0±8.1 |
| 13 | 56.4±10.7 | 162.4±8.0 | 21.3±3.3 | 74.1±8.0 | 125.0±13.5 | 69.4±11.6 |
| 14 | 60.5±13.4 | 167.7±7.1 | 21.5±3.7 | 77.0±13.8 | 126.1±13.1 | 68.0±9.3 |
| 15 | 65.9±11.1 | 169.4±7.0 | 22.9±3.1 | 77.5±8.5 | 129.5±14.6 | 68.2±9.5 |
| 16 | 62.9±12.4 | 169.6±6.2 | 21.8±3.9 | 74.7±9.6 | 124.8±12.2 | 68.9±9.7 |
| 17 | 75.0±18.1 | 176.9±7.2 | 24.0±5.9 | 84.4±15.9 | 126.7±15.8 | 65.2±5.1 |
| Female | ||||||
| 12 | 52.2±10.5 | 156.5±5.3 | 21.2±3.9 | 71.2±9.0 | 118.3±21.8 | 69.8±9.9 |
| 13 | 55.1±10.2 | 157.3±6.3 | 22.2±3.6 | 72.2±8.0 | 120.4±13.6 | 72.7±8.4 |
| 14 | 55.7±8.4 | 158.5±5.3 | 22.2±3.2 | 72.3±6.9 | 116.8±11.7 | 70.3±8.7 |
| 15 | 60.6±11.0 | 161.6±5.8 | 23.2±4.0 | 73.6±9.4 | 119.4±12.5 | 70.5±9.6 |
| 16 | 59.9±12.6 | 159.5±7.0 | 23.4±3.7 | 75.9±10.3 | 119.1±13.6 | 70.5±9.5 |
| 17 | 63.5±14.5 | 157.8±8.0 | 25.3±4.5 | 76.9±13.0 | 118.9±7.5 | 70.0±10.4 |
SD, standard deviation; BMI, body mass index; DBP, diastolic blood pressure; SBP, systolic blood pressure; WC, waist circumference.
Proportion of students with abnormal BMI, WHR, and BP data.
| BMI>P85, n (%) | WHR>0.5, n (%) | Obesity (WHR), n (%) | SBP>P90, n (%) | DBP>P90, n (%) | |
|---|---|---|---|---|---|
| Female (n=295) | 81 (27.6) | 62 (21.0) | 52 (17.6) | 170 (57.8) | 88 (29.9) |
| Male (n=335) | 66 (19.7) | 70 (20.9) | 69 (20.6) | 232 (69.3) | 61 (18.3) |
| p | <0.05 | NS | NS | <0.01 | <0.001 |
WHR, waist/height ratio; BMI, body mass index; NS, not significant; BP, blood pressure; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Mean BMI of the sample was 22.0±3.8, with higher BMI in males (22.4±3.8 vs 21.0±3.2; p<0.01). The proportion of adolescents with BMI higher than P85 was 23.3%, and was higher in females (27.6% vs 19.7%; p<0.05) Prevalence rates of overweight and obesity were 16.3% and 7.0% respectively. Using Cole criteria, 15.8% of students were overweight and 5.3% were obese. There were no adolescents with malnutrition.
WC positively correlated to age (Pearson's r=0.1669; p<0.0001) and was greater in males (75.4±10.9 vs 72.9±8.9; p<0.01).
Percent fat estimated from WHR was 25.9±4.9 in females and 20.6±6.8 in males. No significant difference was seen between males and females.
WC exceeded P75 in 27.2%. Central obesity, as defined by WC greater than P90, was found in 7.5% of students (Table 4).
Mean WHR was 0.46±0.06, with no difference between sexes. Twenty-one percent of students had WHR greater than 0.5 (20.9% of males, 21.0% of females), with no significant sex or age differences.
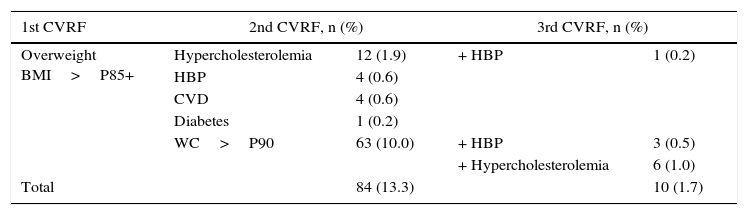
Table 5 shows the number of students with more than one CVRF (overweight, abdominal obesity, diabetes, HBP, hypercholesterolemia, or cardiovascular disease). There were 84 adolescents (13.3%) with two CVRFs (overweight+any other) and 10 adolescents (1.7%) had three CVRFs.
Adolescents with one or more cardiovascular risk factors.
| 1st CVRF | 2nd CVRF, n (%) | 3rd CVRF, n (%) | ||
|---|---|---|---|---|
| Overweight BMI>P85+ | Hypercholesterolemia | 12 (1.9) | + HBP | 1 (0.2) |
| HBP | 4 (0.6) | |||
| CVD | 4 (0.6) | |||
| Diabetes | 1 (0.2) | |||
| WC>P90 | 63 (10.0) | + HBP | 3 (0.5) | |
| + Hypercholesterolemia | 6 (1.0) | |||
| Total | 84 (13.3) | 10 (1.7) | ||
CVD, cardiovascular disease; CVRF, cardiovascular risk factor; HBP, high blood pressure; BMI, body mass index; WC, waist circumference.
SBP above the 90th percentile was found in 63.8% of students, while 23.7% had DBP values above the 90th percentile. Table 2 shows the mean BP values of the sample stratified by age.
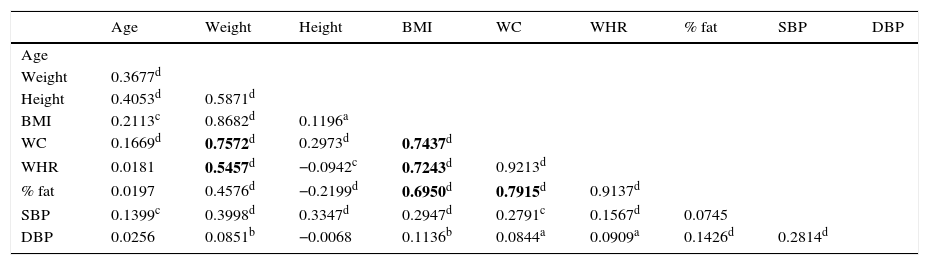
Table 6 details the correlations found between the different CVRFs. There was a high moderate correlation between WC and weight, between WC and WHR, between BMI and WHR, and between BMI and WC.
Correlations between the different anthropometric variables.
| Age | Weight | Height | BMI | WC | WHR | % fat | SBP | DBP | |
|---|---|---|---|---|---|---|---|---|---|
| Age | |||||||||
| Weight | 0.3677d | ||||||||
| Height | 0.4053d | 0.5871d | |||||||
| BMI | 0.2113c | 0.8682d | 0.1196a | ||||||
| WC | 0.1669d | 0.7572d | 0.2973d | 0.7437d | |||||
| WHR | 0.0181 | 0.5457d | −0.0942c | 0.7243d | 0.9213d | ||||
| % fat | 0.0197 | 0.4576d | −0.2199d | 0.6950d | 0.7915d | 0.9137d | |||
| SBP | 0.1399c | 0.3998d | 0.3347d | 0.2947d | 0.2791c | 0.1567d | 0.0745 | ||
| DBP | 0.0256 | 0.0851b | −0.0068 | 0.1136b | 0.0844a | 0.0909a | 0.1426d | 0.2814d |
WHR, waist/height ratio; BMI, body mass index; DBP, diastolic blood pressure; SBP, systolic blood pressure; WC, waist circumference.
Study limitations in relation to studies previously conducted in Spain, included the age intervals considered, which differ from those in some other studies, making comparison of results difficult. An additional limitation is self-reporting of health problems by the surveyed students, which is not always reliable, particularly at earlier ages. For the same reason, another limitation would be that blood glucose and lipid profile tests were not performed, and the study therefore relied on statements by adolescents for these factors.
No agreement exists in epidemiological studies on the cut-off points of BMI that define obesity in children. According to current consensus in Europe and Asia, obesity is defined as BMI greater than P97, and overweight as BMI values between P85 and P97, the limits used in this study. Mean BMI was 22.0±3.8, greater than in the Carmona study19 on adolescents aged 9–17 years, where BMI was 21.0±3.9 and significantly lower in males (22.4±4.7) as compared to females (23.2±5.5). In our study, however, BMI was significantly greater in males (22.4±3.8) than in females (21.0±3.2), which agrees with data reported in the 2010 AFINOS study.9
Prevalence of overweight+obesity in our study was 23.3%, with 7% obesity and 16.3% overweight. Prevalence was significantly greater in females (27.6% vs 19.7% in males; p<0.05), in contrast to the findings in the EnKid study,7 which reported prevalence rates of 31.2% in adolescents aged 10–13 years and 21.8% in those aged 14–17 years, with higher values in males. Our study does not agree with that of Serra Majem et al.7 in BMI values by age. In our study, BMI shows a mild-moderate increase with age, as occurs in the reference population,11 but this does not occur in the Serra-Majem et al. study.20
Our results as regards overweight and obesity are lower than those reported in a study conducted in Granada21 that found prevalence rates of overweight and obesity of 23.0% and 12.7% in girls and 20.8% and 5.0% in boys respectively.
The prevalence of obesity found, 7.0%, is clearly lower than the 13.7% reported by Rubio et al.22 in a similar population (18–5% in males and 9.1% in females) using the same criteria defining overweight and obesity at the 85th and 97th percentiles of BMI respectively. A comparison with international studies using the same percentile criteria but the Cole et al. Tables,12 would provide higher obesity rates in our study, but we consider more adequate the values obtained according to reference standards for our population.11
Assessment of obesity based on BMI is a widely used method, but is an indirect estimation of percent body fat.23 This is the reason why calculation of obesity as a function of percent fat from WHR values16 results in prevalence rates higher than estimated with BMI, with both being associated to biochemical changes related to CVR.24
WC is an anthropometric variable predicting CVR,25,26 because it determines fat distribution.13,27 WC is less widely used in pediatric populations, and no population standards are available, but the values recorded in this study are similar to those found in the AFINOS study9 and by Martínez-Gómez et al.25 WC values >P90, considered as central obesity, were found in 7.5% of adolescents, with similar proportions in both sexes. Abdominal obesity, reported in 22.7% of adolescents in some studies,28 is a very important CVRF which, together with other CVRFs such as HBP, causes the start of atherosclerotic conditions at these ages.29 Prevalence of central obesity was relatively low in our study, but impaired BP was more prevalent.
Mean WHR was below the limit of 0.5 considered as a CVRF.14 There were no significant differences between sexes.
No WHR standards adapted to our population are available, but a high correlation was found to BMI, in agreement other authors15 who showed a good correlation of this parameter with other indirect methods to measure obesity.
HBP is a CVRF clearly related to presence of obesity.30 More than half the students in our sample (63.8%) had SBP values above the 90th percentile, and almost one fourth (23.7%) had DBP values above such percentile. Increased DBP is more common in females, while high SBP values are more common in males. These results agree with those reported by Martínez-Gómez et al.25 and are higher than those found by Martín et al.19 in adolescents aged 15–17 years with mean SBP and DBP values of 99.6mmHg and 55.0mmHg respectively.
One out of six adolescents in the sample reports first-degree relatives with HBP, almost 6% have first-degree relatives with diabetes, and almost 10% report that they have a disease or CVRF. Caution should be taken with these data, because adolescents do not always have an adequate knowledge of the diseases of their parents, and surveys were conducted in the absence of the parents.
In this study, 13.3% of adolescents had two CVRFs and 1.7% had three CVRFs. These numbers should cause concern, as this is a sample of pre-adults aged 12–17years. Hypercholesterolemia, HBP, obesity, central abdominal fat (WHR), and high SBP values were more common in males, while overweight and high DBP values predominated in females.
A significant prevalence of CVRFs, especially HBP, overweight, and hypercholesterolemia, was found in the adolescent sample analyzed. Despite their short age, more than one out of every 10 adolescents had two CVRFs. Based on these results, it is concluded that immediate and continued educational interventions aimed at improving habits and lifestyles are required to prevent progression to cardiovascular disease and type 2 diabetes mellitus in adult age.
Protection of research people and animalsThe authors state that no experiments with humans or animals have been conducted in this research. The authors state that all procedures used met the regulations of the relevant ethics research committee and the World Medical Assembly and the Declaration of Helsinki.
No personal data have been stored. As a minor sample was recruited, written consent was obtained from the parents or legal guardians of the participants. Data required for the study were managed in aggregate form, with no individual identification of subjects.
FundingThe study was not funded by any person or company other than the research group.
AuthorshipRMG contributed to study conception and design, data interpretation, writing of draft article and critical review of contents, and final approval of the submitted version.
PGR contributed to data collection, analysis and interpretation, writing of draft article, and final approval of the submitted version.
MFC contributed to data collection, analysis and interpretation, writing of draft article, and final approval of the submitted version.
ARR contributed to data collection, analysis and interpretation, writing of draft article, and final approval of the submitted version.
NVC contributed to data analysis and interpretation, writing of draft article, and final approval of the submitted version.
NFAR contributed to study conception and design, data analysis and interpretation, writing of draft article, and final approval of the submitted version.
JAFP contributed to study conception and design, data analysis and interpretation, writing of draft article, and final approval of the submitted version.
IRE contributed to study conception and design, data interpretation, writing of draft article and critical review of contents, and final approval of the submitted version.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Mera-Gallego R, García-Rodríguez P, Fernández-Cordeiro M, Rodríguez-Reneda Á, Vérez-Cotelo N, Andrés-Rodríguez NF, et al. Factores de riesgo cardiovascular en adolescentes escolarizados (RIVACANGAS). Endocrinol Nutr. 2016;63:511–518.