Necrosis in a normal anterior pituitary, although rare, can be seen in routine autopsy series (1–5%), and is more common in patients who have been supported with artificial ventilation before death (∼20%).1–3 In brain-dead patients, pituitary necrosis is invariably observed.4–7 In virtually all cases where pituitary necrosis is found at autopsy, the main histological feature of the necrosis is coagulative infarction, which is only partial and mostly in the center of the anterior pituitary. Here we report complete anterior pituitary infarction in a patient with hypothermia, cardiovascular arrest, and brain death.
A 61-year-old African American female was admitted for resection of multifocal colorectal cancer. She had had no significant past medical history; preoperative physical examination had been unremarkable except for low body mass index (BMI, 17.4kg/m2). The surgical resection was open and extensive, and lasted for 8.5h. Total estimated blood loss was 1050mL and 8000mL of lactated Ringers solution were given cumulatively. At the beginning of anesthesia, her temporal temperature was 36.6°C. Forty minutes later, her esophageal temperature was 35.5°C. A steady drop of temperature started at 5h into the anesthesia, reaching a nadir of 32.3°C near the end of anesthesia, in spite of the use of a warming blanket and raising the room temperature as much as possible. The patient, however, was reportedly able to open eyes and follow simple commands and otherwise stable after anesthesia completion. She remained intubated and was transferred to intensive care unit within 20min. Upon arrival she was bradycardic and severely hypothermic with a temperature of 27.8°C. She was given atropine; within a few minutes she became pulseless with narrow-complex ventricular tachycardia, requiring cardiopulmonary resuscitation for 4min with 5 cardioversions. She resumed normal sinus rhythm but remained comatose. Cardiac arrest was believed to be due to hypothermia rather than primarily cardiogenic. Coagulopathy, acidosis, bilateral pleural effusions and acute congestive heart failure developed within a few hours after cardiopulmonary resuscitation, and required pressor support. Her core temperature rose to about 36.7°C after 5h of warming measures. Cortisol levels were not measured and she did not receive corticosteroids. On postoperative day 1, the neurological team determined that the patient had suffered from brain death, attributed to multiple causes including advanced cancer, anesthesia, pain medications, hypoxia, electrolyte abnormality and hypothermia, but not hypoperfusion during cardiac arrest. Head CT was considered but the patient was too unstable to be taken to the imaging department to undergo the procedure. On postoperative day 3, she was extubated and expired shortly thereafter (extubation was delayed to give the family time to accept the brain death).
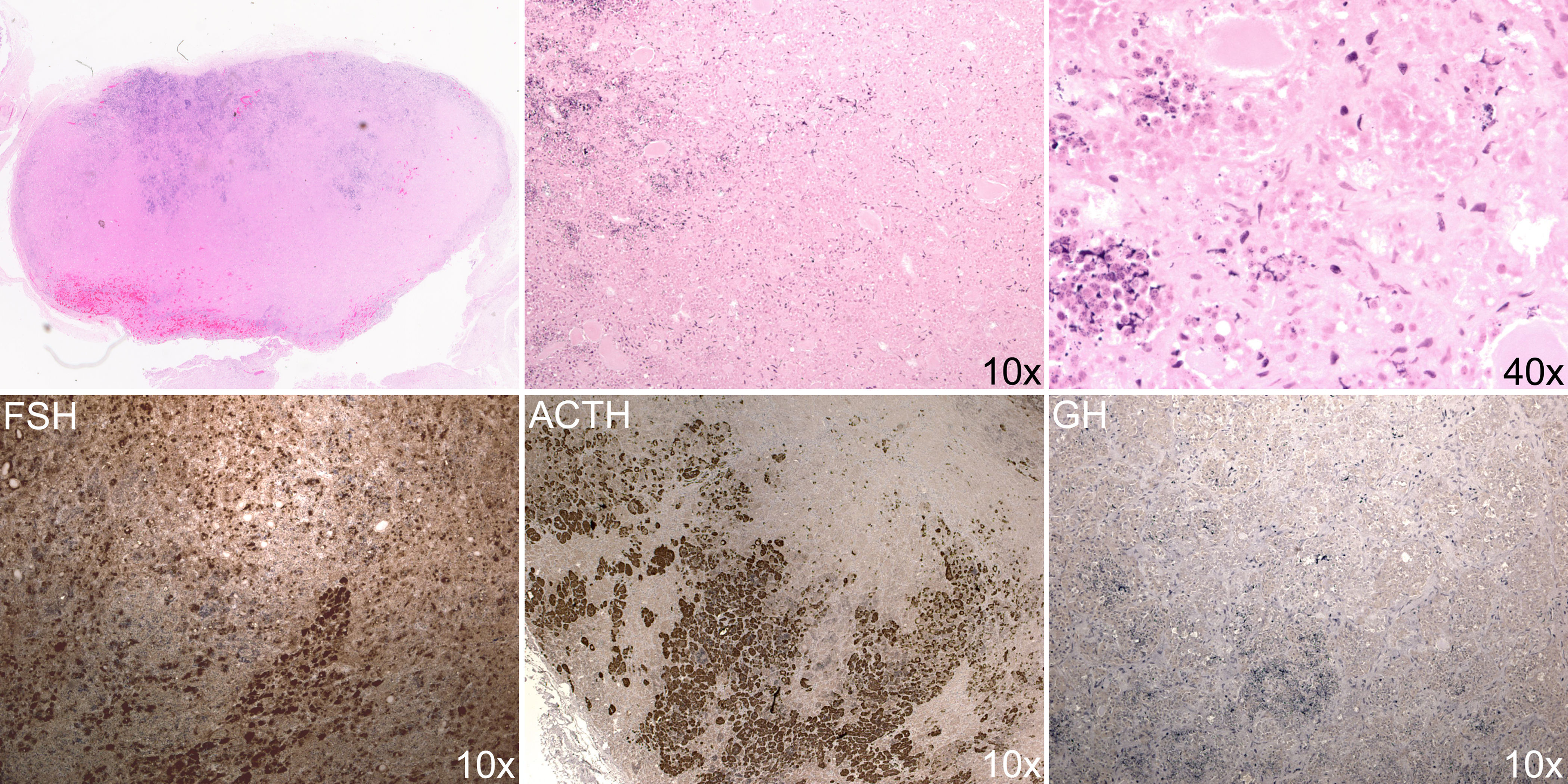
An autopsy was performed within 10h after bodily death to search for the cause of profound hypothermia. General autopsy results were unremarkable; there was no evidence of coronary events; the thyroid and adrenal glands showed no signs of atrophy. Grossly, the brain exhibited diffuse cerebral edema and gray discoloration without focal lesions identified in hypothalamus; the pituitary gland appeared unremarkable. Microscopically, the brain exhibited diffuse anoxic or ischemic changes. The pituitary gland showed complete infarction of the anterior lobe (Fig. 1). There was no evidence of pituitary adenoma, as demonstrated by the preservation of acinar architecture with reticulum stain (not shown) and the presence of mixed population of pyknotic anterior pituitary cells. Although immunostaining for FSH, LH, ACTH, and TSH were largely preserved (FSH and ACTH are shown) and prolactin was nearly absent as expected in a postmenopausal woman, GH staining was completely lost (Fig. 1). There was no hemorrhage or infiltration by neutrophils or macrophages.
Histology of the postmortem pituitary. Upper panels: hematoxylin and eosin staining. Upper left: whole anterior pituitary which measured 10mm×6mm. The whole anterior pituitary was replaced by amorphous material (upper left and upper middle panels) and pyknotic cells (upper right panel). Lower panels: immunostains for FSH, ACTH and GH.
We have thus described complete anterior pituitary infarction in an adult female patient with hypothermia, cardiovascular arrest, and brain death. Pituitary infarction per se is not surprising in this brain-dead patient who has been on artificial ventilation for 3 days before autopsy, as pituitary coagulative infarction (necrosis) is well known in all brain-dead patients and in nearly one fifth of all patients who have been on artificial ventilation before death.3–7 To the best of our knowledge, complete pituitary infarction has not been reported previously together with relatively well-preserved brain structure, or in a patient who has been brain dead for only a few days; the finding is surprising as pituitary should be well preserved even after 21 days of brain death, and its total necrosis seems to occur only after 28 days of brain death.6 The exact timing of her complete pituitary infarction deserves consideration. As the patient was clinically well preoperatively and both thyroid and adrenal glands were normal at autopsy, she most likely had normal pituitary preoperatively. It is possible that pituitary necrosis occurred intraoperatively. Although the patient had a few risk factors for intraoperative hypothermia such as low body mass index, prolonged anesthesia, and complicated surgery,8 appropriate intraoperative warming measures were provided and the extent of hypothermia is very unusual. No hypothalamic lesions that could explain the hypothermia were found in autopsy. Adrenal insufficiency and hypopituitarism are well known but rare causes of hypothermia.9 The patient's complete pituitary infarction, if occurring intraoperatively, could certainly cause hypopituitarism and acute adrenal insufficiency and contribute to the profound hypothermia.
Alternatively, the complete pituitary infarction may have occurred postoperatively. Both artificial ventilation and brain death experienced by the patient are known to be associated with pituitary infarction.3–7 The mechanisms for ventilator-associated pituitary infarction are not clear, while in brain death it is suggested to be due to the absence of blood supply to the center of pituitary due to increased intracranial pressure secondary to brain edema; the preservation of the glandular periphery is explained by its extracranial blood supply.3,5 The patient's complete pituitary infarction would require stoppage of any blood supply to the gland, including extracranial components. As pituitary hormone immunostaining is preserved beyond a week after brain death,7 this patient's intact pituitary hormone staining cannot be used as evidence of recent pituitary infarction. The patient's profound hypothermia may have contributed to the complete pituitary infarction as serum GH levels, a potential marker of pituitary necrosis, are higher in patients who died of hypothermia,5,10 and she indeed had total lack of GH-positive cells in the pituitary.
In summary, we here report a very unusual complete pituitary infarction in a patient with profound intraoperative hypothermia and brain death. If it occurred intraoperatively, the complete pituitary infarction could partly explain the intraoperative hypothermia; if it occurred postoperatively, the complete pituitary infarction may be attributed to hypothermia, the full causes of which would remain obscure.