The high incidence of nodular thyroid pathology has led to growing concern about the economic impact that this pathology represents on the healthcare system. There are conclusive data about the cost-effectiveness of high-resolution units for nodular thyroid pathology; however, their implementation is not homogeneous in the Endocrinology and Nutrition services of our country. The objective of the present study was to evaluate the economic impact of the implementation of the high-resolution thyroid nodule unit (HRTNU) in our center.
Patients and methodsThe present work is a prospective, observational and descriptive study carried out in 1314 patients (82% women, mean age 58 years ds = 11) evaluated at the HRTNU during the period of August 2022–August 2023. Demographic data (age and sex) were analyzed, referral center and consultation type, number of total consultations and neck ultrasound performed, number of fine needle aspiration (FNAB) performed, and cytology results were analyzed.
ResultsIn the period from August 2022 to August 2023, a total of 1314 patients were evaluated (neck ultrasound and clinical consultation) and a total of 133 FNAB were performed, of which only 2.26% were non-diagnostic. Compared to the percentage of unsatisfactory FNAB from the previous year August 2021–July 2022 of 25%, a mean saving of 9931.43 euros was estimated. 84.47% of the patients evaluated for the first time by the HRTNU were discharged, estimating a mean saving of 133,200 euros.
ConclusionsThe implementation of a HRTNU at the Endocrinology and Nutrition departments, coordinated with primary and specialized care, is a cost-effectiveness alternative, as it reduces the number of medical consultations and is accompanied by a higher rate of diagnostic FNAB.
La alta incidencia de la patología nodular tiroidea ha hecho que crezca la preocupación sobre el impacto económico que representa esta patología sobre el sistema sanitario. Existen datos concluyentes acerca del coste efectividad de las unidades de alta resolución de patología nodular tiroidea, sin embargo, su implantación no es homogénea en los servicios de Endocrinología y Nutrición de nuestro país. El objetivo del presente estudio fue evaluar el impacto económico de la puesta en marcha de la unidad de alta resolución de nódulo tiroideo (UARNT) en nuestro centro.
Pacientes y métodosEl presente trabajo es un estudio prospectivo, observacional y descriptivo en 1314 (82% mujeres, una edad media de 58 de = 11.) evaluados en la UARNT durante el periodo de Agosto 2022–Agosto 2023. Se analizaron datos demográficos (edad y sexo), especialidad de derivación, número de visitas totales realizadas, número de punción con aspiración de aguja fina (PAAF) realizadas y resultados de la citología.
ResultadosEn el periodo de estudio se valoraron un total de 1314 pacientes (ecografía y visita clínica) y se realizaron un total de 133 punciones con aguja fina (PAAF) de las cuales solo un 2,26% fueron no diagnósticas. Comparado con el porcentaje de PAAF insatisfactorias del año anterior (Agosto 2021–Julio 2022) del 25%, se estimó un ahorro de 9.931,43 euros. El 84,47% de los pacientes valorados por la UARNT fueron dados de alta en el mismo acto, estimando un ahorro de 133.200 euros.
ConclusionesLa implantación de la UARNT en los servicios de Endocrinología y Nutrición coordinada con Atención Primaria y especializada es una alternativa coste eficaz, al reducir el número de visitas médicas y asociar una mayor tasa de punciones diagnósticas.
Nodular thyroid disease is one of the most prevalent conditions encountered by Endocrinology services in their routine clinical practice. The prevalence of nodular thyroid disease is said to affect nearly 60% of the population, depending on the mode of detection (palpation or imaging), being more prevalent among women, obese, and elderly patients.1
Of note that the incidence of nodular thyroid disease has been increasing over the years due to the diagnosis of subclinical disease (non-palpable nodules) in association with the increasingly widespread use of imaging modalities such as ultrasound, MRI, CT, and PET in the routine clinical practice.2–4
This increase in the incidence rate of thyroid nodules has raised concerns on the financial impact of this disease on the health care system. In countries such as the United States, the annual cost related exclusively to the diagnosis of nodular thyroid disease is estimated at $25.1 billion.5 Besides the direct costs associated with the disease, there are indirect costs associated with the inconveniences caused to the patient, such as loss of work hours, resulting in financial harm.5,6
Cervical ultrasound is the imaging modality of choice for screening nodular thyroid disease due to the accessibility and high-resolution capacity of current machines.1,7 Since most thyroid nodules are benign, the main goal in evaluating nodular thyroid disease should be to clearly determine its clinical significance, distinguishing benignity from malignancy, and avoiding overdiagnosis and overtreatment of these lesions.8
Moreover, to adequately evaluate thyroid nodules, a comprehensive approach is necessary (clinical and biochemical evaluation by the endocrinologist, ultrasound and cytological evaluation when indicated). Endocrinologists play a central role in managing the thyroid nodule, as they are responsible for integrating all diagnostic information to make proper decisions regarding clinical management.9,10 Therefore, in 2004, the American Thyroid Association (ATA) encouraged all endocrinologists in their editorial of Thyroid to conduct standardized thyroid ultrasounds in patients without relying on external services.11
In Spain, same as it happens in other units developed in several services such as cardiac rehabilitation units and cardiovascular risk units, various endocrinology and nutrition services have integrated thyroid disease into high-resolution thyroid nodule units (HRTNU), where patients are evaluated comprehensively by integrating ultrasound and fine needle aspiration (FNA) into their routine services.12 The development of these units has proven to be cost-effective by accelerating medical care, improving the quality of perceived health care, and reducing the number of visits, imaging modalities, and non-diagnostic punctures for nodular disease.6,13
However, the implementation of HRTNUs in Spain remains variable and, in many cases, is not coordinated with primary care services.13
To highlight and emphasize the importance of high-resolution units, our work aims to demonstrate the financial viability of these units by presenting the results of the first year of operation of Hospital Verge de la Cinta de Tortosa HRTNU (reference center of the territorial management of Terres de l’Ebre, Catalonia).
Materials and methodsPatients and methodsThis work is a prospective, observational, and descriptive study aimed at analyzing the financial impact of the Endocrinology and Nutrition service HRTNU of Hospital Verge de la Cinta de Tortosa from its implementation in August 2022 until August 2023. This study has been approved by Institut d’Investigació Sanitària Pere Vergili Drug Research Ethics Committee (reference 098/2023).
All patients with nodular thyroid disease referred from primary care centers in the territorial management of Terres de l’Ebre, from our center specialized care, and from 2 hierarchical hospitals (Hospital Comarcal d’Amposta and Hospital Comarcal de Mora d’Ebre) were evaluated.
The HRTNU was created back in August 2022 as a structural requirement of the endocrinology and nutrition service to address 2 issues: to alleviate the diagnostic delay of requested thyroid ultrasounds, and to reduce the high percentage of unsatisfactory punctures at the center.
The HRTNU was launched due to a coordinated and protocolized model of the Endocrinology service with collaboration from the departments of Radiology, Pathological Anatomy, and primary care, following this scheme:
- 1
The risk assessment scale used by both the high-resolution and radiology units is the ACR TI-RADS scale proposed by the American College of Radiology.14
- 2
Initial ultrasound evaluation of clinically significant thyroid nodules (>1 cm of major diameter) by the HRTNU.
- 3
Ultrasound follow-up of malignant disease by the HRTNU, including preoperative staging ultrasounds for thyroid cancer and ultrasound follow-up of thyroid carcinomas.
- 4
Ultrasound follow-up of benign disease treated with minimally invasive techniques for thyroid nodules (ethanol ablation of cystic nodules and radiofrequency ablation of solid thyroid nodules) by the HRTNU.
- 5
Coordinated follow-up of thyroid nodules with benign ACR TI-RADS 3 cytological results. Benign ACR TI-RADS 3 thyroid nodules are followed for 2.5 years by the HRTNU and, if clinically and radiologically stable, they are discharged with a clinical report and a recommendation to primary care to request a follow-up ultrasound with radiology in 2.5 years for a complete 5-year follow-up. Cystic or spongiform ACR TI-RADS thyroid nodules 1 < 1 cm are monitored by primary care and radiology and, if they grow, they are referred to the HRTNU. Thyroid nodules with benign ACR TI-RADS 4 cytology are followed for a total of 3 years by the HRTNU and discharged with a recommendation to primary care to request a follow-up ultrasound in 2 years for a complete 5-year follow-up. Thyroid nodules with benign ACR TI-RADS 5 cytology are followed for a total of 4 years by the HRTNU and discharged with a recommendation to primary care to request a follow-up ultrasound in 1 year to complete a 5-year follow-up.
To improve the efficiency of this organizational model, referrals that arrive at the HRTNU from primary and specialized care are screened by a team of physicians from the Endocrinology and Nutrition. Referrals arrive electronically along with a referral report that includes the physical examination, the biochemical and immunological profile of thyroid function, and, if available, a radiological report. During screening, the indication for the thyroid ultrasound and the priority of the appointment are analyzed. If necessary data for assessment purposes are missing, or referral is made without a clinical report, the inter-consultation goes back to the general practitioner or specialized physician to complete the initial report required for an appropriate screening of nodular thyroid disease.
The high-resolution thyroid nodule consultation is led by a physician from the Endocrinology and Nutrition service with 4 years of prior training in thyroid ultrasound and ultrasound-guided FNA incorporated into the Endocrinology and Nutrition MIR training program at Hospital Universitario Son Espases, where progressive supervised learning in thyroid ultrasound (anatomical aspects and risk assessment scales for the management of nodular thyroid disease) and technical aspects, both diagnostic (ultrasound-guided FNA) and therapeutic (minimally invasive techniques for the treatment of benign thyroid disease, such as ethanol ablation of cystic nodules and radiofrequency ablation of solid nodules) was conducted. The number of ultrasound-guided FNAs on record during the training period was 168, and the estimated number of thyroid ultrasounds, 371. The high-resolution consultation is conducted once a week and is divided into 2 modules:
- 1
Morning module, in which 12 patients with nodular thyroid disease previously screened and eligible for a diagnostic puncture are scheduled. Each visit lasts 30 min.
- 2
Afternoon module, in which 17 patients with nodular thyroid disease are scheduled, including 2 initial visits for screening nodular disease (cases with a questionable ultrasound-guided FNA indication), 3 patients being monitored for thyroid cancer, and 12 patients for nodular thyroid disease with benign cytology. Initial visits and thyroid cancer follow-ups last 30 min, while follow-up visits for benign thyroid nodules last 20 min. Within the first 6 months of operation, an additional afternoon module was structured with 17 patients, each visit lasting 15 min, to perform the pending cervical ultrasounds from the previous year (from August 2021 through July 2022).
In each module, a comprehensive clinical, analytical, and ultrasound evaluation is conducted. Patients without criteria for FNA or follow-up are discharged during the same visit. The ultrasound is performed using a Philipps Affiniti 50G ultrasound machine with a linear probe L12-5 9–14 MHz. The FNA is performed with 21G needles attached to a flexible plastic extension system to avoid using a Cameco by aspirating the material by capillarity. If the material is not easily aspirated by capillarity, a 10 mL syringe is used for aspiration purposes. The sample is, then, sent to the Pathological Anatomy department, where it is processed (a clot is obtained, fixed in 10% buffered formalin, embedded in paraffin, serially sectioned, and stained with hematoxylin-eosin). Additionally, samples for cytology are obtained and stained with Papanicolaou and Diff-Quick in both direct smear and liquid cytology (Thin Prep). Two cytotechnicians and 5 pathologists are involved in the process of preparing and analyzing the samples.
Study variables, cost savings estimation, and effectivenessDemographic data (age and sex), referral specialty, total number of visits, total number of discharges by the HRTNU, number of follow-up visits by the HRTNU, number of ultrasound-guided FNAs performed by the HRTNU, and cytology results (benign, malignant, suspicious for malignancy, atypia of undetermined significance, suspicion of follicular neoplasm, and insufficient sample) from the cytologies performed by the HRTNU were analyzed. Information on the number of FNAs performed 1 year before the unit was implemented (from August 2021 through July 2022) and the percentage of unsatisfactory punctures was obtained from the Pathological Anatomy unit. The number of ultrasounds performed (from August 2021 through July 2022) was obtained from the Radiodiagnosis service.
To estimate the potential financial impact of the unit, direct costs related to unperformed medical care were considered, as well as the theoretical costs stipulated by the Institut Català de Salut for a follow-up endocrinology visit and a thyroid ultrasound. Additionally, the costs associated with performing ultrasound-guided FNAs (cost per needle, 10 mL syringe, and materials used for smear and cytology staining as stipulated by Institut Català de la Salut) were calculated to evaluate the potential cost savings associated with reducing unsatisfactory punctures.
Statistical analysisThe total and per capita costs of the first visit for each intervention were calculated, adding the cost of all necessary materials for both the HRTNU and the Radiodiagnosis service. Similarly, the cost of follow-up visits was estimated for both the HRTNU and Radiology. These costs were compared by calculating the cost difference and the percentage change rate.
We conducted a descriptive analysis of the frequency and percentage of unsatisfactory and diagnostic FNA results depending on whether they were performed by the HRTNU or Radiodiagnosis. The Cohen's Kappa index was calculated to assess concordance between the HRTNU and Radiodiagnosis results.
For the sensitivity analysis, 2 incidence rate estimates of thyroid cancer were considered (5 cases/100,000 inhabitants-year and 10 cases/100,000 inhabitants-year).
The statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 20.0 for Windows, assuming a statistical significance of P < .05.
ResultsDuring the first year of operation of the HRTNU, the Endocrinology and Nutrition service of Hospital Verge de la Cinta took over most requested thyroid ultrasounds for a total of 1314 patients being evaluated. A total of 85% of the patients seen were women, with a mean age of 58 years (SD, 11) (Table 1).
Activity of the HRTNU at Hospital Verge de la Cinta from August 2022 through August 2023.
| Total HRTNU visits (n = 1314) | |
|---|---|
| Sex, women, % | 82% |
| Age, mean (SD) | 58 (SD, 11) |
| Direct discharges, first visit discharge (%) | 1110 (84.47%) |
| Follow-up visits, follow-up visit (%) | 204 (15.53%) |
| Source of first visits, number of first visit requests (%) | Primary care: 1202 (91.47%) |
| Specialized care: 112 (7.7%) | |
| Total patients evaluated | 1314 |
SD, standard deviation.
Most patients were referred from primary care (91.47%) vs 7.7% who referred from specialized care. A total of 84.47% of all patients evaluated were discharged during the same visit without a follow-up consultation (1110 patients), while 15.53% of patients (204) were still monitored in the high-resolution unit in the morning (ultrasound-guided FNAs) or afternoon module (follow-up thyroid ultrasounds). Demographic data and HRTNU activity are shown in Table 1.
Table 2 compares the 2 follow-up circuits for nodular thyroid disease (HRTNU vs Radiodiagnosis). During the previous year (August 2021–July 2022), when thyroid ultrasound was not still centralized in the HRTNU, a total of 719 patients with nodular thyroid disease were studied at our center, which accounts for 45.59% fewer patients compared with the HRTNU activity displayed the next year. Although the number of ultrasound-guided FNAs was similar in the 2 circuits (133 vs 100), the number of unsatisfactory punctures was lower in favor of the high-resolution unit (2.26% vs 25%), thus meeting the requirement of <10% unsatisfactory punctures stipulated by clinical practice guidelines.1 There was no agreement between both diagnostic circuits (Kappa index −0.175, P < .001), showing differences, which were favorable to the HRTNU. Finally, the mean waiting time for a thyroid ultrasound was also lower and favorable to the HRTNU (30 days [SD, 7.31] vs 90 days [SD, 11.2]).
Comparison between HRTNU activity (August 2022–August 2023) and Radiodiagnosis (August 2021–July 2022).
| HRTNU (August 2022–August 2023) | Radiodiagnosis (August 2021–July 2022) | |
|---|---|---|
| No. of patients evaluated | 1314 | 719 |
| No. of FNAs performed | 133 | 100 |
| Percentage of unsatisfactory FNAs (%) | 3 (2.26%) | 25 (25%) |
| Cohen's Kappa Index | −0.175* | |
| Delay time until thyroid ultrasound, mean (SD) | 30 (SD, 7.31) days | 90 (SD, 11.2) days |
SD, standard deviation; FNA, fine needle aspiration; HRTNU, high-resolution thyroid nodule unit.
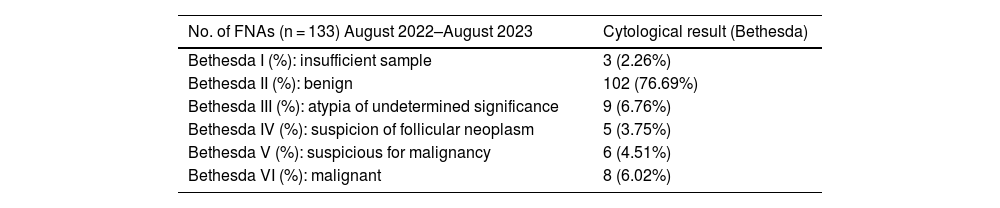
Table 3 shows the distribution of cytology results performed by the HRTNU from August 2022 through August 2023 based on the Bethesda system.
Results of cytologies of thyroid nodules subjected to FNA by the HRTNU from August 2022 through August 2023.
| No. of FNAs (n = 133) August 2022–August 2023 | Cytological result (Bethesda) |
|---|---|
| Bethesda I (%): insufficient sample | 3 (2.26%) |
| Bethesda II (%): benign | 102 (76.69%) |
| Bethesda III (%): atypia of undetermined significance | 9 (6.76%) |
| Bethesda IV (%): suspicion of follicular neoplasm | 5 (3.75%) |
| Bethesda V (%): suspicious for malignancy | 6 (4.51%) |
| Bethesda VI (%): malignant | 8 (6.02%) |
Considering the potential financial savings derived from the implementation of the HRTNU, Table 4 illustrates the cost savings associated only with not performing follow-up thyroid ultrasounds and successive visits to the Endocrinology and Nutrition service. From August 2022 through August 2023, an estimated ;133,200 were saved by avoiding 1110 follow-up thyroid ultrasounds and successive visits to Endocrinology.
Estimation of potential direct cost savings in the HRTNU single-visit medical and ultrasound model.
| HRTNU | n | % | Cost/Euros |
|---|---|---|---|
| Number of patients evaluated | 1314 | ||
| Direct discharges (ultrasounda + visitb) | 1110 | 84.47% | −;133,200.00 |
| Follow-up visits (ultrasounda + visitb) | 204 | 15.53% | ;24,480.00 |
HRTNU, high-resolution thyroid nodule unit.
On the other hand, Table 5 illustrates the cost savings derived from reducing unsatisfactory punctures since the ultrasound-guided FNA became centralized in the HRTNU. The cost of each unsatisfactory puncture (considering the costs of the materials used for puncture and sample processing) is estimated at ;451.43. From August 2022 through August 2023, the HRTNU had a 2.26% rate of unsatisfactory punctures, resulting in an annual cost of ;1354.28 due to repeated punctures with unsatisfactory results. Considering the 25% rate of unsatisfactory punctures during the previous period (from August 2021 through July 2022), the overall cost savings from reducing unsatisfactory FNAs is ;9931.43. Overall, the HRTNU allowed a 46.69% reduction from unsatisfactory FNAs at our center.
Estimation of potential direct cost savings related to fewer non-diagnostic FNAs by the HRTNU.
| Radiodiagnosis (August 2021–July 2022) | HRTNU (August 2022–August 2023) | |
|---|---|---|
| No. of unsatisfactory punctures | 25 | 3 |
| No. of diagnostic punctures | 75 | 130 |
| Percentage of unsatisfactory FNAs (%) | 25% | 2.26% |
| Cost of FNAsa + ultrasoundb + visitc | ;11,285.71 | ;1354.28 |
| Total savings | −;9931.43 |
FNA, fine needle aspiration.
Overall, assuming cost savings associated with avoiding follow-up thyroid ultrasounds and successive visits (−;133,200) and reducing unsatisfactory punctures (−;9931.43), the total estimated cost savings associated with the implementation of the HRTNU is ;143,131.43.
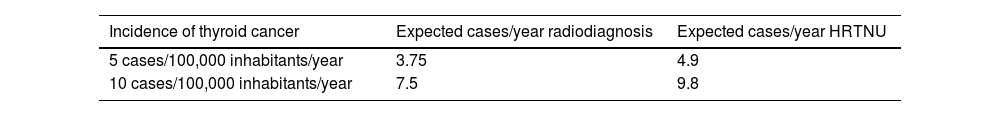
To evaluate the clinical impact of the HRTNU, a sensitivity analysis was performed, considering 2 different scenarios of incidences of differentiated thyroid cancer.
- •
Scenario #1 (incidence of 5 cases/100,000 inhabitants-year): incidence estimated by the ATA.1
- •
Scenario #2 (incidence of 10 cases/100,000 inhabitants-year): incidence of differentiated thyroid cancer while the HRTNU was in full operation, that is, from August 2022 through August 2023 with a reference population of 200,000 inhabitants.
The results of sensitivity analysis are presented in Table 6. In both scenarios, the implementation of the HRTNU correlating with the low percentage of unsatisfactory FNAs presents a higher diagnostic rate of differentiated thyroid carcinoma vs the diagnostic rate of the Radiodiagnosis service.
DiscussionProper management of nodular thyroid disease is crucial for Endocrinology and Nutrition services, as it is one of the most common reasons for referral. The approach to nodular thyroid disease should not only be associated with the highest level of technical expertise but also be accompanied by an effective organizational structure that allows for prompt patient care to correctly rule out malignant disease without elevating costs.1
The results of our study support the hypothesis that HRTNUs can reduce the costs associated with nodular thyroid disease through comprehensive assessments of thyroid nodules in a single visit.
Firstly, the reduced number of avoided visits and examinations by the unit resulted in direct cost savings of ;133,200, related to the reduced number of requested ultrasounds and successive visits. Díaz-Soto et al.13 reported annual savings of ;70,000 related to an increased number of direct discharges performed by the high-resolution unit, along with fewer requested ultrasounds and clinical follow-ups. Similarly, a different study conducted by Carral et al.15 estimated annual direct savings of ;94,441.36.
One of the main aspects related to nodular thyroid disease is the high number of referrals and examinations related to low-complexity disease. Based on this, a significant part of cost savings associated with the development of high-resolution units is associated with the high percentage of direct discharges. Díaz Soto et al.13 reported a direct discharge percentage of 21.1% within the first year of the high-resolution unit work, while Castells et al.16 reported a higher percentage of 42.3%. In our study, this percentage is much higher (84.47%) and is mainly associated with 2 aspects:
- 1
An elevated number of requested cervical ultrasounds without adequate clinical screening (absence of biochemical tests and/or cervical physical examination).
- 2
A high percentage of benign thyroid nodules with stable clinical and radiological conditions for more than 5 years, for which cervical ultrasound was requested.
Of note that the HRTNU took over most pending cervical ultrasounds not yet performed by the Radiodiagnosis service, which justifies the nearly 50% increase in thyroid ultrasound demand during the first year HRTNU was operational vs the previous year.
Therefore, the proposed referral and follow-up system will be crucial in evaluating the costs associated with the unit implementation. On the one hand, the telematic referral system allows for better screening of thyroid nodules without FNA or follow-up criteria (spongiform and cystic nodules without clinical symptoms and subcentimeter nodules), as long as it fully complies with the principles established by the protocol (biochemical evaluation, physical examination, and radiological report, if available). On the other hand, the comprehensive care model offered by the unit (clinical and radiological) allows patients to visit the hospital less frequently, resulting in cost savings in working hours.
Secondly, the lower number of non-diagnostic punctures resulted in direct cost savings of ;9931.43. We should mention that the effectiveness of the HRTNU largely depends on the physicians’ knowledge and technical ability to evaluate the risk of nodular thyroid disease by ultrasound and comply with current recommendations of <10% unsatisfactory punctures¹. In this regard, Tofé-Povedano et al.10 demonstrated that the number of diagnostic punctures increases exponentially with gained experience. In a different study published by Castells et al.,16 the rate of unsatisfactory FNAs dropped by 20.7% after the implementation of ultrasound in the HRTNU.
In our own experience, the lower number of unsatisfactory punctures is due not only to the fact that physicians responsible for performing FNAs have prior formal training with a 4-year experience performing thyroid ultrasounds and ultrasound-guided FNAs, but also to improvements in the referral and sample processing circuit with the Pathological Anatomy service.
When thyroid punctures did not depend on the HRTNU, longer delays were reported between the FNA and sample processing, which eventually increased the number of unsatisfactory punctures as thyroid cells were prone to greater desiccation processes. These technical aspects are all gone after the HRTNU was implemented, as the consultation is now held on a fixed day each week, and the Pathological Anatomy service knows that it must act quickly and in coordination with the HRTNU.
Thirdly, the delays experienced in the diagnostic process of nodular thyroid disease are shorter when centralized in a single service. Within the first year of HRTNU operation, the mean waiting time from the appointment request to the unit evaluation was 30 days (SD, 7.31). These results are shorter than the mean waiting time within the previous year (August 2021–July 2022), when the management of cervical ultrasound did not depend on the Endocrinology service. Additionally, these results are consistent with those reported by Díaz Soto et al.13 of mean waiting times of 36.5 days (SD, 1.1).
The main limitation of this study is that the costs derived from the change in the referral and request system for thyroid ultrasound by primary and specialized care since the HRTNU implementation have not been evaluated yet. The implementation of a prior telematic screening (based on clinical, analytical, and radiological criteria) has eliminated a significant amount of requested ultrasounds for functional thyroid disease (Hashimoto's disease) and nodules that are, by definition, benign (asymptomatic cystic or spongiform nodules), as well as solid nodules with benign FNA that have been followed for 5 years without any clinical changes being reported. Additionally, the costs related to the lower number of core needle biopsies (CNBs) performed since the HRTNU inception have not been evaluated either.
In conclusion, this study supports the idea of improved health care resulting from implementing a HRTNU in terms of costs. On the one hand, it reduces costs by decreasing the number of clinical visits and requested cervical ultrasounds and, in experienced hands, it reduces the percentage of unsatisfactory punctures. In this regard, the development of the HRTNU in our center is justified not only by cost reduction but also by the clinical impact associated with the reduced rate of unsatisfactory punctures being performed, which allows for a higher detection rate of thyroid carcinomas (sensitivity analysis).
Finally, we would like to emphasize that the role of HRTNUs should not only be limited to diagnosis but also to treating nodular thyroid disease. In this regard, in line with other Spanish groups, we have integrated minimally invasive techniques (ethanol ablation of cystic thyroid nodules and radiofrequency ablation of solid thyroid nodules) for the treatment of nodular thyroid disease within the HRTNU.17–19
FundingNone declared.
Conflicts of interestNone declared.