Recurrent laryngeal nerve injury ranges from 1.4 to 5.1% following surgery involving the thyroid gland. Some associated risk factors include extensive lymphadenectomy, thyroid carcinoma, Graves’ disease and re-intervention. The introduction of ultrasound in daily practice offers advantages such as safe examination, easy reproducibility, and rendering real time imaging, inter alia. This article describes the use of ultrasound in the evaluation of the recurrent laryngeal nerve via the visualization of the vocal folds.
ObjectiveTo describe the use of ultrasound in thyroidectomy for evaluation of the recurrent laryngeal nerve via the vocal-fold movement.
ResultsThe article discusses 2 female patients undergoing thyroidectomy due to different gland pathologies. Before the start of the surgical procedure, vocal fold mobility was evaluated in real time using ultrasound. The recurrent laryngeal nerve was identified during surgery and the integrity of the vocal fold mobility was again assessed during phonation under ultrasound visualization.
ConclusionsUltrasound may be a tool for the evaluation of the recurrent laryngeal nerve in surgical procedures involving the thyroid gland.
La lesión del nervio laríngeo recurrente va desde el 1,4 al 5,1% tras cirugías que comprometen la glándula tiroides. Existen factores de riesgo como cirugías asociadas a linfadenectomía extensas, carcinoma tiroideo, enfermedad de Graves y reintervenciones. La llegada del ultrasonido a la práctica diaria ofrece ventajas como ser un examen seguro, de fácil reproducción y brindar imágenes en tiempo real entre otras. En este trabajo se hace la descripción de su uso para la valoración del nervio laríngeo recurrente mediante la visualización de las cuerdas vocales.
ObjetivoDescribir la utilidad del ultrasonido en tiroidectomía para la evaluación del nervio laríngeo recurrente mediante la movilidad de las cuerdas vocales.
ResultadosSe describen los casos de 2 pacientes de sexo femenino sometidas a tiroidectomía por diferentes patologías glandulares. Antes de iniciar el procedimiento quirúrgico se realiza valoración de la movilidad de las cuerdas vocales en tiempo real bajo visión ecográfica. Durante la cirugía se identifica el nervio laríngeo recurrente y al finalizar el procedimiento nuevamente se revisa la integridad de cuerdas vocales mediante movilidad durante la fonación bajo visión ecográfica.
ConclusionesEl ultrasonido puede ser una herramienta en la valoración del nervio laríngeo recurrente en cirugías que comprometen la glándula tiroides.
The use of ultrasound is becoming increasingly important in the daily practice of anesthesia, not only to assist in peripheral nerve blocks, but also in the ICU and ER environments. Some of the major advantages of this diagnostic and therapeutic tool are easy use at the patient's bedside, reproducible images and, above all, real time renderings.
The purpose of this case report – with prior approval by the institution's medical ethics committee – is to describe the benefits of ultrasound in airway evaluation, particularly for real time vocal-fold assessment to determine the integrity of the recurrent laryngeal nerve following thyroidectomy.
A systematic literature review was performed based on Ovid, Pubmed, and Cochrane database search; the terms used in the search included: “laryngeal nerve”, “ultrasonography”, and “thyroid”. The initial search was limited to human articles, meta-analyses, reviews and random articles.
The main search yielded 114 articles from which only the documents describing the thyroid ultrasound approach, studies to assess the vocal-fold paralysis and the evaluation of the recurrent laryngeal nerve were selected.
Case 1A 47-year-old female patient scheduled for subtotal left thyroidectomy due to multinodular goiter and a history of primary high blood pressure, dyslipidemia and obesity; functional class I/IV. The patient was on metoprolol, amlodipine, furosemide, atorvastatin, and fluoxetine. The physical examination showed a body weight of 85kg and a BMI of 36kg/m2. The airway evaluation resulted in Mallampati II, TMD less than 6cm, and mouth opening 4cm. A slightly oversized thyroid gland at the expense of the left lobe, no midline deviation, and no difficult airway predictors were observed. The rest of the physical workup did not show relevant findings.
The anesthetic induction was administered with propofol 160mg, 4ng/ml TCI remifentanil, neuromuscular relaxation with succinylcholine 150mg; there were no complications during the orotracheal intubation. Maintenance of anesthesia was with desflurane or remifentanil. During the surgical procedure, the surgeon visualized the recurrent laryngeal nerve. The patient was extubated awake at the end of the procedure with no complications.
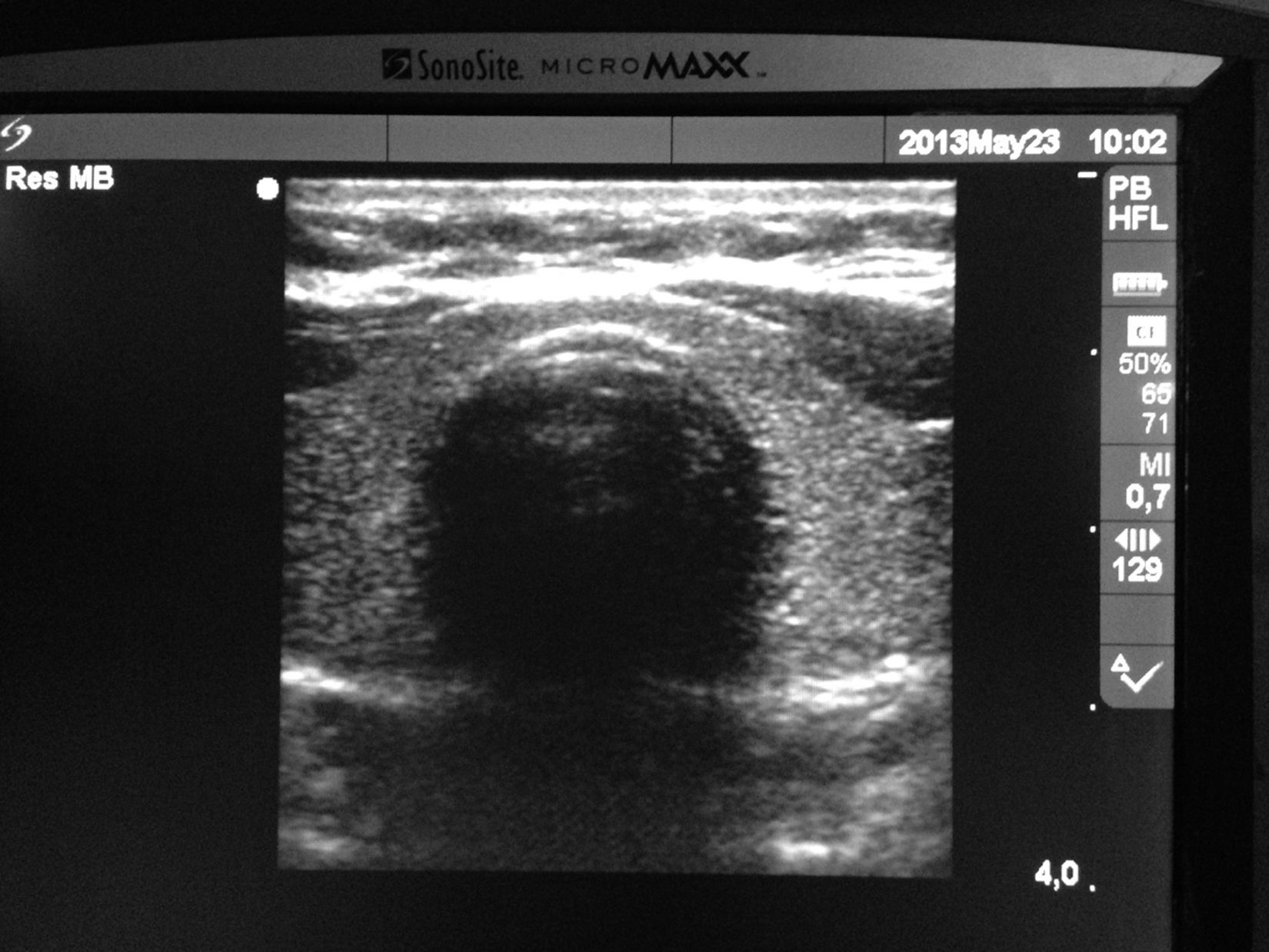
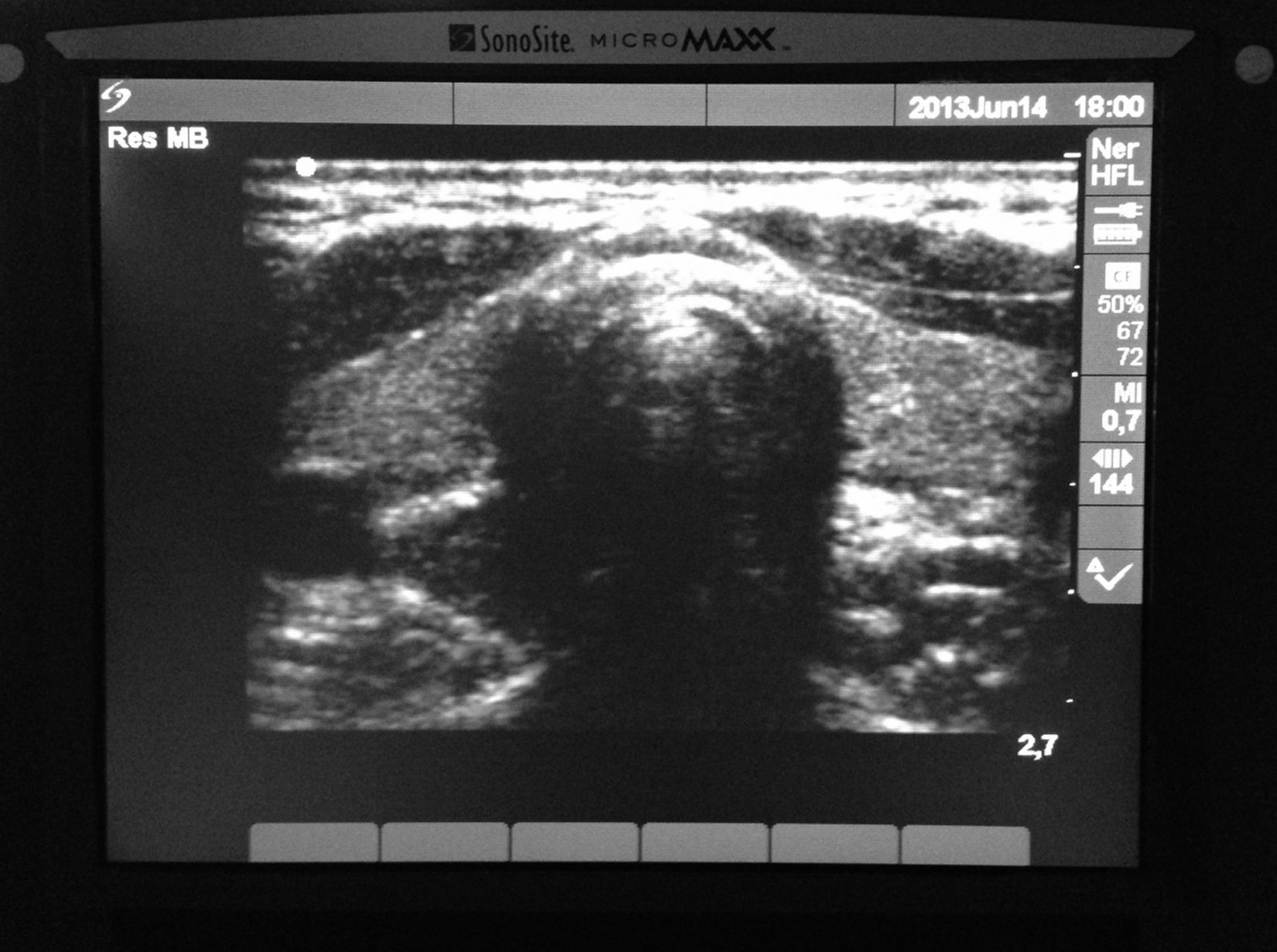
Prior to the induction of anesthesia, several structures including the tracheal rings, the carotid artery and the internal jugular artery (Fig. 1) were identified under ultrasound vision with a lineal transducer (6–13MHz, Sonosite Micromaxx) perpendicular to the trachea; the transducer slides into a cephalic position to identify the thyroid cartilage and the vocal folds. During phonation the vocal folds express bilateral movement (Fig. 2).
At the end of the procedure the patient was awake and an ultrasound evaluation was performed with a lineal transducer visualizing the trachea, the thyroid cartilage and the vocal folds, which are once again assessed for total bilateral mobility during phonation. The patient did not exhibit any clinical nerve injury and was then transferred to post-anesthesia care free of complications.
Case 2A 49-year-old female patient scheduled for subtotal thyroidectomy due to a thyroid nodule with a history of vertigo and ENT treatment, functional class I/IV. The patient had been receiving diphenhydramine, metoclopramide, and nimodipine. The physical examination indicated a body weight of 58kg and a BMI of 24kg/m2. The airway examination resulted in Mallampati I, TMD 6cm, and mouth opening 4cm. Symmetric neck and absence of difficult airway predictors were observed on examination. The rest of the examination showed no alterations.
The anesthetic induction was administered using lidocaine 40mg, propofol 120mg, and rocuronium 10mg; there were no complications during the orotracheal intubation. The maintenance of anesthesia was accomplished with 0.2μg/kg/min remifentanil and desflurane. During the surgical procedure, the surgeon visualized the recurrent laryngeal nerve. The patient was extubated awake at the end of the procedure with no complications.
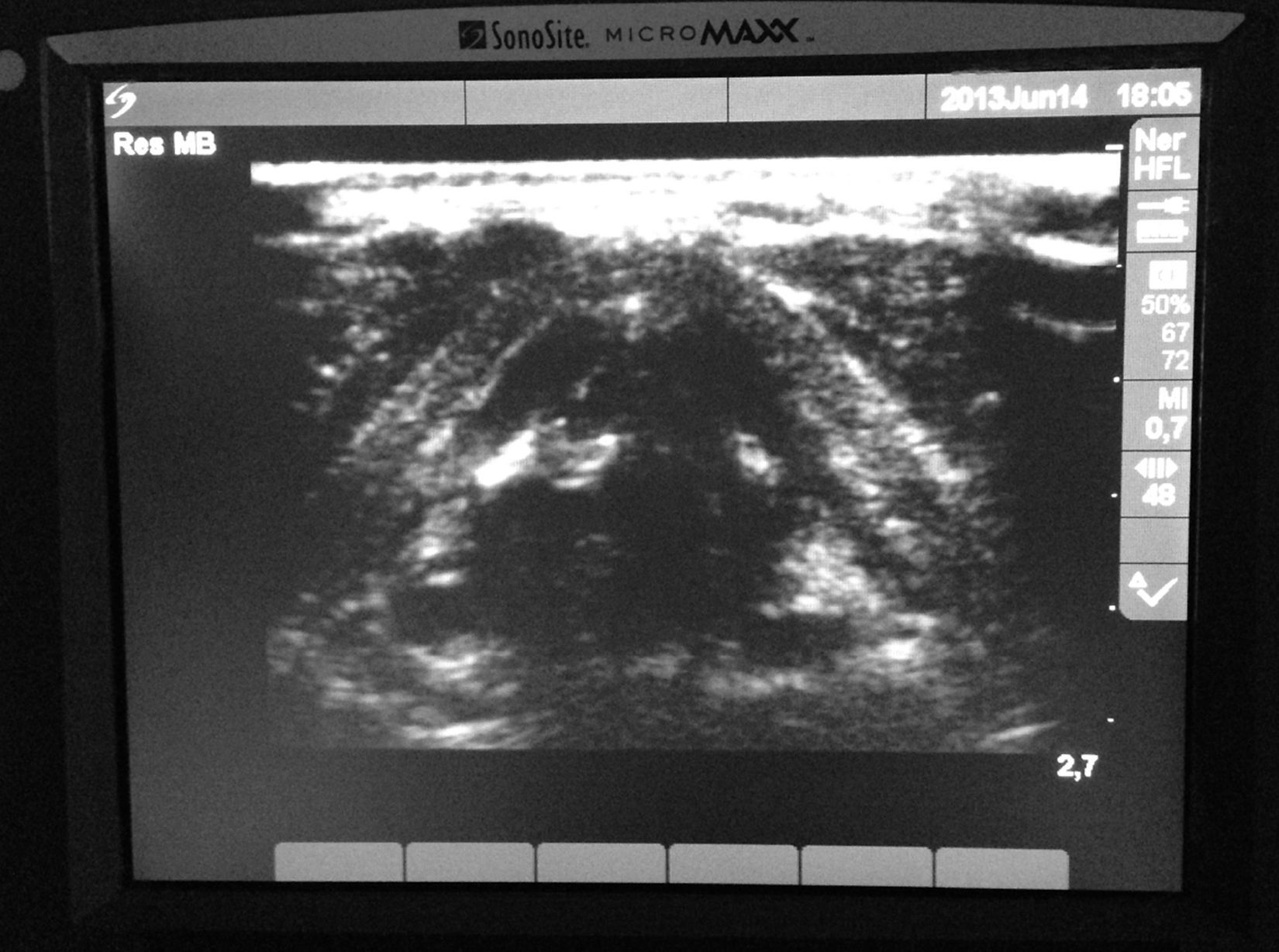
Prior to the induction of anesthesia, several structures including the tracheal rings, the carotid artery and the internal jugular artery (Fig. 1) were identified under ultrasound vision with a lineal transducer (6–13MHz, Sonosite Micromaxx) perpendicular to the trachea; the transducer slides into a cephalic position to identify the thyroid cartilage and the vocal folds (Fig. 3). During phonation the vocal folds expressed bilateral movement.
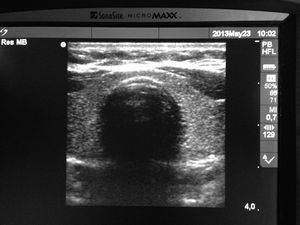
At the end of the procedure the patient was awake and an ultrasound evaluation was performed with a lineal transducer visualizing the trachea, the thyroid cartilage and the vocal folds, which are once again assessed for total bilateral mobility during phonation (Fig. 4). The patient did not exhibit any clinical nerve injury and was then transferred to post-anesthesia care free of complications.
DiscussionFor surgeries involving the thyroid gland, general anesthesia is preferable because of amnesia, immobility, and airway control.1 In most cases the airway control is achieved using orotracheal intubation; however, since preserving the integrity of the recurrent laryngeal nerve is crucial to these surgical approaches,2 the use of the laryngeal mask has also been described for it provides advantages in terms of intraoperative visualization of vocal fold mobility under direct vision using the fibroscope. Hillermann et al., suggest the use of small diameter orotracheal tubes (5.0mm inner diameter) together with a laryngeal mask to position the fibrobronchoscope. This mechanism allows for adequate airway control concurrent with direct monitoring of the recurrent laryngeal nerve.3
The incidence of unilateral and temporary recurrent laryngeal nerve injury following thyroid surgery ranges from 1.4% to 5.1%.4 The incidence of permanent lesions ranges from 0.4 to 0.9%. Some risk factors include thyroid carcinoma surgery, re-interventions, Graves’ disease or extensive lymphadenectomies; there have even been some cases of transient paralysis following infiltration of the surgical wound with local anesthesia in thyroidectomies.5 Identifying the recurrent laryngeal nerve and documenting its integrity during surgery have been associated with a lower probability of transient postoperative injury.6 If the recurrent laryngeal nerve is injured, the complication usually arises during the immediate postoperative period as airway obstruction attributable to reduced diameter of the glottis, secondary to ipsilateral paralysis of the vocal folds. In the presence of unilateral injury, usually the respiratory involvement is not severe; however, if the lesion is bilateral, there may be total glottis closure and complete respiratory obstruction requiring orotracheal intubation.
Several methods have been described to monitor the recurrent laryngeal nerve and other nerves such as the upper lateral laryngeal nerve branch that controls the vocal folds and the cricothyroid muscles.7,8 Most techniques require direct stimulation or total visualization. Usually this function is determined by the following: (1) direct visualization under the fibro bronchoscope; (2) palpation of the larynx during stimulation of the recurrent laryngeal nerve; (3) laryngeal muscles electromyography; (4) electromyography with orotracheal tube inserted electrodes. Monitoring of the recurrent laryngeal nerve usually impacts the anesthetic technique used, particularly with regard to the airway management approach (orotracheal tube or laryngeal mask) and whether neuromuscular relaxants are used.
Conventional ultrasound allows for visualization of the airway from the most superior region to the pleura. Special techniques enable a more specific functional airway evaluation and may be applicable to anesthesia. Ultrasound delivers multiple advantages inter alia: it is safe, fast, reproducible, portable and renders of real time images.9,10
Due to the superficial localization of the larynx, the ultrasound lineal transducer provides for an adequate definition of the structures and precise identification. The component parts of the laryngeal skeleton elicit different ultrasound images.11 The trachea for instance is characterized by alternating hypo- and hyper-echoic bands representing the cartilaginous rings and the annular ligaments, respectively. The thyroid cartilage and the cricoid in adults exhibit progressive calcification and hence slight changes in the ultrasound images, particularly in males, which make the vocal-fold visualization in men even more difficult. The epiglottis on the other hand remains constantly hypoechoic. Thus, at 60 years of age, everyone shows signs of partial calcification; 40% of the cartilages at the level of the vocal folds are calcified and show a strong echo with posterior acoustic shadow; the thyroid cartilage provides the best window to observe the vocal folds in the form of an isosceles triangle with a central tracheal shadow; the vocal folds are medially aligned by the vocal ligaments that are hyperechoic.12
The vocal folds may be seen as lineal hyperechoic images that move during phonation. The thyrohyoid membrane that runs from the posterior margin of the hyoid bone to the cephalic margin of the thyroid provides an acoustic membrane through which the epiglottis may be visualized. However this is usually done with the lineal transducer placed parallel to the trachea with a slight cephalic angulation. Under the parasagittal view, the epiglottis looks like a curved hypoechoic structure and in the transverse view it looks like an inverted “C” anteriorly next to a triangular hyperechoic space, pre-epiglottic space and posteriorly against the mucous-air interphase.13
The vocal folds may easily be seen through the thyroid cartilage in people with no thyroid cartilage calcifications14; on the other hand, when calcifications are present, the vocal folds and the arytenoid cartilages may still be visualized, but some times the transducer has to be angulated at approximately 30° in the cephalic direction from the cricothyroid membrane. Singh et al., in a trial with 24 volunteers with an average age of 30 years, found that the best window to visualize the vocal folds is through the thyroid cartilage, moving the transducer slightly into a cephalic angle in the cephalocaudal direction.15 The true vocal folds are seen as hypoechoic images surrounded by lineal hyperechoic images corresponding to the vocal ligament that moves medially during phonation. Hu and cols in a trial with 229 patients, 2 to 81 years old, found that the vocal folds were visible in 100% of female participants; the visualization was 100% in males under 18 years of age and gradually dropped up to 40% in the 60-year-old patients.16
These results are consistent with that of a trial by Wang et al.,17 between august 2008 and march 2010, including 705 patients of whom 33 had some type of vocal fold paralysis. The purpose of the trial was to evaluate the use of ultrasound for vocal fold mobility. The average age of the participants in the trial was 48 years. The vocal fold movement seen under ultrasound was 87% in total, with 98% discrimination for females and 51% for males. Based on previous studies reported in the literature, ultrasound has the ability to document vocal fold mobility dysfunction in the pediatric population, as well as phonation disorders.18 The article concludes that ultrasound is an option for the assessment of vocal fold mobility in over 90% of the female population and approximately 50% of males. Flexible nasolanryngoscopy has been considered the method of choice to establish the paralysis of the vocal folds in the pediatric population; however, it does pose some limitations, particularly in children under 10 yeas of age because they tend to be uncooperative. Although CT scan and MRI are extremely useful, these methods do not allow for real time evaluation of the vocal fold movements, in addition to the risk of radiation and contrast media exposure. Wang et al.,19 in a trial with pediatric patients, analyzed the maximum angle of the glottis (determined by a line between the anterior commissure and the medial margin of the arytenoid with the vocal folds in total abduction) and the maximum arytenoid angle (formed by the medial and anterior margin of the commissure and the medial and lateral margin of the vocal folds) as a quantitative measure to evaluate the extent of vocal fold paralysis. They found that most patients presented with a maximum angle of the glottis of 61.4±9°, while patients with paralysis exhibited flaccidity and immobility during phonation and their maximum angle of the glottis dropped to 42.25°. Likewise, the maximum angle of the glottis decreased, as did the maximum angle of the arytenoid, so the authors suggest these ultrasound measurements as valuable parameters in the evaluation of the vocal fold paralysis.
It is then clear that ultrasound has multiple clinical applications, particularly in terms of real time images that can be used dynamically to enhance the evaluation and to develop airway management protocols, not only for the OR, but also for the ER and the ICU.20
The purpose of this case report is to underline the use of ultrasound in surgeries involving the thyroid gland and potentially the recurrent laryngeal nerve. The literature supports the use of ultrasound for the evaluation of the vocal folds and through phonation it is possible to assess the integrity of the recurrent laryngeal nerve, before and after surgery. This examination is easy, reproducible and on real time and can be done at the patient's bedside.
This article discusses 2 patients undergoing thyroidectomy for various surgical reasons and in both cases a previous evaluation was done to verify the bilateral and posterior integrity of the vocal folds bilateral mobility, using ultrasound with a lineal transducer, and evaluate the integrity of the recurrent laryngeal nerve.
The use of ultrasound is thus considered an option for the evaluation of the integrity of the recurrent laryngeal nerve following thyroidectomy.
FundingNone.
Conflicts of interestNone.
Please cite this article as: Linares JPA. Utilidad del ultrasonido en la valoración de cuerdas vocales posterior a tiroidectomia. Rev Colomb Anestesiol. 2014;42:238–242.