Systemic toxicity due to local anesthetics is one of the most feared complications in regional anesthesia due to the risk for the heart, the central nervous system and, in particular, the risk of triggering cardiorespiratory arrest, which is difficult to manage, even in healthy patients. Prevention as the main goal, together with prompt recognition and early treatment using several general measures followed by specific treatment with 20% lipid emulsions, improve prognosis dramatically for these patients. Their immediate availability in the operating theater or in areas where regional anesthesia is provided such as the emergency services and rooms where blocks are performed, may make the difference between a favorable or adverse prognosis in situations of severe systemic toxicity from local anesthetics.
The objective of this article is to create awareness on the prevention of toxicity events due to local anesthetics and provide knowledge about the management protocols in case such events should happen, recognizing the importance of having a toxicity kit available during daily practice and of following basic management guidelines adapted to the needs of each institution because, although this is a rare occurrence, it may be devastating.
La intoxicación sistémica por anestésicos locales es una de las complicaciones más temidas en la anestesia regional por su potencial tóxico cardiaco, neurológico y principalmente por el riesgo de desencadenar paro cardiorrespiratorio de difícil manejo, aún en pacientes sanos. La prevención como la primera meta, seguida de un rápido reconocimiento y tratamiento oportuno basado en diversas medidas generales y luego del tratamiento específico con las emulsiones lipídicas al 20% permiten mejorar drásticamente el pronóstico de estos pacientes. Su disponibilidad inmediata en las salas de cirugía o en las áreas destinadas para la realización de la anestesia regional como sala de bloqueos, servicios de urgencias, entre otros, puede significar la diferencia entre un pronóstico favorable o adverso en situaciones de toxicidad sistémica grave por anestésicos locales.
El objetivo de este artículo es sensibilizar al lector para prevenir los eventos de toxicidad por anestésicos locales y en caso de presentarse, conocer el protocolo de manejo y reconocer la importancia de disponer en su práctica diaria de un kit de toxicidad por anestésicos locales, siguiendo unos lineamientos básicos de manejo pero adaptados a las necesidades de cada institución, pues si bien esta complicación es rara, es potencialmente devastadora.
Local anesthetic systemic toxicity (LAST) is a rare but potentially fatal complication that may arise due to elevated plasma concentrations from high doses or inadvertent intravenous administration.1–3 Barrington et al. report an incidence of 0.98 for every 1000 blocks4,5 and it is one of the most frequent causes of anesthetic-related cardiorespiratory arrest.2
MethodNarrative review of local anesthetic systemic toxicity based on a search in PubMed and LILACS with no restrictions for language, or date of publication, using MeSH terms “local anesthetics”, “toxicity” and “lipids”.
Clinical presentationNeurologic toxicityNeurologic toxicity is reported in 89% of cases, without signs of cardiotoxicity in 45% of cases.6 The most common signs are seizures, agitation and loss of consciousness.1,6 Prodromic symptoms such as dysarthria, perioral numbness, metallic taste, tinnitus, dysphoria, confusion and dizziness occur only in 18% of patients.6
Cardiac toxicityIt is found in 55% of cases in the form of bradyarrythmias, hypotension, tachyarrythmias, conduction defects, wide QRS interval, ST changes with dyspnea and hypertension, and may progress to ventricular tachycardia with absent pulse, ventricular fibrillation or asystole.1,6
Atypical toxicity presentationsThere are atypical LAST presentations, such as the onset of symptoms 5min after the local anesthetic injection, associated with deep sedation or general anesthesia.1,6 The other form of atypical presentation is the presence of cardiotoxicity in the absence of neurotoxicity.6 It is important to recognize the clinical manifestations and understand the management of this complication because it is potentially fatal.7–9
Early prevention and detectionThe risk of severe systemic toxicity associated with local anesthetics increases in the case of peripheral nerve blocks, considering that several approaches to nerve structures are in close vicinity of the blood vessels and sometimes it takes more than one injection to achieve adequate regional anesthetic block.10–12 Prevention, as the first step, is the basis for lowering the risk of local anesthetic toxicity.13 The standard practice for the prevention of local anesthetic systemic toxicity includes the following14–16:
- -
-Limit the total dose of local anesthetic: Restrict the dose of local anesthetic using the smallest volume and the lowest concentration needed to achieve the block, in accordance with the maximum doses recommended for each of the local anesthetics,17 bearing in mind individual variability that may result in toxicity at levels below the recommended doses. It is important to be more cautious with higher risk patients, because in patients with altered conduction, low cardiac output or ischemia, metabolic diseases, liver diseases, or patients with low plasma protein concentrations, there is an increase in the free fraction of local anesthetics and also potential lower toxicity thresholds.13
- -
Incremental injection: It is advisable to inject slowly in fractionated doses of the local anesthetic, suctioning periodically to check for blood return every 3–5mL and waiting 30–45s before resuming the injection throughout the administration of the local anesthetic.14 It is worth remembering that intermittent aspiration may have a false negative rate of 0.6%–2.3%.18
- -
Use less toxic anesthetics: Short-acting local anesthetics (lidocaine) have a lower toxicity profile than long-acting agents (bupivacaine or l-bupivacaine),19 whose potency and effect are greater than those of the short-acting anesthetics.20,21l-Enantiomeres have better safety profiles for the central nervous system and for the cardiovascular system when compared to racemic compounds (bupivacaine).21,22
- -
The use of l-enantiomeres does not eliminate the need for following other safety recommendations.3,21
- -
Intravascular injection markers: The most important etiologic factor for the development of a systemic toxicity condition continues to be inadvertent intravascular injection of the local anesthetic.16 The use of epinephrine (2.5–5mcg/mL) is very important as a marker of intravascular injection.20,23 An unexplained increase in heart rate (10 beats per minute) and/or blood pressure (15mmHg), as well as changes in the status of the patient (confusion, restlessness, dizziness, seizures, etc.) may reflect intravascular injection, even if aspiration is negative.1,10,11,13,23 When patients are sedated, reported symptoms may be absent.24 In elderly patients using b-blockers under general anesthesia the response to intravascular epinephrine injection may be limited.14,25 The use of ultrasound has been associated with a lower incidence of inadvertent intravascular injection4,26 and it could be associated with a lower risk of local anesthetic toxicity.27 When used, ultrasound must always identify tissue distension under the local anesthetic injection; if not, intravascular injection must be suspected, even if color Doppler rules out the presence of blood vessels in the area of the block.28,29
- -
Basic monitoring: Required before, during, and at least for 30min after the nerve block, with immediate availability of the cardiovascular resuscitation equipment.15,30–32
- -
Atypical presentations of LAST must be known in order to be able to diagnose them and provide timely treatment18; it must also be remembered that symptoms may recur.18
In the event intravascular injection is detected, the injection must be interrupted, help must be requested,33 and the surgical procedure must be canceled. Adequate oxygenation is paramount, midazolam must be used for seizure suppression or, if seizures persist, succinylcholine must be considered in order to avoid acidosis from muscle activity.15,33 Cardiac depressant drugs must be avoided.15,33 In the event of cardiorespiratory arrest, Basic and Advanced Live Support guidelines must be followed, with the following modifications: use epinephrine in a dose of less than 1mcg/kg, avoid the use of vasopressin as well as the use of lidocaine as anti-arrhythmic15,33; also, it is important to remember that it may be a long resuscitation process lasting perhaps more than 1h.34 An assistant should make sure to read the checklist for the management of LAST35; transfer the patient to the Intensive Care Unit (ICU) or the Special Care Unit (SCU) for at least 12–24h because symptoms may recur. During the first two days, measure amylase and lipase to rule out the onset of pancreatitis.34
Report the event and lipid use at www.lipidrescue.org and www.lipidregistry.org.15,33
LipidsThe mainstay of treatment for LAST are the basic measures already described, which may solve most of the mild-to-moderate cases, and even some serious ones. The only specific successful treatment for LAST is 20% lipid emulsion,1 based on case reports and animal studies.36–41 The most generally accepted theory on the mechanism of action of lipid emulsion therapy is that of the “lipid sink”, which suggests that the lipid infusion creates a lipid compartment in plasma that remains separated from the aqueous phase.42 Lipophilic local anesthetics are collected in this lipid sink, reducing their aqueous phase concentration in plasma.42,43
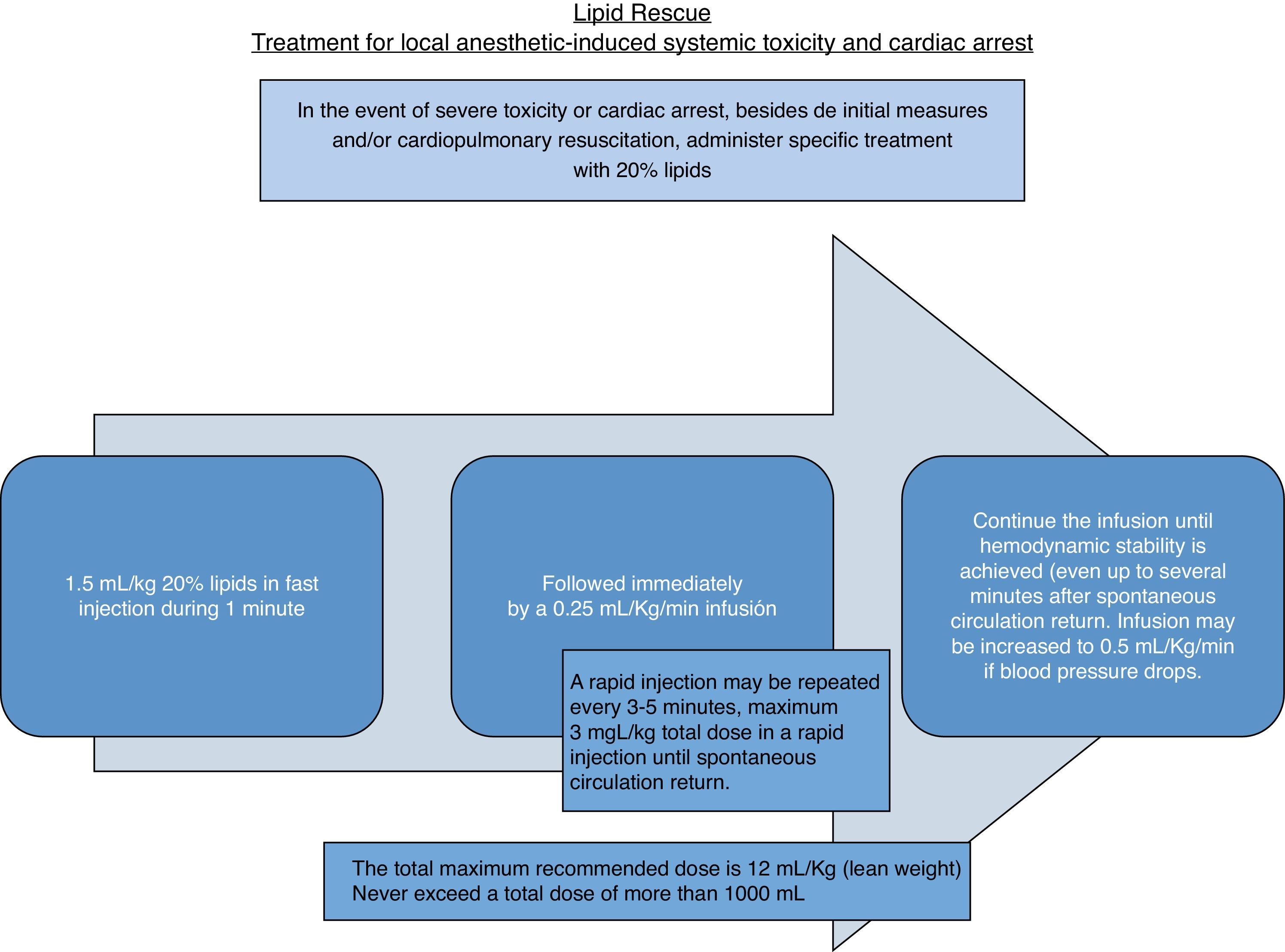
A 1.5mL/kg IV bolus in one minute is followed by 0.25mL/kg/min IV, with a repeat bolus after 3–5min if there is no spontaneous circulation return, followed afterwards by 0.5mL/kg/min,18 for a maximum of 10–12mL/kg33 as shown in Fig. 1.
It is important to recognize that lipids are not only used in cases of cardiorespiratory arrest, but also early on in cases of severe cardiac and/or neurological toxicity. The use of propofol is not recommended as a substitute for lipids in LAST18 because its lipid matrix is only 10% and it is a cardiac depressant.19
Adverse effects associated with lipid therapy, although not reported in patients receiving treatment for LAST, may occur in the form of hypersensitivity responses in patients who are allergic to soy protein or to eggs.36 Likewise, in patients with altered lipid metabolism (like hepatic, pancreatic or renal disorder), there may be an exacerbation of their underling condition.36
Considering that lipid therapy is of short duration, risks are lower than those that may emerge during prolonged parenteral nutrition,44 like increased risk of infection,45 thrombophlebitis46 or fat embolism.47
There are no randomized, placebo-controlled double-blind trials on the use of lipids in humans for obvious ethical reasons.44 Consequently, data are derived from animal studies and limited case reports in humans, but they suggest that lipid emulsion may be useful for cardiotoxicity or potentially lethal cardiac arrest attributable to other drugs such as antidepressants, verapamil, beta-blockers, bupropion, quetiapine, among others.48,49
Although most papers describe lipid rescue with a specific trademark (Intrapilid) different lipid brands and preparations have been used successfully for LAST rescue,50 which means that the exact formulation of the emulsion might not be important.36
RecommendationsAt the Pablo Tobón Uribe Hospital we have two kits, each with its protocol sheet listing the lipid dose and describing the management of patients with LAST. Information about the protocol and the kits in our unit was shared with the anesthetists through mass distribution of pocket guides, as well as e-mailings of all the information and references listed in them. Additionally, the protocol was presented during academic meetings in order to create awareness. An operating room nurse was charged with the job of showing the kits and their location to all the paramedical and other staff in the surgery area, and how to deliver them immediately when requested by the anesthetist. Two kits are available at all times, considering that, although the intoxication is a rare occurrence, it may have potentially lethal effects. One of the kits is located in the area where regional blocks are performed, and the second one is in the surgery storeroom, strategically located in the event it is required in an operating room. Kits are checked on a weekly basis by the non-paramedical staff in the surgery area and verified by the nursing staff.
It is important to have this protocol handy considering that this is a critical event in anesthesia that, although rare, requires optimal management in order to avoid fatal outcomes. It is even recommended that this management protocol must be made known to the ICU and SCU staff in charge of continuing to provide care to the patient.
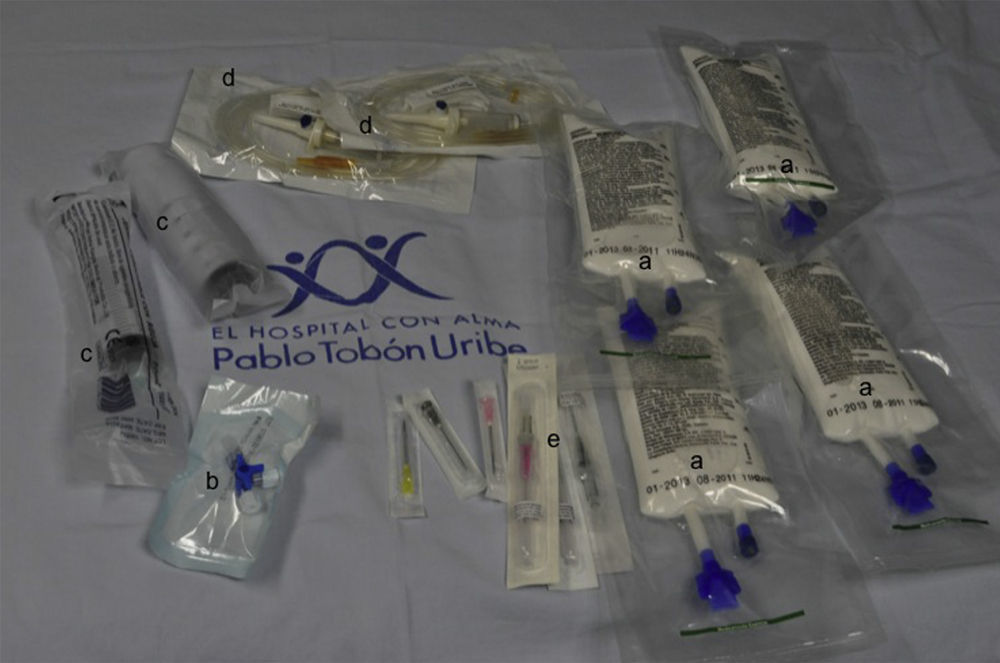
The kit (Fig. 2) consists of four bags of the 20% lipid emulsion (250mL) based on the suggestion by Marwick et al.51 of having a total dose of 1000mL available, in the event of potential recurrence of cardiovascular instability after having reversed the initial condition. The kit also includes a 3-way lock, two 50mL luer-lock syringes, intravenous access and venoclysis equipment, and the protocol sheet. The kit costs approximately COP 400000. We use a lipid emulsion containing 80% refined olive oil and 20% refined soybean oil for every 100mL (Fig. 3). This emulsion must be protected from the light and must be stored at a temperature below 30°C, without refrigeration, and must not be shaken before use.
Local anesthetic toxicity kit used at the Pablo Tobón Uribe Hospital. Contents detail: (a) 20% lipid emulsion (four 250mL bags); (b) 3-way lock; (c) 50mL luer-lock syringes for rapid infusion of the lipid emulsion; (d) infusion venoclysis equipment; (e) venous access devices of different diameters.
The increasing use of peripheral nerve blocks may result in more frequent cases of LAST than previously mentioned, because the risk has not been shown to diminish even despite the use of ultrasound. This and the potential fatal consequences of this occurrence means that we must become familiar with the management of this complication and have kits immediately available in those areas where regional anesthesia is used, including obstetric services, in order to provide timely treatment.
FundingAuthors’ own resources.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Berrío Valencia MI, Vargas Silva JF. Protocolo y necesidad de kit para toxicidad sistémica por anestésicos locales. Rev Colomb Anestesiol. 2013;41:274–279.