Patients who have experienced trauma usually develop hypovolemic shock, which determines different levels of tissue hypoperfusion. The determination of lactate levels has been used as a reliable biomarker in the assessment of the magnitude of hypoperfusion. Additionally, it has been established that lactic clearance in the first 6h has value as a prognostic measurement for the mortality rate of these patients. However, beyond 6h its utility is controversial.
ObjectiveTo evaluate the predictive capacity of serial lactic acid as well as clearance (at the time admitted, 12 and 24h) in mortality cases for trauma patients admitted to the ICU.
Materials and methodsDuring the period between 2010 and 2014, an observational longitudinal cohort study was conducted with trauma patients admitted to the Intensive Care Unit (ICU) at the Clínica Universidad de la Sabana. The clinical and demographic data was registered in a data base using Microsoft Excel and analyzed in STATA 12® statistical software.
In order to determine the association between each measurement with mortality after seven days, serial measurements of lactic acid were taken at admission time, 12–24h as well as the clearance of lactic acid at 12 and 24h.
Results233 patients participated during the time of the study. The average age was 38 years. 78% of the patients were male, with 21% of the mortality at seven days in the ICU. Among the severity indexes, an average of 14 in APACHE II, 9 in SOFA and 25 in ISS was found. The average of length of stay for survive patients was nine days in contrast to five days of mortality patients.
In brief, the lactic acid average was associated with mortality at seven days in the three time measurements.
On the other hand, the values of the receptor curve operating showed the best performance of the discrimination at 24h with a 2.35 cut-off point and OR 1.65 (CI 95% 1.27–2.13).
ConclusionsOur findings determined a similar performance of the lactic acid as compared to other studies, especially in the lactic acid level at 24h with relevant discrimination over 2.35mEq/L at 24. Nonetheless, reverse causality can eventually occur.
Los pacientes con trauma habitualmente cursan con choque hipovolémico que determina diferentes grados de hipoperfusión tisular. La determinación de los niveles de lactato ha sido utilizada como un biomarcador fiable en la evaluación de la magnitud de la hipoperfusión. Adicionalmente se ha establecido que el aclaramiento del lactato en las primeras seis horas, constituye una medida pronóstica de mortalidad de estos pacientes, sin embargo más allá de estas seis horas su utilidad es controvertida.
Objetivoevaluar la capacidad de predicción del lactato seriado y su aclaramiento (al ingreso, 12 y 24 horas) en la presentación de la mortalidad de los pacientes con trauma, que ingresaron a la unidad de cuidado intensivo.
Materiales y métodoSe realizó un estudio observacional de cohorte longitudinal, en pacientes ingresados a la unidad de cuidados intensivos de la Clínica Universidad de la Sabana, con diagnóstico de trauma, durante el periodo comprendido entre 2010 y 2014, de manera concurrente fue registrada en una base de datos creada en Microsoft Excel y analizada en el paquete estadístico STATA 12 (Data analysis and statistical software).
Mediciones seriadas de ácido láctico fueron realizadas al ingreso, 12 y 24 horas. Con el fin de determinar la asociación de cada una de las mediciones, así como el aclaramiento del ácido láctico a las 12 y 24 horas con la mortalidad a los siete días.
Resultados233 pacientes fueron incluidos durante el periodo de estudio, la edad promedio fue de 38 años, 78% fueron hombres con una mortalidad del 21%. Dentro de los índices de severidad, se encontró promedio de APACHE II de 14, SOFA de 9 y ISS de 25. La estancia hospitalaria para los no sobrevivientes fue de 4,7 días mientras que para los sobrevivientes fue de 9 días. Los valores promedios de las tres mediciones de lactato se asociaron a la mortalidad a los 7 días, teniendo mayor capacidad de discriminación el valor de lactato a las 24 horas con un punto de corte de 2,35 y un OR de 1,65 (IC 95% 1,27 – 2,13).
ConclusionesEl estudio permite determinar un comportamiento del lactato similar al encontrado en otras publicaciones, con evidencia de mayor capacidad de discriminación cuando este permanece elevado por encima de 2,35 a las 24 horas, pudiéndose explicar por la presencia de causalidad reversa.
Trauma is the third leading cause of death worldwide, notably affecting the population under 40 years of age. Of all causes, traffic accidents are responsible for the largest number of patients. Around the world every day, about 3000 people die from injuries resulting from traffic accidents. These especially affect the 15–29 year-old age group, according with WHO reports.1,2 In Colombia, trauma is a public health problem, where traumatic injuries due to violence and traffic accidents are among the top causes of morbidity and mortality.3,4 Therefore, there is a need for a biomarker that allows us to quickly and reliably assess the diagnostic process of hypoperfusion during its early stage, in order to take the pertinent steps to reduce these mortality figures.5–7 This why lactate represents an important tool within this scenario, being a widely studied biomarker.8,9
Several publications show the relationship between lactate intake, early clearance and mortality. However, beyond these 6h, its usefulness is controversial.8,10–19 In the present article, we tried to establish the predictive capacity of serial lactate and its clearance (at admission time, 12 and 24h) when mortality occurred in patients with trauma who entered the intensive care unit.
Materials and methodsAn observational longitudinal cohort study was conducted in patients admitted to the Intensive Care Unit (ICU) of the Universidad de la Sabana Clinic (located in Chía, Cundinamarca, Colombia) between January 1st, 2010 and January 1st, 2014. The clinic is located in a busy traffic area where an large number of patients suffer traffic accidents. After the approval by the institutional ethics committee, the information of all patients diagnosed with trauma who survived at least 24h was recorded concurrently. Socio-demographic, clinical and paraclinical variables, as well as APACHE II, SOFA and ISS severity indexes were taken into account.20–24 Also, measurements of serum lactate upon admission to the ICU, at 12 and 24h were considered. All patients with incomplete measurements or data and those referred from other institutions were excluded.
Statistical analysisFor the elaboration of the database we used Microsoft Excel 2011, version 14.0 and for the processing of data we used the statistical package STATA 12.0. Descriptive statistics were performed and the association between the averages for each of the three lactate measurements with early mortality at seven days was determined. The clearance of lactate levels was evaluated, considering the percentage of lactate cleared with respect to the previous measurement, with the following equation: %Clearance=((basallactate−lactatecontrol)/basallactate)×100.13,25
In addition, discrimination capacity was determined by calculating the area under the ROC curve and the highest discrimination cut-off point by the Liu method, which maximizes the product of the sensitivity and specificity from which the lactate measurements were dichotomized. OR estimates were obtained in relation to mortality. All calculations were performed with a significance level of <0.05.
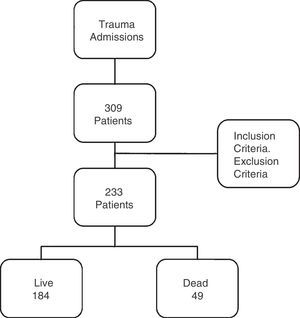
ResultsA total of 309 polytraumatized patients were admitted to the ICU during the study period. 233 patients met the inclusion criteria for information recording as shown in flow chart 1 (Fig. 1).
Of the total number of patients with polytraumatism, 184 patients (78%) were male. Early mortality, described as less than 7 days, was 21%, being higher in the male group compared to the female group (58% vs 42%, respectively).
All measurements of lactate inflow to the unit were performed within the first 28h SD (10) of admission to the hospital. The time of admission to the UCI was considered as hour “zero”. The second measurement was performed at 12h with an average of 10.2h and a SD of 11.8h. The third measurement was performed at 24h with an average of 24.4h and a SD of 13h. The analysis of variance for the three measurements showed differences between the three groups of measurements with a p-value<0.001.
The variables that were associated with early mortality were APACHE II, SOFA and ISS, as well as the lactate levels in each of the measurements. See Table 1.
General characteristics and biomarkers in trauma patients.
| Live N=184 | Dead N=49 | p-value | |
|---|---|---|---|
| Male gender n (%) | 155 (84) | 28 (57) | 0.001 |
| Age, mean (SD) | 35.61 (13.36) | 44 (19.40) | 0.001 |
| IQR | 24–44 | 30–52 | |
| APACHE II, mean (SD) | 13.20 | 21.40 | 0.001 |
| IQR | 8–17 | 16.5–27 | |
| Lactate at admission, mean (SD) | 2.81 (1.55) | 4.92 (3.97) | 0.001 |
| IQR | 1.85–3.45 | 2.4–5.8 | |
| Lactate at 12h, mean (SD) | 2.35 (1.58) | 4.14 (3.51) | 0.001 |
| IQR | 1.2–3 | 1.4–5.7 | |
| Lactate at 24h, mean (SD) | 1.9 (1.14) | 3.67 (2.79) | 0.001 |
| IQR | 1.3–2.2 | 1.6–5 | |
| Stay in UCI, mean (SD) | 9.33 (8.22) | 5.05 (7.39) | 0.001 |
| IQR | 3.66–13 | 1–5 | |
| SOFA, mean (SD) | 8.73 (3.04) | 10.5 (2.41) | 0.001 |
| IQR | 7–11 | 9.5–12 | |
| ISS, mean (SD) | 21.07 (14.87) | 39.2 (25.95) | 0.001 |
| IQR | 12–24 | 18–75 | |
| % Lactate-clearance admission – 12h | |||
| Mean (SD) | 5.64 (62.7) | −2.68 (61.9) | 0.48 |
| % Lactate-clearance admission – 24h | |||
| Mean (SD) | 20.7 (51.9) | −3.23 (65.8) | 0.04 |
| % Clearance – 12h–24h | |||
| Mean (SD) | 9.5 (39.7) | −44.5 (138) | 0.001 |
Mortality measured at 7 days.
SD: standard deviation, IQR: interquartile range; SOFA: Sequential Organ Failure Assessment; ISS: Injury Severity Score; APACHE II: Acute Physiology and Chronic Health Evaluation.
Source: Authors.
The average stay for living patients was 9 days whereas for those who did not survive it was 4.7 days.
Trend of lactate levelsAs shown in Table 1, the value of lactate levels decreased as time progressed from admission to 12h and 24h, with averages and standard deviations of: 3.28 (2.46) (CI 95% (2.92–3.64)); 2.73 (2.24) (CI 95% (2.39–3.67)); 2.21(1.68) (CI 95% (1.93–2.49)), respectively. When the lactate averages between live and dead patients are compared, statistically significant differences in the mean values at admission, 12 and 24h of −2.11–1.79 and −1.77 were found.
Regarding the lactate clearance, an association in the differences between the admission time and the 24h and between 12 and 24h was found, but not between admission and the first 12h.
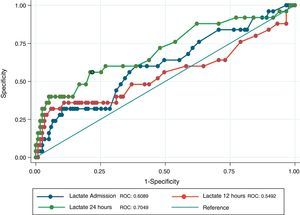
Discrimination capacity of lactate for early mortality in each of the three time periodsIn Table 2, the values of the area under the ROC curve of the three moments of lactate measurement are recorded. A trend of greater discrimination was observed as time progresses. Additionally, cut-off point, sensitivity and specificity values were recorded for each of the moments in relation to early mortality (seven days).
Discrimination capacity of lactate during the first 48h for the prediction of mortality at seven days in trauma patients.
| Measurement | ROC curve area (CI 95%) | Cut-off point (mEq/L) | Sensibility | Specificity |
|---|---|---|---|---|
| Lactate admission | 0.61 (0.48–0.73) | 3.05 | 0.66 | 0.67 |
| Lactate 12h | 0.55 (0.40–0.70) | 3.65 | 0.46 | 0.84 |
| Lactate 24h | 0.70 (0.58–0.83) | 2.35 | 0.56 | 0.79 |
Source: Authors.
As can be seen in Table 3, the ORs for early mortality for each one of the moments were calculated from the values of the cut-off points. We found an OR of 1.4 (CI 95% (1.17–1.68)) for the lactate at admission when a lactate level is greater than 3.04mEq/L; at 12h, an OR of 1.35 (CI 95% (1.14–1.60)) with a lactate greater than 3.65mEq/L; and at 24h, an OR of 1.65 with (95% CI (1.27–2.13)) with a cut-off point of 2.35mEq/L.
Fig. 2 shows the largest area under the curve for lactate levels at 24h after admission (0.70) denoting a greater discriminatory power for early mortality, whereas the values of the area under the curve at admission time and 12h are lower, 0.60 and 0.54 respectively.
DiscussionLactate levels in the blood reflect the balance between lactate production and lactate uptake in tissues, which is usually in the range of 0.5–1.8mM/L.26 Numerous studies have established the use of lactate as a diagnostic, therapeutic and prognostic marker for tissue hypoxia. The vast majority of these studies have used 2.0mM/L as a cut-off. This cut-off point has been established in different scenarios and different types of patients. That is how Kliegel et al. examine patients who were resuscitated from cardiac arrest and survived at least 48h,27 concluding that sustained hyperlactatemia (>2.0mM/L after 48h) is a predictor of mortality as well as of a poor neurological prognosis. Kruse et al. carried out a systematic review establishing that the cut-off point of >2mM/L is most frequently associated with mortality in critical patients with some type of trauma. More recently, cut-off points have been classified according to their severity, into the levels low (<2.5mg/dL), moderately elevated (2.5–3.9mg/dL) and severely elevated (>4mg/dL).26,28–30 One of the first studies that determined the association between lactate levels and mortality in trauma patients was performed by Abramson. He found that the delay in the normalization of lactate levels after 24 and 48h was associated with increased mortality, whereas patients who normalized lactate values before 24h had a 100% survival rate. In our study, this finding was not confirmed. Even patients with normal lactate during the first 12h died, this probably due to the greater severity of our patients with a mean ISS of 30 whereas the one reported in Abrasom study was 22.10
When it was explored which of the measures in the time (admission, 12 and 24h) would have the greater discrimination capacity for survival, it was observed that those patients with lactate above 2.35mEq/L at 24h presented the highest mortality rate. However, in 2012, Dr. Marie-Alix Régnier12 found that measurements of clearance within the first four h based on lactate levels at admission, had an adequate ability to discriminate between the patients who died or survived, with an area under the ROC curve (0.78, 95% CI: 0.73–0.83). We only found that lower and later clearance was associated with mortality at 24h, with an area under the ROC curve of 0.70 (0.58–0.83)
In 2013, Stephen R. Odom13 included 4742 trauma patients in his study, finding that initial lactate was the strongest predictor of mortality in the trauma patient when the first lactate was greater than 4mEq/L. They also performed the calculation of lactate clearance in this group of patients, with a time interval of 6h, finding that with lower clearance came higher mortality. Our study evaluated the clearance between admission, 12 and 24h, only finding an association with the decrease of clearance at 24h.
In 2015, Dr Dezman Zachary's work14 with 18,304 patients with trauma is published. Lactate clearance was evaluated at 24h in 3887 patients and only 7.8% of the population achieved a lactate clearance of below 2mEq/L. However, an adequate discriminatory capacity of lactate levels at 24h with an area under the curve of 0.8 was found. The severity of the population of this study was lower than ours with an average of 25 in the ISS.
Our study has the limitation of not having evaluated lactate clearance within the first 6h based on lactate levels at admission. Nevertheless, it does monitor lactate in the first 24h, showing a broader picture and demonstrating how the later worsening of lactate levels determines increased mortality.
ConclusionsOur study showed that lactate levels greater than 2.35mEq/L at 24h were associated with an increased risk of mortality. On the other hand, lower lactate clearance or even negative clearance led to increased mortality, especially at 24h. It could not be established that early clearance would improve prognosis. The findings of the present study could be influenced by reverse causality in that those patients with the worse prognosis would be precisely those in which the goals of resuscitation would not be achieved.
FundingThis project was supported by the Universidad de la Sabana with regard to methodological aspects.
Conflict of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Oliveros-Rodríguez H, Estupiñán-López R, Rodríguez-Gómez J. Mediciones seriadas del lactato y su validez predictiva de la mortalidad temprana en los pacientes con politrauma que ingresan a la unidad de cuidado intensivo. Rev Colomb Anestesiol. 2017;45:166–172.