Despite the widespread use of Propofol–opioid combinations for induction and maintenance of adequate anesthesia and analgesia, there are no studies comparing the use of manual Total Intravenous Anesthesia with Remifentanil–Propofol versus Fentanyl–Propofol.
ObjectiveTo compare emergence and discharge times between two Total Intravenous Techniques used at Occidente de Kennedy Hospital, one based on Propofol and Remifentanil (manual infusion) and the other based on Stangraf-controlled Propofol and Fentanyl.
MethodAnalytical observational study for the comparison of two groups of subjects, one exposed to Remifentanil plus Propofol and the other exposed to Fentanyl plus Propofol, comprising 43 patients taken to surgery under Total Intravenous Anesthesia at Occidente de Kennedy Hospital. Data were analyzed using the Shapiro–Wilks, Student t and Mann–Whitney U tests and the Spearman and Pearson correlation coefficients, using Windows SPSS, version 20. A p value <0.05 was accepted as statistically significant.
ResultsIn comparing the two techniques, no statistically significant time differences were found. The mean emergence time was 10.1min for Fentanyl and 10.2min for Remifentanil. The discharge time for Fentanyl was 11.9min and 11.5min for Remifentanil.
ConclusionsThe Stangraf-guided use of Fentanyl–Propofol combination is equivalent to the use of Remifentanil–Propofol (manual infusion) in terms of emergence and discharge times. Additional studies are required in order to confirm these findings.
A pesar del amplio uso de combinaciones de propofol y opiáceos para inducir y mantener una adecuada anestesia y analgesia, no existen estudios que comparen el uso de anestesia total intravenosa manual con remifentanilo-propofol versus fentanilo-propofol, controlado por Stangraf.
ObjetivoComparar el tiempo de despertar y el tiempo de descarga entre 2 técnicas de anestesia total intravenosa manual empleadas en el Hospital Occidente de Kennedy, una basada en propofol y remifentanilo y otra basada en propofol y fentanilo controlado por Stangraf.
MetodologíaEstudio observacional analítico de comparación de 2 series de sujetos expuestos, unos a remifentanilo-propofol y otros a fentanilo-propofol, en 43 pacientes llevados a cirugía bajo anestesia total intravenosa en el Hospital Occidente de Kennedy. Se analizó la información mediante las pruebas de Shapiro-Wilks, t de Student y U de Mann Withney y los coeficientes de correlación de Spearman y de Pearson, usando SPSS versión 20 para Windows. Un valor de p<0,05 fue aceptado como estadísticamente significativo.
ResultadosAl comparar las 2 técnicas no se encontraron diferencias estadísticamente significativas en los tiempos evaluados. El tiempo de despertar promedio fue de 10,1min para fentanilo y de 10,2min para remifentanilo. El tiempo de descarga para fentanilo fue de 11,9min y para remifentanilo, de 11,5min.
ConclusionesEl uso de fentanilo-propofol guiado por Stangraf es equivalente al uso de remifentanilo-propofol en cuanto a los tiempos de despertar y de descarga. Se requierennuevos estudios para corroborar estos hallazgos.
Total Intravenous Anesthesia has advantages over inhaled anesthesia, such as absence of pollution, minimal cardiac depression, lower neurohumoral response, reduced oxygen consumption, lower incidence of postoperative nausea and vomiting,1 early recovery and prompt transfer to the recover room, with shorter discharge time.2 The discovery of Propofol revolutionized the use of Total Intravenous Anesthesia and is the most widely used agent for maintenance.3 However, Propofol does not have all the characteristics of an ideal agent, requiring supplementation with other drugs.1,4 Propofol–opioid combinations are used widely at the present time for induction and maintenance of adequate anesthesia and analgesia, reducing the dose of the induction agent, increasing hemodynamic stability, and suppressing the response to laryngoscopy and intubation.2 The knowledge of drug pharmacokinetics and pharmacodynamics will enable anesthesiologists to administer a combination that will provide the best anesthetic stability with short induction and recovery times, together with optimal surgical conditions and low incidence of adverse effects.4
Different studies have been conducted comparing intraoperative responses, recovery profiles, postoperative adverse effects and costs generated by the use of Remifentanil and Fentanyl.5 Compared with Fentanyl, as a supplement to general anesthesia, Remifentanil has shown to improve intraoperative hemodynamic control, emergence time and the incidence of respiratory depression during postanesthetic recovery. However, Remifentanil has not been shown to improve hospital discharge times, post-emergence adverse effect profiles or patient satisfaction, and it has been associated with a higher incidence of intraoperative hypotension and bradycardia. Moreover, its costs are higher. Another disadvantage is the rapid waning of the analgesic effects once it is discontinued. The adverse effect profiles of Remifentanil and Fentanyl are similar, with frequent occurrence of nausea, vomiting and pruritus. They can both produce chest wall stiffness, in particular when given as boluses.6
Anesthesiologists base their choice of drugs on their perception of effect duration.7 Traditionally, it has been accepted that anesthesia with Propofol–Remifentanil is associated with a faster awakening after any infusion time when compared with Fentanyl, Alfentanil or Sufentanil, due to their pharmacokinetic differences,6 and it is suggested that in order to avoid delay in awakening, responses must be counteracted with additional Propofol when it is combined with Fentanyl, Alfentanil or Sufentanil.4
Pharmacokinetic and pharmacodynamic models are based on sets of mathematical equations that relate the dose of the drug to its blood concentration and its time-related effect.2 These models may be incorporated into a computer software that shows the predicted drug concentration, plasma and effect site levels throughout time for a given dose, helping the anesthesiologist to set an adequate and stable level of anesthesia and predict the duration of action after short periods of administration, and optimize recovery after prolonged periods of administration.2,5
ObjectiveTo compare emergence and discharge times between two manual Total Intravenous Anesthesia techniques used in the anesthesia service of Occidente de Kennedy Hospital, one based on Propofol–Remifentanil and the other based on Propofol–Fentanyl.
Materials and methodsAnalytical observational study was done comparing two series of subjects exposed to Remifentanil–Propofol (manual infusion) in the first group and Fentanyl–Propofol (controlled by Stangraf) in the second group, between June 2011 and January 2012. The groups consisted of patients in whom the Total Intravenous Anesthesia protocol established by the anesthesia service of the Occidente de Kennedy Hospital was used (Annex 1).
The following were the inclusion criteria: ASA I and II patients of both sexes between 18 and 65 years of age, who received general anesthesia using Total Intravenous Anesthesia for elective low or intermediate risk surgeries. The exclusion criteria included body mass index greater than 30, altered state of consciousness, need for postoperative ventilation support, refusal to participate in the study, and contraindication for the use of any of the drugs in the study.
Data were collected before and during the surgical procedure and included subject demographics (age and gender), anthropometric measurements (weight and height), anesthetic technique (Propofol–Remifetanil or Propofol–Fentanil), ASA classification, type of surgical procedure and operative time. At the end of the surgical procedure, the investigator used a stopwatch to measure emergence and discharge times (time elapsed between the end of the procedure and the transfer to the Post-Anesthetic Care Unit) in accordance with the Recovery Scale for breathing and wakefulness of Schraag et al.,7 and recorded them in the tool designed for that purpose. Adverse reactions and other observations deemed relevant by the investigator were also recorded.
The Shapiro–Wilks test was used to assess the fit between the continuous quantitative variables and the normal probability distribution, and it was found that surgical times are quite asymmetrically distributed, making it impossible to use this distribution for data analysis. For comparison between the effects of the anesthesia procedure, the Student t test and the Mann–Whitney U test were used depending on the case. Spearman and Pearson correlation coefficients were used to assess the relationship between emergence/discharge times and other variables such as age, weight, and the length of surgery. Fisher's exact test was used to compare the proportion of occurrence of certain events of interest between the groups. All analyses were done using Windows SPSS, version 20, and a value of 0.05 was accepted as the limit for type 1 error in statistical decisions.
ResultsA total of 43 patients were included in the study: 27 males (62.8%) and 16 females (37.2%). The mean age was 38.9 years (range 18–65); mean weight was 63.9kg (range 39–90kg) and mean height was 1.64m (range 1.45–1.79m). Surgery time ranged between 35 and 275min with an average of 95.7min. Of all the patients, 23 (53.5%) were ASA I, 17 males and six females, and 20 patients (46.5%) were ASA II, ten of each sex. Forty patients (93%) had a normal nutritional status, 2 were (4.7%) overweight and 1 (2.3%) was low weight.
The surgical procedures were the following: 5 (11.6%) head and neck surgeries, 6 (14.0%) otolaryngological surgeries, 2 (4.7%) maxillofacial surgeries, 3 (7.0%) thoracic surgeries, 10 (23.3%) abdominal surgeries, 9 (20.3%) orthopedic surgeries, 3 (7,0%) peripheral vascular surgeries, and 5 (11.6%) plastic surgeries.
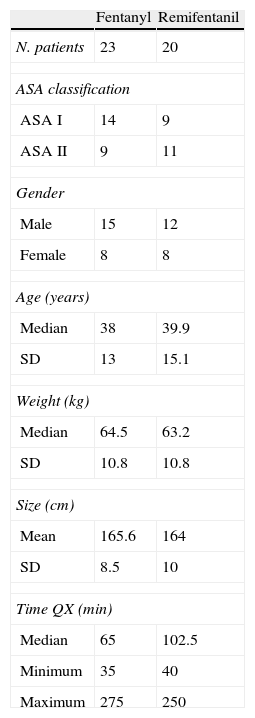
The Remifentanil group included 20 patients, 12 males (60%) and 8 females (40%) and the Fentanyl group included 23 patients, 15 males (65.2%) and 8 females (34.8%). The demographic and anthropometric characteristics of the two groups were homogeneous (Table 1).
Patient characteristics by treatment groups.
| Fentanyl | Remifentanil | |
| N. patients | 23 | 20 |
| ASA classification | ||
| ASA I | 14 | 9 |
| ASA II | 9 | 11 |
| Gender | ||
| Male | 15 | 12 |
| Female | 8 | 8 |
| Age (years) | ||
| Median | 38 | 39.9 |
| SD | 13 | 15.1 |
| Weight (kg) | ||
| Median | 64.5 | 63.2 |
| SD | 10.8 | 10.8 |
| Size (cm) | ||
| Mean | 165.6 | 164 |
| SD | 8.5 | 10 |
| Time QX (min) | ||
| Median | 65 | 102.5 |
| Minimum | 35 | 40 |
| Maximum | 275 | 250 |
SD: standard deviation.
Source: Authors.
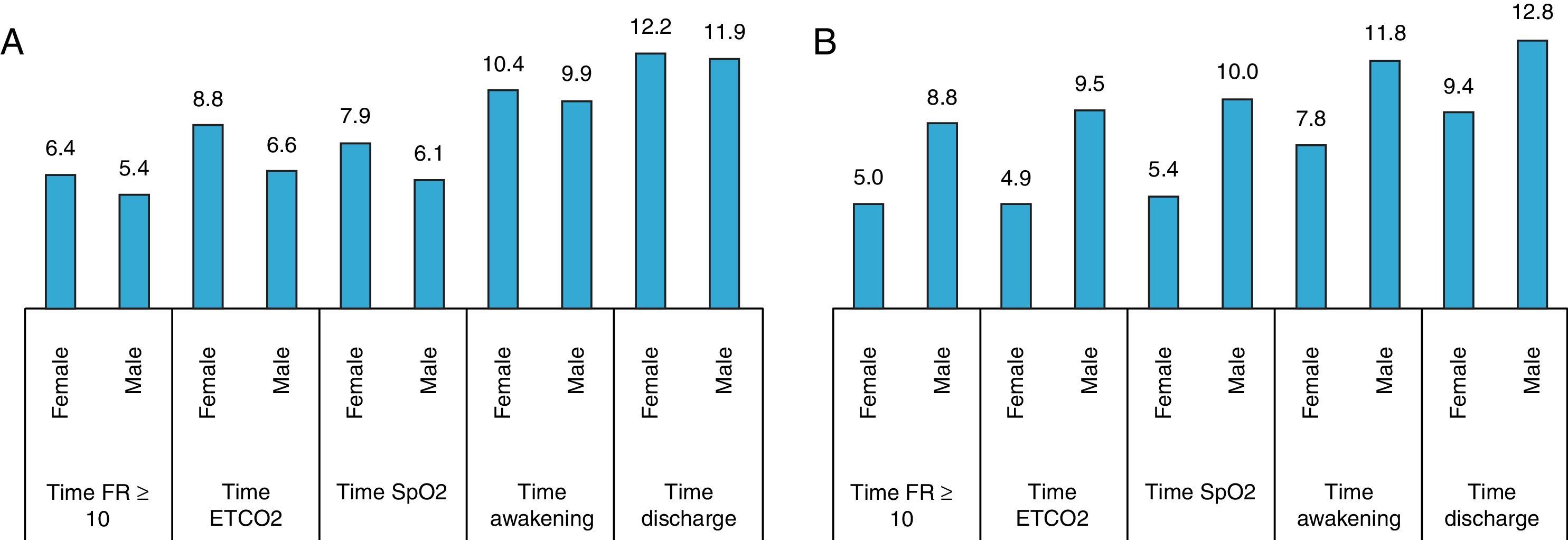
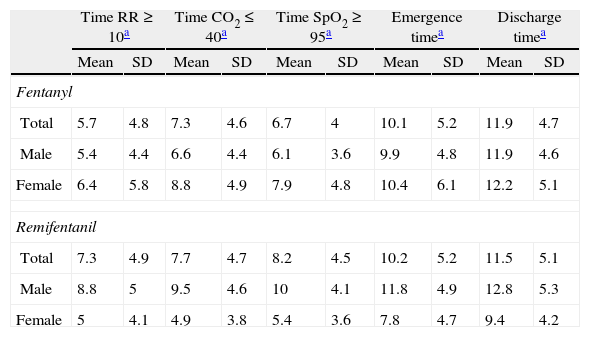
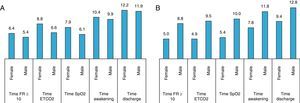
No statistically significant differences were found when comparing times between the two techniques: Remifentanil–Propofol and Fentanyl–Propofol. The mean time to achieve respiratory rate greater than or equal to 10 breaths per minute was 5.7min for Fentanyl, and 7.3min for Remifentanil. The mean time to achieve CO2 values less than or equal to 40mmHg was 7.3min for Fentanyl and 7.7min for Remifentanil. The time to achieve an SpO2 greater than or equal to 95% was 6.7min for Fentanyl and 8.2min for Remifentanil. Mean emergence time was 10.1min for Fentanyl and 10.2min for Remifentanil. Discharge time in the Fentanyl group was 11.9min and 11.5min for the Remifentanil group (Table 2).
Emergence and discharge times according to treatment groups.
| Time RR≥10a | Time CO2≤40a | Time SpO2≥95a | Emergence timea | Discharge timea | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Fentanyl | ||||||||||
| Total | 5.7 | 4.8 | 7.3 | 4.6 | 6.7 | 4 | 10.1 | 5.2 | 11.9 | 4.7 |
| Male | 5.4 | 4.4 | 6.6 | 4.4 | 6.1 | 3.6 | 9.9 | 4.8 | 11.9 | 4.6 |
| Female | 6.4 | 5.8 | 8.8 | 4.9 | 7.9 | 4.8 | 10.4 | 6.1 | 12.2 | 5.1 |
| Remifentanil | ||||||||||
| Total | 7.3 | 4.9 | 7.7 | 4.7 | 8.2 | 4.5 | 10.2 | 5.2 | 11.5 | 5.1 |
| Male | 8.8 | 5 | 9.5 | 4.6 | 10 | 4.1 | 11.8 | 4.9 | 12.8 | 5.3 |
| Female | 5 | 4.1 | 4.9 | 3.8 | 5.4 | 3.6 | 7.8 | 4.7 | 9.4 | 4.2 |
Source: Authors.
While emergence and discharge times were longer among women in the Fentanyl group, in the Remifentanil group this finding was observed among the men. However, no statistically significant differences were found in the two groups (Fig. 1).
No linear relationship was observed in the Propofol–Fentanyl group when analyzing the correlation between emergence/discharge times and surgical time; however, in the Propofol–Remifentanil group an inverse relationship was found both for emergence time (r=−0.342) as well as for discharge time (r=−0.308). Although it is not statistically significant, this relationship is an indication that, in this group of patients, those who had a longer surgery tended to wake faster and, consequently, were taken sooner to the Post-Anesthesia Care Unit. In analyzing the relationship on the basis of gender, in the Propofol–Remifentanil group there is a direct trend in men, whereas the trend is inverse in women, although the differences were not statistically significant.
Using the Spearman coefficient, a weak negative, non-statistically significant relationship was found between age and emergence time, and between age and discharge time in the Propofol–Fentanyl group. This means that, the older the age, the shorter the emergence and discharge times (r=−0.117 and r=−0.172). In the Propofol–Remifentanil group, correlation coefficients were quite close to zero, indicating absence of correlation between the two variables.
There was intraoperative hypotension in nine patients (20.9%), 1 (4,3%) with Fentanyl (female) and 8 (40%) with Remifentanil (5 males and 3 females); the difference in the incidence of hypotension between the two groups was statistically significant (p=0.0053).
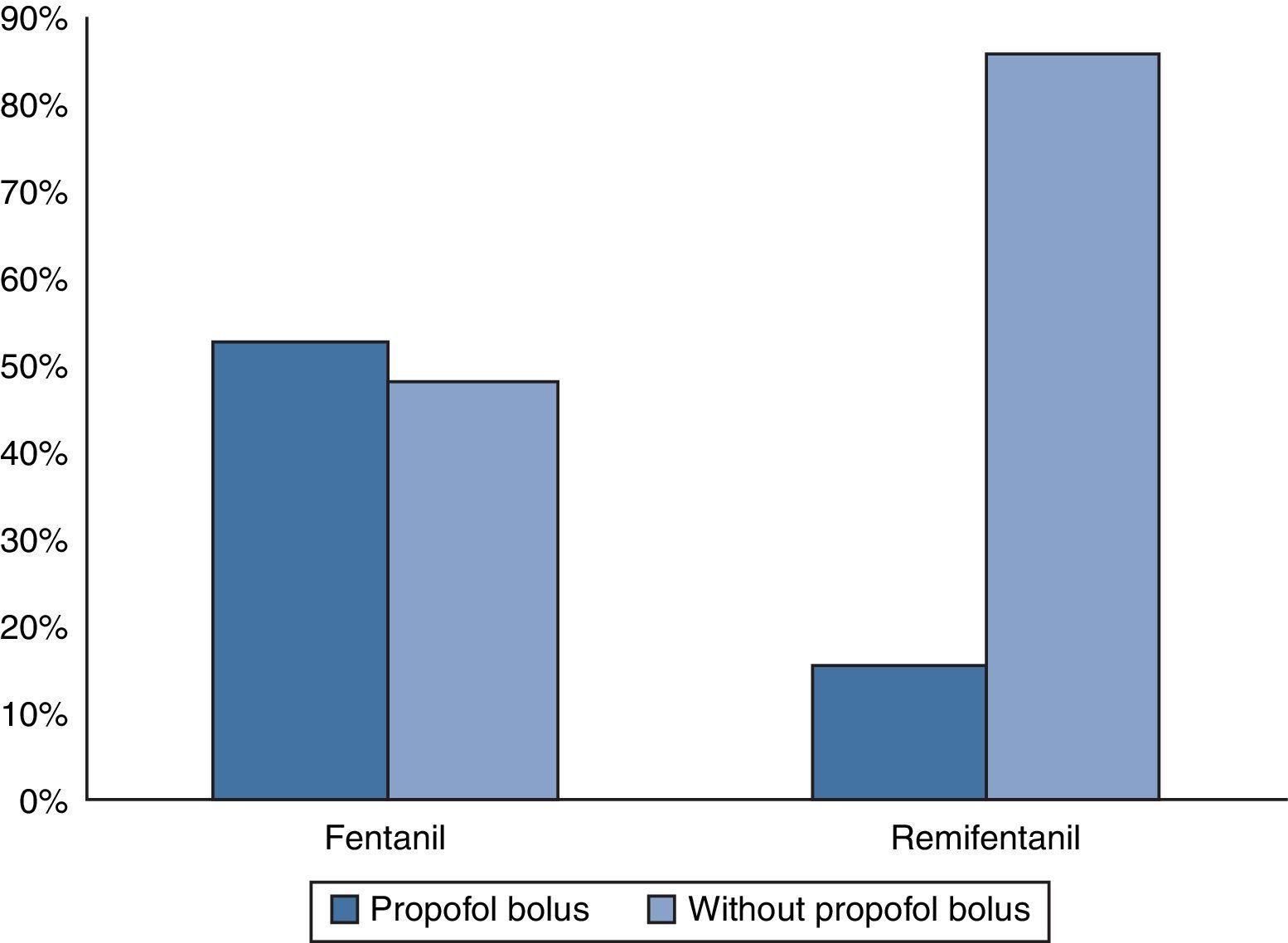
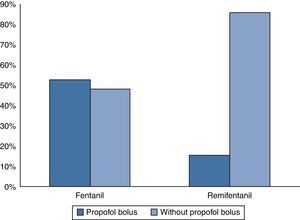
In the Fentanyl group, 12 patients (52.2%) required one or more additional boluses of Propofol, while in the Remifentanil group, 3 patients (15%) required them (Fig. 2). The difference in the requirement of additional doses between the two anesthetic techniques was statistically significant (p=0.0257).
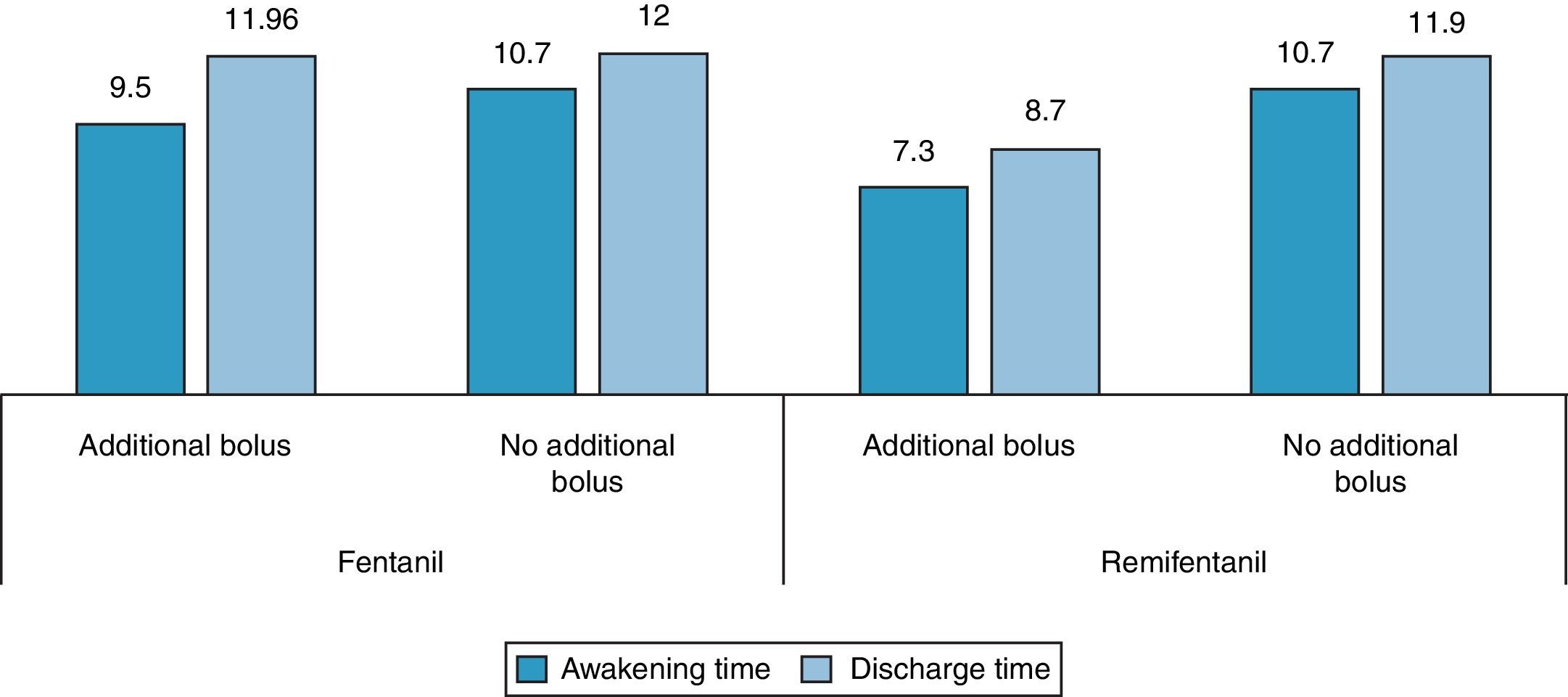
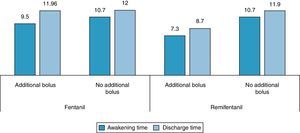
A non-statistically significant weak negative correlation was observed between the number of boluses and emergence and discharge times in the Propofol–Remifentanil group. In the Fentanyl group, the mean emergence and discharge times in the patients who did not receive additional boluses were 10.7min and 12min respectively, and the mean times in those who received boluses were 9.5min and 12.0min, respectively. In the Remifentanil group, mean emergence and discharge times in the patients who did not receive Propofol boluses were 10.7min and 11.9min, respectively, and 7.3min and 8.7min in those who received them (Fig. 3). In the Fentanyl group, the younger patients required additional boluses. The mean age of the subgroup requiring boluses was 35.9 years, and 40.3 years in the group that did not require additional boluses, with no statistically significant differences. No differences were observed in relation to age in the Remifentanil group. In the Fentanyl group, although the mean weight of the patients requiring additional Propofol boluses was lower (62.5kg) compared to the weight of the patients who did not require boluses (66.6kg), this difference was not statistically significant.
DiscussionPropofol and opioid combinations are widely used in modern anesthetic practice and it has been traditionally accepted that Propofol–Remifentanil anesthesia is associated with a faster recovery of consciousness after any infusion time when compared to Fentanyl, due to its pharmacokinetic characteristics. However, there are no studies in the literature comparing the use of Propofol–Remifentanil with the use of Stangraf-guided Propofol–Fentanyl. The use of a manual system based on a mathematical pharmacokinetic model allows concentration adjustments in accordance with patient conditions, and may be implemented with any available infusion system. Computer-based simulation systems have been used with this aim, including the Stangraf, Tivaman, Tivatrainner and Rugloop systems.2,8 Studies show that the use of a manual system supported by a pharmacokinetic model has advantages over the use of Target Controlled Infusion, such as the use of smaller quantities of Propofol, the ability to use any form of Propofol and any infusion pump, as well as the use of Total Intravenous Anesthesia with the same efficacy and safety of an automated system.8–10
Computer simulations may help anticipate the clinical behavior of anesthetic drugs. According to prior studies, the Stangraf software provides reliable pharmacokinetic estimates for optimal general anesthesia administration, and reliable estimates regarding recovery variables during the use of Propofol in combination with opioids, as demonstrated in a study that compared the use of Remifentanil infusion with the use of a Sufentanil infusion in combination with Propofol in patients taken to thyroid surgery.5 There are studies in the literature showing the benefits of using Remifentanil and Fentanyl in general anesthesia,11–14 but there are few studies using Fentanyl infusions, and there are no studies showing Stangraf-controlled use.
This study enabled us to show that emergence and discharge times with the use of Fentanyl are very similar to emergence and discharge times associated with Remifentanil, when the former is guided by a simulation software like the Stangraf. The two manual Total Intravenous Anesthesia techniques deliver safe general anesthesia with short emergence and discharge times.
Like other reports in the world literature, we found a higher incidence of hypotension with the use of Remifentanil compared with Fentanyl. No other adverse effects were found in either of the two groups assessed. The group that received Fentanyl–Propofol, required a significantly higher number of Propofol boluses because of signs of inadequate depth of anesthesia, compared with the group that received Remifentanil–Propofol. This may be explained by the fact that Fentanyl was maintained at a fixed dose throughout the study period, while Remifentanil could be modified according to the patient's requirements; moreover, there is synergy between Remifentanil and Propofol, resulting in lower Propofol requirements. This is an important fact, considering that one of the disadvantages of the Fentanyl-based technique is its lower cost compared to Remifentanil, and the use of additional Propofol boluses could increase costs substantially. The negative correlation between the number of Propofol boluses and emergence time is an interesting finding, meaning that patients requiring a higher dose have a shorter waking time. This may reflect pharmacodynamic differences between individuals. It was not possible to assess the impact of weight disorders, due to the small number of patients who were low weight or overweight. Although gender differences were not statistically significant, they could be important from the clinical standpoint. However, a larger sample is required for a more adequate assessment. The longer emergence time in women who received Propofol–Fentanyl may be due to the higher fat content in females leading to greater accumulation of the drug in that compartment and delayed redistribution and emergence time. In terms of the gender differences observed in the group that received Propofol–Remifentanil, it is important to mention that those differences have not been reported in the literature and there are no pharmacokinetic, pharmacodynamic or pharmacogenetic explanations to date for these findings, warranting new studies.
ConclusionsThe use of Stangraf-controlled Fentanyl–Propofol is equivalent to the use of Remifentanil–Propofol (manual infusion) in terms of emergence and discharge times. The use of a simulation software may avoid delays in emergence and discharge times when Fentanyl infusion is administered. Additional studies are required in order to confirm the findings.
The use of Fentanyl–Propofol is associated with a higher requirement of Propofol with the infusion approach used in this study.
The Propofol–Remifentanil-based technique is associated with a higher incidence of intraoperative hypotension.
Additional studies are required in order to assess differences between emergence times among genders when using a Propofol–Remifentanil-based technique.
EthicsThe Research Protocol was approved by the Universidad de El Rosario Ethics Committee and informed consent was obtained from the subjects in order to ensure compliance with Resolution 8430 issued in 1993 by the Ministry of Health and Social Protection.
FundingNone.
Conflict of interestNone declared.
- •
Basic monitoring: pulse oximetry, non-invasive blood pressure, electrocardiogram, capnography and muscle relaxation monitor. The depth of anesthesia will be monitored on the basis of clinical findings.
- •
Five minutes before induction, all patients will receive a dose of 50mcg/kg of midazolam.
- •
Propofol will be administered at a dose of 20mg/kg/h during the first 10min, 10mg/kg/h during the following 10min, 8mg/kg/h during the next 10min, and 6mg/kg/h during the remainder of the procedure. The infusion will be stopped at the time the surgeon starts skin closure.
- •
Patients will receive Remifentanil or Fentanyl-based TIVA according to the choice of the anesthesiologist in charge of the case.
- ∘
Remifentanil at a dose of 0.25mcg/kg/h for induction and, during the procedure, the dose range will be 0.1 and 0.25mcg/kg/h depending on patient requirements. The infusion will be stopped at the time the surgeon starts skin closure.
- ∘
Fentanyl at a dose of 20mcg/kg/h until the Stangraf simulation software indicates that the effect site concentration of 2.5ng/ml has been reached. At that point, the infusion will be reduced to 2mcg/kg/h, and this dose will be maintained during the rest of the procedure. The infusion will be stopped when the Stangraf simulation software shows that the estimated time to reach a plasma level of 1.0 is the same as the estimated time for completing the surgical procedure.
- ∘
- •
At the start of the surgery, all patients will receive 10mg of metoclopramide IV and 50mg of ranitidine IV.
- •
A dose of dipirone 50mg/kg IV and diclofenac 75mg IV will be given for analgesia.
- •
Patients requiring neuromuscular relaxation will be given a dose of 0.1mg/kg of cisatracurium as soon as palpebral reflex is lost. In the event reversal of neuromuscular blockade is required, neostigmine and atropine shall be given according to the anesthesiologist's judgment.
- •
In the event of light anesthesia, the patient will receive a bolus of propofol 40mg IV.
Please cite this article as: Pérez López DC, et al. Comparación del tiempo de despertar y tiempo de descarga entre dos tecnicas de anestesia total intravenosa manual: remifentanil vs fentanil. Rev Colomb Anestesiol. 2013;41:250–256.