The aim of this study is to determine the financial burden of preeclampsia (PE) from a single institution's perspective and then determine the cost of the illness from the reimbursement institution perspective and finally draw a regression model that predicts the annual cost of a patient.
Materials and methodsThe research is a descriptive and cross-sectional type of research and a retrospective cost analysis. Patients diagnosed with PE in 2021 were included in the study. For the regression analysis of the study, a dataset with 29 parameters belonging to 65 patients was created. Regression models were built on top of it.
ResultsIn our study, per-patient expenses of PE patients from the perspective of the reimbursement institution were calculated and presented as average costs; severe PE patient with cesarean section 7598.5 Ł ($769.8), severe PE patient with normal vaginal delivery 8487.48 Ł (1050.43 $), mild PE patient with cesarean section 5331.67 Ł ($659.86) and mild PE patient with normal vaginal delivery was calculated as 6220.65 Ł (769.88 $). In the study, different regression formulas were created for the two groups of PE. The created regression model had an R2 score of 91.85%.
ConclusionThe actors involved in the management of the disease should determine the cost-effectiveness of the disease by using the financial data of the patients and choose the right approach. Health costs in Turkey differ from the parameters in the European Union economy. Therefore, there are lower health costs. The financial findings of the disease are a guide for health policy makers, health managers and researchers.
El objetivo de este estudio es determinar la carga financiera de la preeclampsia (PE) desde la perspectiva de una única institución, para luego determinar los costes de la enfermedad desde la perspectiva de la institución de reembolso, y así elaborar un modelo de regresión que prediga el coste anual de un paciente.
Materiales y métodosSe trata de una investigación de tipo descriptivo, transversal y de un análisis retrospectivo de costes. Se incluyeron en el estudio los pacientes diagnosticados de PE en 2021. Para el análisis de regresión del estudio se creó un conjunto de datos con 29 parámetros que pertenecían a 65 pacientes diferentes. Los modelos de regresión se construyeron en base a este.
ResultadosEn nuestro estudio, los gastos por paciente de las pacientes con PE desde la perspectiva de la institución de reembolso se calcularon y presentaron como costos promedio; paciente con PE grave con cesárea 7598.5 (769.8 $), paciente con PE grave con parto vaginal normal 8487.48 (1050.43 $), paciente con PE leve con cesárea 5331.67 (659.86 $) y paciente con PE leve con parto vaginal normal se calculó como 6220.65 (769.88 $). En el estudio se crearon diferentes fórmulas de regresión para los dos grupos de PE. El modelo de regresión creado tuvo una puntuación R2 de 91,85%.
ConclusiónLos agentes implicados en la gestión de la enfermedad tendrán que determinar su rentabilidad utilizando los datos económicos de los pacientes y elegir el enfoque adecuado. Los costes sanitarios en Turquía difieren de los parámetros de la economía de la Unión Europea. Por tanto, los costes sanitarios se reducen. Los hallazgos financieros de la enfermedad servirán de guía para los responsables de las políticas de salud, los gerentes de salud y los investigadores.
One of the hypertensive diseases seen in pregnancy is preeclampsia (PE). PE is a disease of unknown cause, accompanied by proteinuria and/or organ damage, accompanied by high blood pressure after the 20th gestational week of a pregnant woman whose blood pressure was normal before the 20th week of pregnancy.1,2 Of the hypertension seen in 12–15% of all pregnancies, 70% is caused by PE and 30% is caused by chronic hypertension.3 PE is seen in many countries in the world and causes 10–15% of maternal deaths in the world.4 The severity of the disease is determined according to the clinical findings. This distinction is defined PE with and without severity features. In this way, it is very important to distinguish PE and to predict it before complications occur and to apply appropriate treatment protocols. PE is a difficult and costly disease with an important place in the medical literature to be diagnosed early.5
It is important for health enterprises to control costs in disease management as well as in financial management processes of other enterprises.6 Disease cost analysis (DCA) highlights the epidemiology of disease-related mortality and morbidity, guides medical research, and provides a basis for economically evaluating the effectiveness of new interventions.7
In the DCA literature, they are grouped as disease-specific or general disease cost studies. The purpose of general disease cost studies is to calculate the cost of health services for the year determined by using International Classification of Disease (ICD) codes.8 The maximum benefit amount to be obtained with DCA studies can be calculated. DCA studies provide the determination of the expenditures made for the opportunity cost of a particular disease in a particular population. In addition, it can be determined how much the benefit will be obtained by the recovery of the patients.9
Disease cost analysis perspectiveAfter determining the purpose in disease cost analysis research, it is necessary to determine the perspective of the cost.10 In DCA studies, it should be determined separately which cost element is incurred by those who bear the cost, such as the health enterprise, the state, the patient and the reimbursement institution. The included costs differ according to the chosen perspective. The costs in perspective are as follows11; medical costs, non-medical costs, mortality costs, morbidity costs are transfer payments.
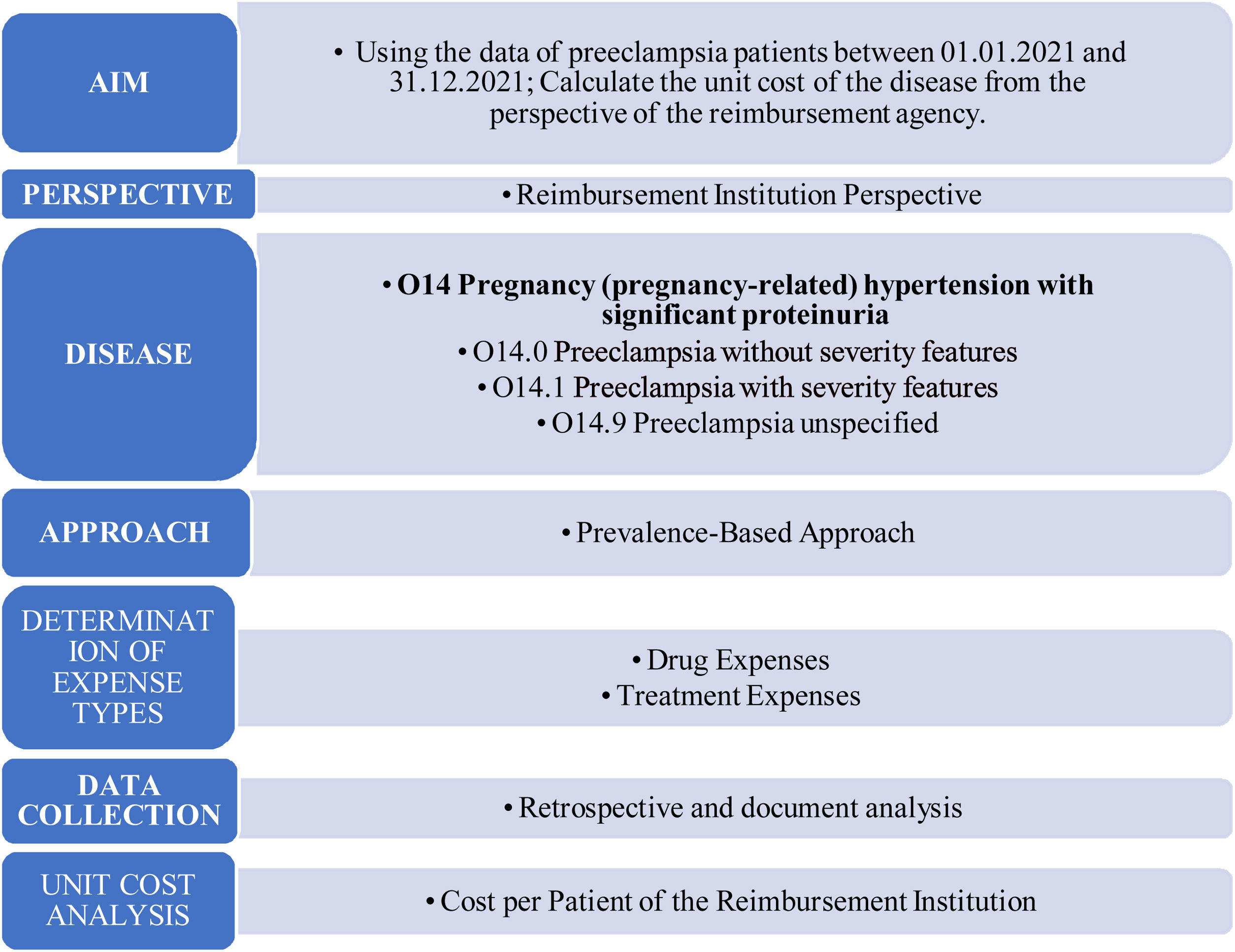
Disease cost analysis methodsIn the process of disease cost analysis, it consists of stages such as purpose, perspective, collection of disease data, analysis and reporting. The first stage, the goal setting stage, is very important. The next step is to decide which cost analysis approach to use. Subsequently, the types of expenses are determined and the cost analysis method is determined accordingly. After this stage, the methodology is defined. Expenses are determined and the available data is analyzed. At the last stage, reporting is done (Fig. 1).
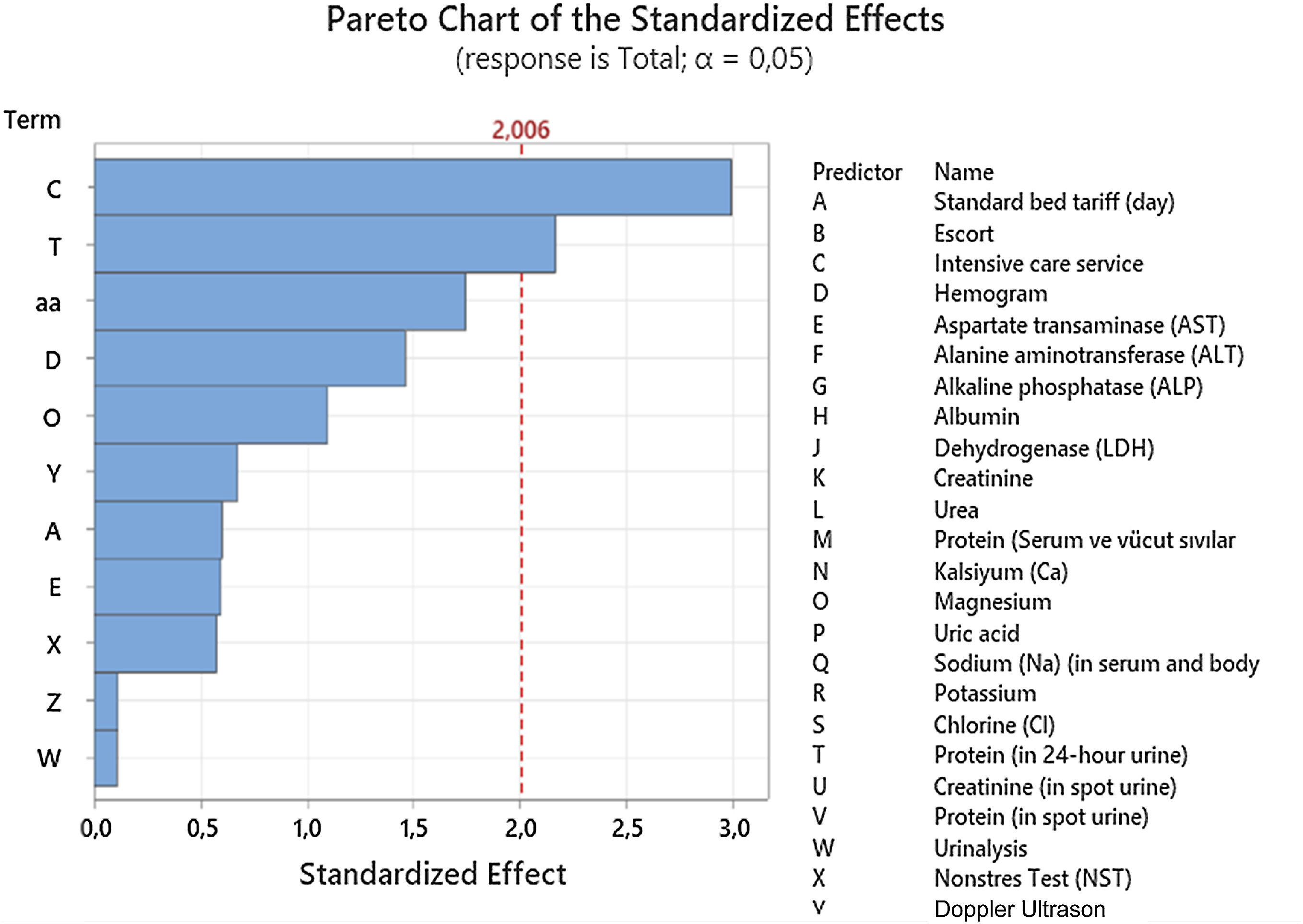
Linear regression analysis in determining disease costsRegression analysis is a statistical method used to analyze the relationship between dependent and independent variables and to model this relationship. Regression analysis is used to express the calculation of a dependent variable over different independent variables as a function, and to calculate the dependent variable with the help of this function. Regression analysis is a method used to estimate the annual costs of the disease. There are different techniques used to measure the success of regression analysis. The most preferred ones are R2 and Pareto analysis.
- -
R2: It is the percentage representation of the relationship between the dependent and independent variable.
- -
Pareto analysis: It is used to determine the effects of independent variables used in the calculation of a dependent variable.
- -
Adjacent R2: It is the subtraction of the ratio between the sum of square errors and sum of total squares.
- -
MSE: Squared difference between the actual value and the predicted value
Stevens et al.12 examined the short-term costs of PE in the USA in a study. In the study, in which annual costs were calculated, data from 2012 provided by the National Health Statistics Center were used. Considering the results, side effects during pregnancy increased from 4.6% to 10.1% in mothers and from 7.8% to 15.4% in children in cases with PE. Considering the annual cost, in all cases examined, the total cost in the first 12 months of the birth process was calculated as $1.03 billion for mothers and $1.15 billion for children.12
Hodel et al.13 conducted the first study to analyze PE costs in Switzerland in 2020. They used the databases of the finance and control departments to calculate the costs of patients with suspected or diagnosed PE in the study. 301 cases were included in the study. The cost of suspected PE was found to be €6658 on average, €12,974 for PE cases with vaginal delivery, and €21,507 for PE cases by cesarean section.13
Material and methodThe universe and sample of the studyThe reimbursement institution perspective and linear regression model universe of the study consists of 355 patients who received PE treatment between 01.01.2021 and 31.12.2021 at the Gynecology and Pediatrics Training and Research Hospital. ICD-10 diagnostic coding system, which is used in hospital automation systems, was used to identify cases with PE. Using this coding system, the sub-fractions of O14.0 (pre-eclampsia), O14.1 (PE with severity features) and 014.9 (pre-eclampsia) associated with PE with the diagnosis code O14 (Pregnancy [pregnancy-related] hypertension, significant proteinuria) were used. Eclampsia, unspecified were evaluated. In our dataset we used 11–20 weeks as gestational age and all data was taken from inpatients. In data gathering process we were able to obtain all test results for only 65 patients out of 355 patients which is why their data was used in further analysis. For the reimbursement institution perspective, the sample was not selected, and the entire universe was included in the study. The sample of the linear regression model consists of 65 PE patients. The regression model was built on 29 features and 10 of them were selected in the regression model.
Data collection method, tools and processThe direct medical costs in the Health Practice Communiqué (HPC) were used while conducting the cost analysis in terms of the reimbursement perspective of the study. The prescription information of the patients obtained from the hospital automation system and the e-prescription, https://www.ilacrehberi.com/ site was used. Medication costs of PE patients were used at the 2021 public price. In the study, the costs were calculated in Turkish Lira (Ł). The cost analysis results of the disease are also stated in Dollars ($) and T.C. The Central Bank's 2021 average rate is taken as a basis. Accordingly, 1 US Dollar ($) is taken as 8.08 Ł.
To create the linear regression model, a dataset consisting of 29 parameters belonging to 65 patients was created. The patients in the created dataset were selected according to the ICD-10 code and consisted of patients who did not have a secondary disease, did not develop complications during their hospitalization, and did not receive any treatment other than PE disease. Retrospective document analysis was made and Microsoft Excel program was used.
Linear regression analysisFor the regression analysis of the study, a 29-parameter dataset belonging to 65 patients was created. On this dataset, 2 different regression formulas were created depending on the PE with and without severity features. The importance degrees of the variables in the created regression models were determined by Pareto analysis.
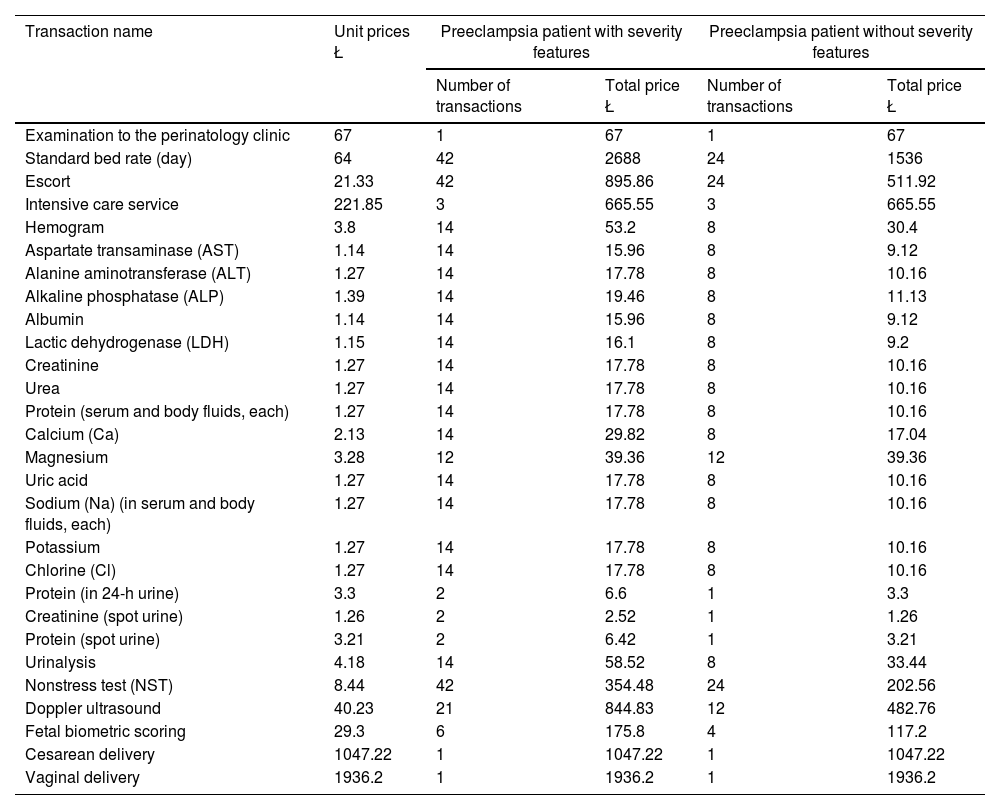
ResultsResults regarding treatment expensesSince the definitive treatment of preeclampsia is delivery, outpatient treatment, inpatient treatment and delivery services are used in the follow-up/treatment processes of the disease. While determining the treatment costs, some assumptions were made by making use of expert opinion and literature. The study includes the treatment costs of patients who comply with these assumptions. Table 1 shows information on the treatment costs of patients with preeclampsia.
Information on the treatment costs of preeclampsia patients.
| Transaction name | Unit prices Ł | Preeclampsia patient with severity features | Preeclampsia patient without severity features | ||
|---|---|---|---|---|---|
| Number of transactions | Total price Ł | Number of transactions | Total price Ł | ||
| Examination to the perinatology clinic | 67 | 1 | 67 | 1 | 67 |
| Standard bed rate (day) | 64 | 42 | 2688 | 24 | 1536 |
| Escort | 21.33 | 42 | 895.86 | 24 | 511.92 |
| Intensive care service | 221.85 | 3 | 665.55 | 3 | 665.55 |
| Hemogram | 3.8 | 14 | 53.2 | 8 | 30.4 |
| Aspartate transaminase (AST) | 1.14 | 14 | 15.96 | 8 | 9.12 |
| Alanine aminotransferase (ALT) | 1.27 | 14 | 17.78 | 8 | 10.16 |
| Alkaline phosphatase (ALP) | 1.39 | 14 | 19.46 | 8 | 11.13 |
| Albumin | 1.14 | 14 | 15.96 | 8 | 9.12 |
| Lactic dehydrogenase (LDH) | 1.15 | 14 | 16.1 | 8 | 9.2 |
| Creatinine | 1.27 | 14 | 17.78 | 8 | 10.16 |
| Urea | 1.27 | 14 | 17.78 | 8 | 10.16 |
| Protein (serum and body fluids, each) | 1.27 | 14 | 17.78 | 8 | 10.16 |
| Calcium (Ca) | 2.13 | 14 | 29.82 | 8 | 17.04 |
| Magnesium | 3.28 | 12 | 39.36 | 12 | 39.36 |
| Uric acid | 1.27 | 14 | 17.78 | 8 | 10.16 |
| Sodium (Na) (in serum and body fluids, each) | 1.27 | 14 | 17.78 | 8 | 10.16 |
| Potassium | 1.27 | 14 | 17.78 | 8 | 10.16 |
| Chlorine (Cl) | 1.27 | 14 | 17.78 | 8 | 10.16 |
| Protein (in 24-h urine) | 3.3 | 2 | 6.6 | 1 | 3.3 |
| Creatinine (spot urine) | 1.26 | 2 | 2.52 | 1 | 1.26 |
| Protein (spot urine) | 3.21 | 2 | 6.42 | 1 | 3.21 |
| Urinalysis | 4.18 | 14 | 58.52 | 8 | 33.44 |
| Nonstress test (NST) | 8.44 | 42 | 354.48 | 24 | 202.56 |
| Doppler ultrasound | 40.23 | 21 | 844.83 | 12 | 482.76 |
| Fetal biometric scoring | 29.3 | 6 | 175.8 | 4 | 117.2 |
| Cesarean delivery | 1047.22 | 1 | 1047.22 | 1 | 1047.22 |
| Vaginal delivery | 1936.2 | 1 | 1936.2 | 1 | 1936.2 |
Using the formula below, the outpatient treatment cost of the PE patient was calculated as 67 Ł.
It was learned that PE patients without severity features were diagnosed at an average of 34 weeks of gestation, received hospital inpatient treatment during delivery, and gave birth at an average of 37 weeks of gestation, by seeking expert opinion. Based on this information, it was assumed that patients with mild PE received an average of 28 days (4 weeks) of inpatient treatment. In the HPC Annex-2/C List (Diagnostic-Based Procedure List), the standard bed tariff is 64 Ł and the accompanying fee is 21.33. Inpatient service expense and attendant expense for mild PE patients were calculated using the formula below. The clinical bed service cost of the patients was 1536 Ł, the companion bed cost was 511.92 Ł, and a total of 2047.92 Ł, was found.
Expert opinion was sought to learn the mean gestational week and delivery week of PE patients with severity features. It was found that PE patients were diagnosed at an average of 28 weeks of gestation, inpatient treatment during delivery, and delivered at an average of 34 weeks of gestation. Based on this information, it was assumed that patients with PE with severity features received an average of 42 days (6 weeks) inpatient treatment. In the HPC Annex-2/B List (Per-Service Transaction List), the standard bed tariff is 64 Ł and the accompanying fee is 21.33 Ł. The cost of inpatient service and the expense of accompanying persons for PE patients with severity features were calculated using the formula below. The clinical bed service cost of the patients was found to be 2688 Ł, the accompanying bed cost was 895.86 Ł, and a total of 3583.86 Ł.
Results regarding medication expensesFrom the perspective of the reimbursement institution; One of the direct costs of PE patients is drug costs. Since the drugs prescribed to the patients are included in the HPC Annex-4/D List (Drug List Exempted from the Patient Participation Fee), no contribution fee is charged from the patient and all the drug fees are covered by the reimbursement institution. Adalat Crono Controlled Release Tablet (30mg) unit price is 1.53 Ł, Adalat Crono Controlled Release Tablet (60mg) 1.68 Ł, Alfamet Film Tablet 0.58 Ł and average unit price is 1.26 It was found as Ł. Monthly (calculated as 1 month and 30 days) total average drug cost incurred by the reimbursement institution was calculated as 37.8 Ł, and annual average drug cost (12 months*37.8) was calculated as 453.6 Ł.
Perspective of the reimbursement institution of PE patients, costs per patient;
- -
PE patient with severity features born by cesarean delivery 7598.5 Ł (769.8),
- -
PE with and without severity features with vaginal delivery 8487.48 Ł (1050.43 $),
- -
Cesarean delivery PE patient without severity features 5331.67 Ł (659.86 $),
- -
PE patient without severity features with vaginal delivery was calculated as 6220.65 Ł (769.88 $).
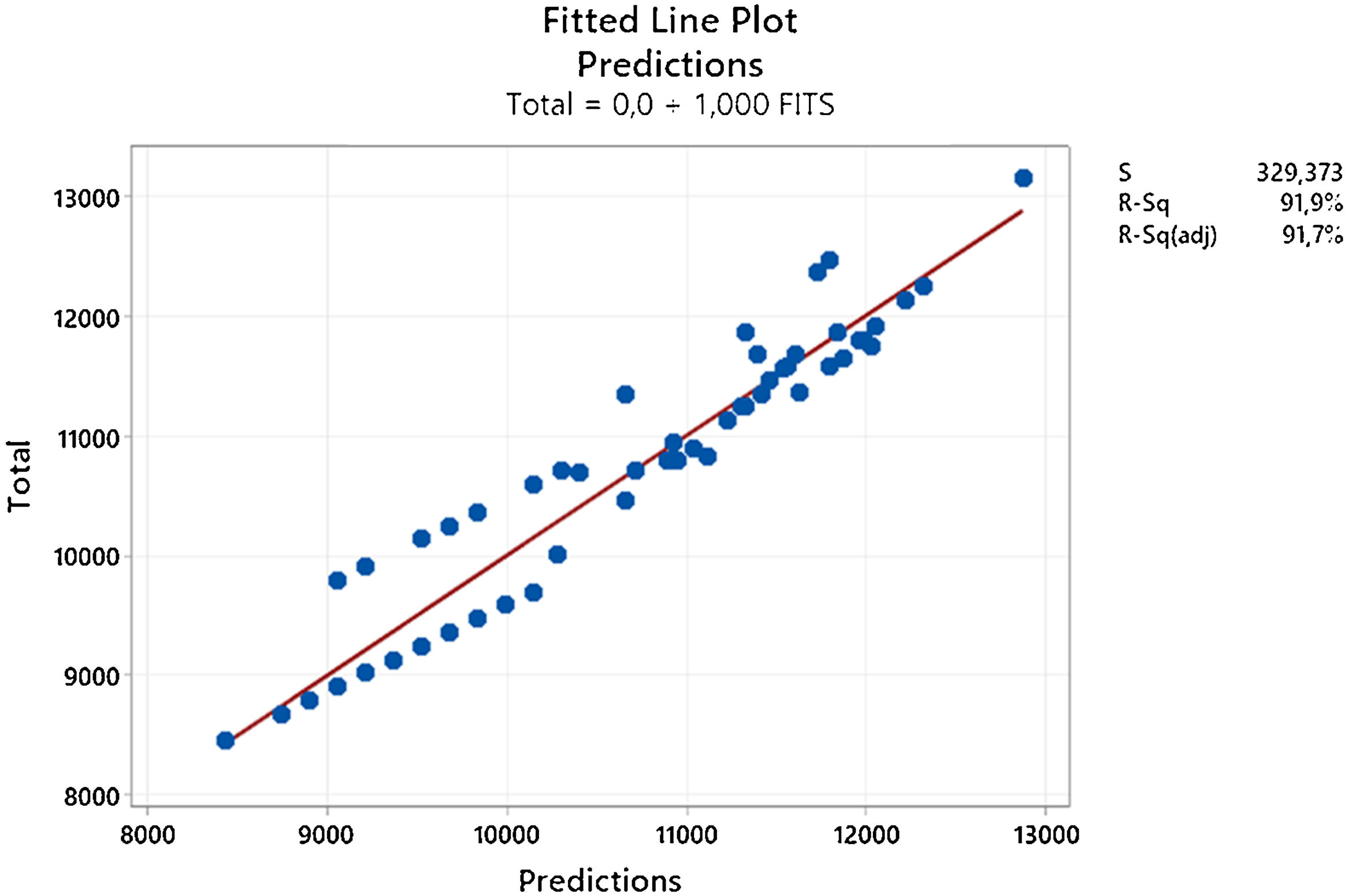
At this stage of the study, linear regression method was applied to determine the 1-year disease cost of the PE patient. 29 parameters of 65 PE patients were analyzed and based on these, the total cost for each patient was estimated. A linear regression model was created by selecting certain variables from among the 29 variables used. While creating the regression model, the 5 K-Fold validation method was used. R2 score was used to evaluate the success of the model, and Pareto analysis was used to determine the weights of the parameters.
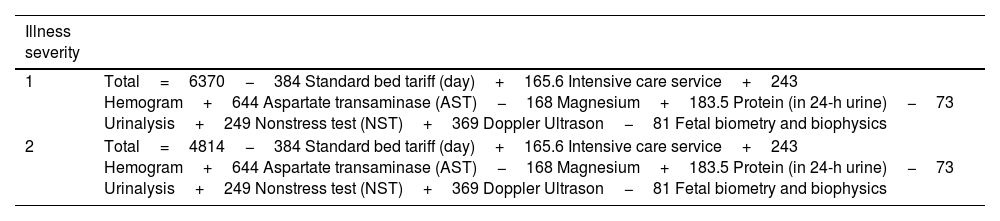
The regression model created 2 different formulas for PE according to disease severity (with or without severity features) given as a categorical and independent variable. In Table 2, the total cost formulas according to patient codes (1=PE with severity features, 2=PE without severity features) were determined by the regression model. As seen in the formulas, the constant coefficient was determined as 6370 for PE patients with severity features, and the regression model formulated that there was a higher cost in PE patients with severity features by keeping the constant value high.
Linear regression formulas according to patient codes.
| Illness severity | |
|---|---|
| 1 | Total=6370−384 Standard bed tariff (day)+165.6 Intensive care service+243 Hemogram+644 Aspartate transaminase (AST)−168 Magnesium+183.5 Protein (in 24-h urine)−73 Urinalysis+249 Nonstress test (NST)+369 Doppler Ultrason−81 Fetal biometry and biophysics |
| 2 | Total=4814−384 Standard bed tariff (day)+165.6 Intensive care service+243 Hemogram+644 Aspartate transaminase (AST)−168 Magnesium+183.5 Protein (in 24-h urine)−73 Urinalysis+249 Nonstress test (NST)+369 Doppler Ultrason−81 Fetal biometry and biophysics |
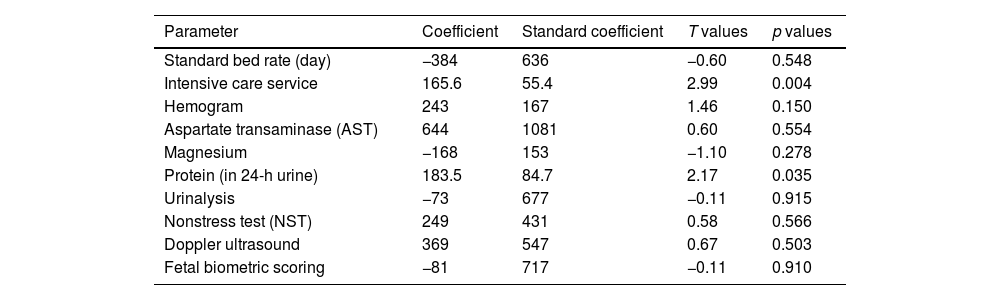
When Table 3 is examined, the parameters used in the regression model, their coefficients and p values are presented. The regression model used 10 of the 29 parameters in the data set in the formula. These variables are respectively; standard bed tariff, intensive care service, blood hemogram, AST, magnesium, protein, complete urinalysis, NST, doppler ultrasound and fetal biometric scoring. When the effects of these variables were examined, it was observed that the intensive care service and protein had a significant effect (p<0.05). The success score of the created regression model, R2, was calculated as 91.85%. For the same model Adjacent R2 score was obtained as 90.16%. The mean squared error (MSE) between the fits and actuals was calculated as 10514.7. The adjacent R2 shows the relation between sum of square errors and sum of total squares and shows the insight how the relation is between MSE and sum of total squares.
Coefficients and p values used in the regression model.
| Parameter | Coefficient | Standard coefficient | T values | p values |
|---|---|---|---|---|
| Standard bed rate (day) | −384 | 636 | −0.60 | 0.548 |
| Intensive care service | 165.6 | 55.4 | 2.99 | 0.004 |
| Hemogram | 243 | 167 | 1.46 | 0.150 |
| Aspartate transaminase (AST) | 644 | 1081 | 0.60 | 0.554 |
| Magnesium | −168 | 153 | −1.10 | 0.278 |
| Protein (in 24-h urine) | 183.5 | 84.7 | 2.17 | 0.035 |
| Urinalysis | −73 | 677 | −0.11 | 0.915 |
| Nonstress test (NST) | 249 | 431 | 0.58 | 0.566 |
| Doppler ultrasound | 369 | 547 | 0.67 | 0.503 |
| Fetal biometric scoring | −81 | 717 | −0.11 | 0.910 |
Fig. 2 shows the Pareto analysis of the regression model. The parameters were coded with letters and their standardized effects on the model were entered into Pareto analysis. According to the analysis, C (ICU) and T (protein in 24-h urine) have a significant effect on the regression model. Pareto analysis is in agreement with the results given in Table 3.
In Fig. 3, the connection between the regression model of the total costs of the patients and the estimated cost is presented. The total cost is shown with the red line, and the distribution of the estimates of the regression model is shown with the blue dots. As can be seen in the figure, the estimated values remained around the total cost line and no outlier point was not encountered. The R2 score of the model was calculated as 91.7% in this test.
DiscussionDiscussing the findings on the perspective of the reimbursement institutionIn this research, some of the encountered limitations were; the dataset was obtained from a single institution. The model was created from a limited number of PE patients. 65 patients used in the research did not have a secondary disease. This model is limited to the treatment costs of these pregnant women and could not be generalized, since it is created by using only the treatment expenses specific to PE disease.
Direct costs of PE patients for the work reimbursement agency (SSI); includes treatment costs and drug costs. Since PE patients are usually followed up in an inpatient setting, the cost of outpatient care was calculated as 67 Ł. The average unit cost of drugs used by PE patients was 1.26 Ł, and the monthly average cost reflected to SSI was calculated as 37.8 Ł.
Hodel et al.13 examined the costs of 301 cases in a study they conducted in Switzerland. The average cost per patient hospitalized for suspected PE was €6658, €12,974 for PE cases with vaginal delivery, and €21,507 for PE cases with cesarean delivery.13 Hao et al.14 examined birth records in the US healthcare system between 2010 and 2015. When the average costs of pregnancies were examined, it was found that the cost was 41,790 $ in the PE group and 13,187 $ in the group without PE.14 In a study examining pregnant women with hypertension, the costs of groups consisting of 97 PE patients and 133 healthy pregnant women were compared. As a result of the study, the cost per patient for PE was found to be 19.7% higher on average. Considering all pregnancy costs, it was found to be 9150 € in the group with PE patients and 7485 € in healthy pregnant women.15 In our study, per-patient expenses of PE patients from the perspective of the reimbursement institution; PE patient with cesarean section 7598.5 Ł ($769.8), PE patient with severity features with vaginal delivery 8487.48 Ł (1050.43 $), PE patient without severity features with cesarean section 5331.67 Ł ($659.86), normal mild PE patient born vaginally was calculated as 6220.65 Ł (769.88 $).
Discussing the findings on regression analysisIn order to estimate the cost per patient of preeclampsia, a estimation study was carried out using the linear regression method. A limited number of studies have been observed using the regression method in cost analysis. No study was found in the literature with a similar scope like this study. The discussion of the findings of this part of the study is presented below.
Zakiyah et al.16 conducted a cost–benefit analysis on early PE screening for women with a first pregnancy. In the study, 25 different scenarios were analyzed for 100,000 pregnant women and a regression decision tree was created.16 With the regression model created as a result of the study, it was seen that early PE screening saved €50,000 per case in the Netherlands and €100,000 in Sweden. Chantraine et al.17 examined the utility of sFlt-1 (soluble fms-like tyrosine kinase 1)/PlGF (placental growth factor) ratio in the prediction of PE disease in a different study. In the study, 1 year data was used. In cases where the sFl1-1/PIGF ratio is made in parallel with the existing tests, early diagnosis and cost–benefit analysis were performed, and the data of approximately 100,000 patients were examined in the examinations made in the Belgian health system and the cost effect was examined in the patient group tested. It resulted in a savings of €712 per patient in the tested scenario.17 In our study, a regression model was created with 29 parameters of 65 PE patients and linear regression was used to calculate the total cost of PE per patient. Inpatients were divided into two groups as PE patients with severity features and PE patients without severity features. Different regression formulas were created for these two groups. The created regression formulas had a R2 score of 91.85% for both groups. Then, the weighted variables determining the cost estimation were determined by Pareto analysis.
ConclusionPreeclampsia, pregnancy-associated hypertension, proteinuria and/or organ dysfunction accompanying is a disease of unknown cause. PE is specific to pregnancy and damages the body by affecting many organs and systems.
The repayment institution perspective of preeclampsia, the regression model and the total cost per patient findings are given below:
- -
In our study, per-patient expenses of PE patients in the institution from the perspective of the reimbursement institution were calculated as; PE patient with severity features with cesarean section 7598.5 Ł ($769.8), PE patient with vaginal delivery 8487.48 Ł (1050.43 $), PE patient without severity features with cesarean section 5331.67 Ł ($659.86), PE patient born vaginally was calculated as 6220.65 Ł (769.88 $).
- -
Two different linear regression models with 91.85% R2 score were calculated.
In the study, while creating the regression model, a limited data set was studied. While creating the dataset, patients who did not have a secondary disease other than PE and did not develop complications during their inpatient treatment were selected. Demographic diversity was not included in the analysis because the data were obtained from a single institution. This limited the applicability of the model.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Patient consentWe have followed the protocols of Zeynep Kamil Training and Research Hospital regarding the publication of patient data, that they have the written consent of their patients for publication.
Ethical approvalThe ethical approval of this study has been granted by University of Health Sciences (Istanbul) on 4th June 2021 with the meeting number 2021/19.
FundingAuthors received no funding for this project.
Conflict of interestThe authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
This article was produced from Ülkü Veranyurt's doctoral thesis titled “Examining the Health Costs of Preeclampsia and Creating a Disease Management Model with an Artificial Intelligence Based Early Diagnosis Clinical Decision Support System” conducted under the supervision of Betül Akalın.