Arterial hypertension and dyslipidemia are two of the most relevant modifiable cardiovascular risk factors (CVRFs), and they often coexist. No recent studies specifically evaluating the achievement of LDL-C and blood pressure (BP) targets in hypertensive patients with dyslipidemia are available in Spain.
MethodsThe SNAPSHOT study was a multicenter, cross-sectional observational study conducted in cardiology and internal medicine (IM) departments/clinics and primary care (PC) centers in Spain. The study enrolled consecutive adult patients (≥18 years of age) diagnosed with both hypertension and dyslipidemia. The primary endpoint was the percentage of patients achieving both the LDL-C goals recommended by the 2021 European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) guidelines and the BP targets established in the 2018 ESC/European Society of Hypertension (ESH) guidelines. Cardiovascular (CV) risk (very high, high, low-to-moderate) was centrally assessed according to the updated Systematic Coronary Risk Evaluation (SCORE2) and SCORE2-Older Person (OP) algorithms recommended in the 2021 ESC guidelines.
ResultsBetween December 2021 and April 2022, a total of 443 evaluable patients were enrolled (males: 54%; ≥65 years of age: 66.1%; obesity: 37.4%; diabetes mellitus: 37.3%; coronary artery disease [CAD]: 25.7%). Out of the 388 patients in whom CV risk could be assessed, 34.3% and 56.4% were considered as having high and very high risk, respectively. Overall, 24% of the patients had achieved their risk-based LDL-C goals (21.8% of the patients at high-CV risk and 25.1% of those at very high risk), and 30.3% of the patients had reached the recommended BP targets (27.1% of the patients at high risk and 36.1% of those at very high risk). A total of 8.8% of the patients had achieved both the LDL-C and BP targets. Overall, 51.4% of the patients with concurrent diabetes had achieved glycemic control (HbA1c <7%), while only 9.4% of the diabetic patients had reached simultaneous control of LDL-C, BP and HbA1C targets (7.8% of the patients at high risk and 10.4% of those at very high risk).
ConclusionThe attainment of LDL-C and BP goals is still suboptimal in patients with dyslipidemia and hypertension in the real-world setting in Spain, with approximately 75% of the patients at very high risk of cardiovascular disease failing to reach their risk-based LDL-C and BP targets. Additionally, the rate corresponding to simultaneous control of LDL-C, BP and HbA1c is likewise very low. The present study thus highlights the current challenge of controlling multiple CVRFs that significantly contribute to atherosclerotic cardiovascular disease events and mortality and emphasizes the need for more effective management of CVRFs in the real-world setting.
La hipertensión arterial y la dislipidemia son dos de los factores de riesgo cardiovascular modificables (FRCVs) más relevantes y, a menudo, coexisten en el paciente. En España, no se dispone de estudios recientes que evalúen específicamente la consecución de los objetivos de colesterol unido a lipoproteínas de baja densidad (c-LDL) y presión arterial (PA) en pacientes con hipertensión y dislipidemia.
MétodosSNAPSHOT fue un estudio observacional transversal y multicéntrico llevado a cabo en servicios/clínicas de cardiología y medicina interna y en centros de atención primaria de España. Se incluyeron de forma consecutiva pacientes adultos (≥18 años) diagnosticados con hipertensión y dislipidemia. El criterio de valoración primario fue el porcentaje de pacientes que alcanzaron tanto los objetivos de c-LDL recomendados por las guías de la Sociedad Europea de Cardiología/Sociedad Europea de Aterosclerosis (ESC/EAS, de sus siglas en inglés de European Society of Cardiology/European Atherosclerosis Society) de 2021 como los de PA establecidos en las guías de la ESC/Sociedad Europea de Hipertensión (ESH, de sus siglas en inglés de European Society of Hypertension) de 2018. El riesgo cardiovascular (CV) (muy alto, alto, bajo a moderado) se evaluó de forma centralizada según los algoritmos actualizados de la Evaluación Sistemática del Riesgo Coronario (SCORE2, de sus siglas en inglés de Systematic Coronary Risk Evaluation) y SCORE2 para personas mayores (OP, de sus siglas en inglés de Older Person), recomendados en las guías de la ESC de 2021.
ResultadosEntre diciembre de 2021 y abril de 2022 se incluyeron un total de 443 pacientes evaluables (varones: 54%; ≥65 años: 66,1%; obesidad: 37,4%; diabetes mellitus: 37,3%; enfermedad arterial coronaria: 25,7%). De los 388 pacientes en los que se pudo evaluar el riesgo CV, el 34,3% y el 56,4% se consideraron de riesgo alto y muy alto, respectivamente. El 24% de los pacientes habían alcanzado los objetivos de c-LDL en función de su riesgo CV (21,8% de los pacientes con riesgo alto y 25,1% de los pacientes con riesgo muy alto), y el 30,3% habían alcanzado los objetivos de PA recomendados (27,1% de los pacientes con riesgo alto y 36,1% de los pacientes con riesgo muy alto). El 8,8% de los pacientes habían alcanzado los objetivos tanto de c-LDL como de PA. El 51,4% de pacientes con diabetes concurrente habían logrado el control glucémico (HbA1c <7%), mientras que solo el 9,4% de los pacientes diabéticos habían alcanzado el control simultaneo de los objetivos de c-LDL, PA y HbA1c (7,8% de pacientes con riesgo alto y 10,4% pacientes con riesgo muy alto).
ConclusionesLa consecución de los objetivos de c-LDL y PA recomendados sigue siendo subóptima en pacientes con dislipidemia e hipertensión en condiciones de vida real en España, y aproximadamente el 75% de los pacientes con riesgo muy alto no alcanzan los objetivos de c-LDL y PA según su riesgo CV. Además, la tasa de consecución del control simultáneo de c-LDL, PA y HbA1c es muy baja también. Este estudio destaca el desafío actual de controlar múltiples FRCVs, que contribuyen significativamente a los eventos asociados a la enfermedad cardiovascular aterosclerótica y a la mortalidad, y enfatiza la necesidad de un manejo clínico de los FRCVs más efectivo en condiciones de vida real.
According to the World Health Organization (WHO), arterial hypertension affects 1.28 billion individuals worldwide.1 Hypertension represents the leading preventable cause of atherosclerotic cardiovascular disease (ASCVD) and all-cause mortality globally.2 In addition, hypertension is responsible for 48% of all strokes and 18% of all coronary events.3 In 2019, it accounted for one-fifth of all reported deaths, i.e., approximately 11 million.4 Most hypertensive patients present with other cardiovascular risk factors (CVRFs) such as smoking, obesity, diabetes, or physical inactivity.5,6 Lipid disorders observed in hypertensive patients mainly include elevated low-density lipoprotein cholesterol (LDL-C) and atherogenic dyslipidemia.7 Hypertension has been shown to often coexist with dyslipidemia.8 The concurrent presence of other CVRFs in hypertensive patients results in an increased risk of ASCVD and mortality.6 Data from the INTERHEART study revealed that individual risk factors generally increase the overall risk of cardiovascular disease two- to threefold.9 However, the concurrent presence of hypertension, diabetes, dyslipidemia, and smoking in the same individual led to an over 20-fold increase in cardiovascular disease risk compared to those with hypertension alone. Therefore, controlling all risk factors has become essential for the prevention of ASCVD events. The European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) recommend the reduction of LDL-C levels to established LDL-C targets according to patient cardiovascular (CV) risk in order to prevent ASCVD, especially in high- and very high-CV risk individuals.10 In fact, a reduction of 1mmol/L LDL-C has been associated with a relative risk reduction of up to 23% in terms of major vascular and coronary events, and 10% in terms of overall 5-year mortality.10,11 Nevertheless, in the real-world setting, a large proportion of patients do not reach the LDL-C targets according to their CV risk.12–14 Despite the available literature on the achievement of LDL-C goals, studies specifically focused on the concomitant control of blood pressure (BP) and LDL-C are limited,15–19 especially after the release of the 2021 ESC/EAS updated guidelines.20 Furthermore, none of the available real-world evidence studies have been carried out in Spain over the last few years.
The SNAPSHOT study was an international, multicenter, cross-sectional observational study aimed at describing achievement of the guideline-recommended risk-based LDL-C goals (2021 ESC/EAS guidelines)20 and BP targets (2018 ESC/European Society of Hypertension [ESH] guidelines)21 in patients with hypertension and dyslipidemia from European countries in the primary care and specialized healthcare settings. The present article describes the results of the Spanish subset of patients from the SNAPSHOT study.
MethodsStudy design and patientsThe SNAPSHOT Spain study was a multicenter, cross-sectional observational study conducted in the cardiology and internal medicine departments/clinics and primary care (PC) centers at 21 sites (50 investigators) in Spain. It was conducted in accordance with the World Medical Association Declaration of Helsinki and Spanish national regulations. The study protocol was approved by the independent Ethics Committee of La Paz Hospital (Madrid, Spain) and the corresponding health authorities.
The study enrolled consecutive adults (aged 18 years or older) diagnosed with arterial hypertension (systolic blood pressure [SBP] ≥140mmHg and/or diastolic blood pressure [DBP] ≥90mmHg or receiving BP-lowering therapy) and dyslipidemia (LDL-C ≥116mg/dL [≥3.0mmol/L] or receiving lipid-lowering therapy [LLT]), who provided written informed consent before inclusion in the study.
A cross-sectional chart review was performed to collect patients’ demographic (age, gender) and clinical data including anthropometric data (body mass index [BMI]), prior cardiovascular disease/events (i.e., coronary artery disease [CAD]), presence and type of kidney disease, and smoking status, and data related to hypertension (time since diagnosis, BP), dyslipidemia (time since diagnosis, lipid parameters levels) and diabetes (HbA1c, fasting glucose levels and diabetes-related complications) as well as treatment-related data for the management of hypertension, dyslipidemia and diabetes, respectively.
The primary endpoint was the percentage of patients achieving both the LDL-C goals recommended by the 2021 ESC/EAS guidelines10 (<1.4mmol/L [55mg/dL] for very high risk, <1.8mmol/L [70mg/dL] for high risk, and <2.6mmol/L [100mg/dL] for low-moderate risk patients) and the BP targets established in the 2018 ESC/ESH guidelines21 (treated patients: SBP/DBP <130/80mmHg in patients aged 18–65 years without chronic kidney disease [CKD] and <140/80mmHg in patients aged <65 years with CKD and patients aged ≥65 years; non-treated patients: SBP/DBP <140/90mmHg in patients aged <80 years and <160/90mmHg in patients aged ≥80 years). Cardiovascular risk (very high, high, low-to-moderate) was assessed according to the 2021 ESC guidelines.20 Secondary endpoints included the percentage of patients with controlled BP and the percentage of patients with controlled LDL-C levels, and the percentage of patients achieving the simultaneous recommended LDL-C and BP control targets as well as the glycosylated hemoglobin (HbA1c) targets for glycemic control (HbA1c <7% [<53mol/mL]).
Statistical considerationsTo describe quantitative variables, measures of central tendency and dispersion, including the mean, standard deviation (SD), median and interquartile range (IQR), were used. Counts and percentages were used to describe qualitative variables. For the comparison of categorical variables, the Chi-squared test was used.
Post hoc analyses were performed to assess the achievement of BP and LDL-C goals according to patient cardiovascular risk (very high, high, low-to-moderate), in relation to age and sex, obesity, and in the subgroups of patients at very high-CV risk, including those patients with diabetes and coronary artery disease (CAD). Post hoc analyses were also conducted to describe the achievement of BP and LDL-C goals as well as HbA1C target concentration according to the primary care or specialized (cardiology and internal medicine) setting.
Missing data were not considered in the analyses, and a significance level of 0.05 was used for statistical testing. The statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 17.0 (SPSS Inc., Chicago, IL, USA).
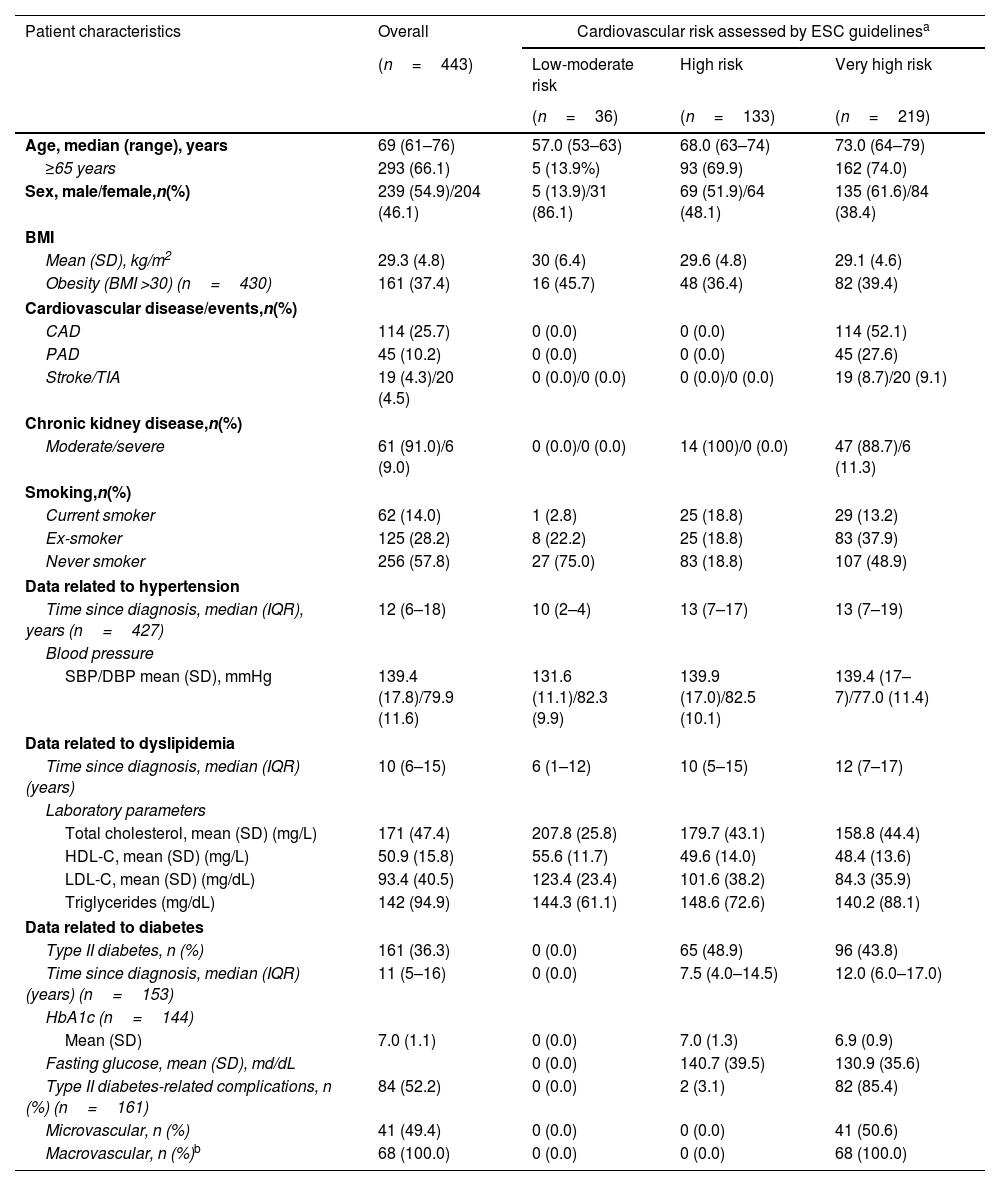
ResultsPatients and cardiovascular riskBetween December 2021 and April 2022, a total of 473 patients were enrolled in cardiology (n=124) and internal medicine (n=138) departments/clinics and primary care centers (n=181). Of these patients, 30 were excluded due to unavailable or incomplete data on LDL-C and BP required to verify compliance with the eligibility criteria. Thus, 443 patients were evaluable for study analyses in the overall study population. Of these patients, 388 had available clinical data for CV risk assessment. When CV risk was centrally assessed using the SCORE2 and SCORE2-Older Person (OP) algorithms (n=388 patients), 34.3% (n=133) and 56.4% (n=219) were considered as having high and very high risk, respectively. The demographic and clinical characteristics of the overall study population and according to cardiovascular risk (very high, high, low-to-moderate) are reported in Table 1. The median age was 69 years (61–76), with 66.1% of the patients being ≥65 years of age (13.3% ≥80 years), and 54.9% were males. Overall, 122 of the patients (27.5%) had isolated systolic hypertension. Regarding concurrent CVRFs, 37.4% of the patients had obesity and 37.3% diabetes (36.3% type II diabetes), 37.6% of them with target organ damage, and 13.8% had moderate chronic kidney disease (CKD). Overall, 25.7% of the patients had CAD. The mean LDL-C level was 93.4 (40.5)mg/dL in the overall study population. The mean HbA1c level was 7.0 (1.1)%.
Sociodemographic and clinical characteristics in the overall population and by cardiovascular risk.
| Patient characteristics | Overall | Cardiovascular risk assessed by ESC guidelinesa | ||
|---|---|---|---|---|
| (n=443) | Low-moderate risk | High risk | Very high risk | |
| (n=36) | (n=133) | (n=219) | ||
| Age, median (range), years | 69 (61–76) | 57.0 (53–63) | 68.0 (63–74) | 73.0 (64–79) |
| ≥65 years | 293 (66.1) | 5 (13.9%) | 93 (69.9) | 162 (74.0) |
| Sex, male/female,n(%) | 239 (54.9)/204 (46.1) | 5 (13.9)/31 (86.1) | 69 (51.9)/64 (48.1) | 135 (61.6)/84 (38.4) |
| BMI | ||||
| Mean (SD), kg/m2 | 29.3 (4.8) | 30 (6.4) | 29.6 (4.8) | 29.1 (4.6) |
| Obesity (BMI >30) (n=430) | 161 (37.4) | 16 (45.7) | 48 (36.4) | 82 (39.4) |
| Cardiovascular disease/events,n(%) | ||||
| CAD | 114 (25.7) | 0 (0.0) | 0 (0.0) | 114 (52.1) |
| PAD | 45 (10.2) | 0 (0.0) | 0 (0.0) | 45 (27.6) |
| Stroke/TIA | 19 (4.3)/20 (4.5) | 0 (0.0)/0 (0.0) | 0 (0.0)/0 (0.0) | 19 (8.7)/20 (9.1) |
| Chronic kidney disease,n(%) | ||||
| Moderate/severe | 61 (91.0)/6 (9.0) | 0 (0.0)/0 (0.0) | 14 (100)/0 (0.0) | 47 (88.7)/6 (11.3) |
| Smoking,n(%) | ||||
| Current smoker | 62 (14.0) | 1 (2.8) | 25 (18.8) | 29 (13.2) |
| Ex-smoker | 125 (28.2) | 8 (22.2) | 25 (18.8) | 83 (37.9) |
| Never smoker | 256 (57.8) | 27 (75.0) | 83 (18.8) | 107 (48.9) |
| Data related to hypertension | ||||
| Time since diagnosis, median (IQR), years (n=427) | 12 (6–18) | 10 (2–4) | 13 (7–17) | 13 (7–19) |
| Blood pressure | ||||
| SBP/DBP mean (SD), mmHg | 139.4 (17.8)/79.9 (11.6) | 131.6 (11.1)/82.3 (9.9) | 139.9 (17.0)/82.5 (10.1) | 139.4 (17–7)/77.0 (11.4) |
| Data related to dyslipidemia | ||||
| Time since diagnosis, median (IQR) (years) | 10 (6–15) | 6 (1–12) | 10 (5–15) | 12 (7–17) |
| Laboratory parameters | ||||
| Total cholesterol, mean (SD) (mg/L) | 171 (47.4) | 207.8 (25.8) | 179.7 (43.1) | 158.8 (44.4) |
| HDL-C, mean (SD) (mg/L) | 50.9 (15.8) | 55.6 (11.7) | 49.6 (14.0) | 48.4 (13.6) |
| LDL-C, mean (SD) (mg/dL) | 93.4 (40.5) | 123.4 (23.4) | 101.6 (38.2) | 84.3 (35.9) |
| Triglycerides (mg/dL) | 142 (94.9) | 144.3 (61.1) | 148.6 (72.6) | 140.2 (88.1) |
| Data related to diabetes | ||||
| Type II diabetes, n (%) | 161 (36.3) | 0 (0.0) | 65 (48.9) | 96 (43.8) |
| Time since diagnosis, median (IQR) (years) (n=153) | 11 (5–16) | 0 (0.0) | 7.5 (4.0–14.5) | 12.0 (6.0–17.0) |
| HbA1c (n=144) | ||||
| Mean (SD) | 7.0 (1.1) | 0 (0.0) | 7.0 (1.3) | 6.9 (0.9) |
| Fasting glucose, mean (SD), md/dL | 0 (0.0) | 140.7 (39.5) | 130.9 (35.6) | |
| Type II diabetes-related complications, n (%) (n=161) | 84 (52.2) | 0 (0.0) | 2 (3.1) | 82 (85.4) |
| Microvascular, n (%) | 41 (49.4) | 0 (0.0) | 0 (0.0) | 41 (50.6) |
| Macrovascular, n (%)b | 68 (100.0) | 0 (0.0) | 0 (0.0) | 68 (100.0) |
ACS: acute coronary syndrome; HbA1c: haemoglobin A1c; HDL: high-density lipoprotein (HDL) cholesterol; LDL-C: low-density lipoprotein (HDL) cholesterol; IQR: interquartile range; SD: standard deviation; TIA: transient ischemic attack.
Of evaluable patient population (n=443), 388 patients had available clinical data for CV risk assessment using the SCORE2 and SCORE2-OP algorithms recommended in the 2021 ESC/EAS guidelines. When CV risk was centrally assessed using the SCORE2 and SCORE2-OP algorithms, 34.3% (n=133) and 56.4% (n=219) were considered as having high and very high risk, respectively, and 36 (9.3%) as having low-moderate risk.
The demographic and clinical characteristics of the overall study population by healthcare setting/physician specialty are shown in Supplementary Table 1.
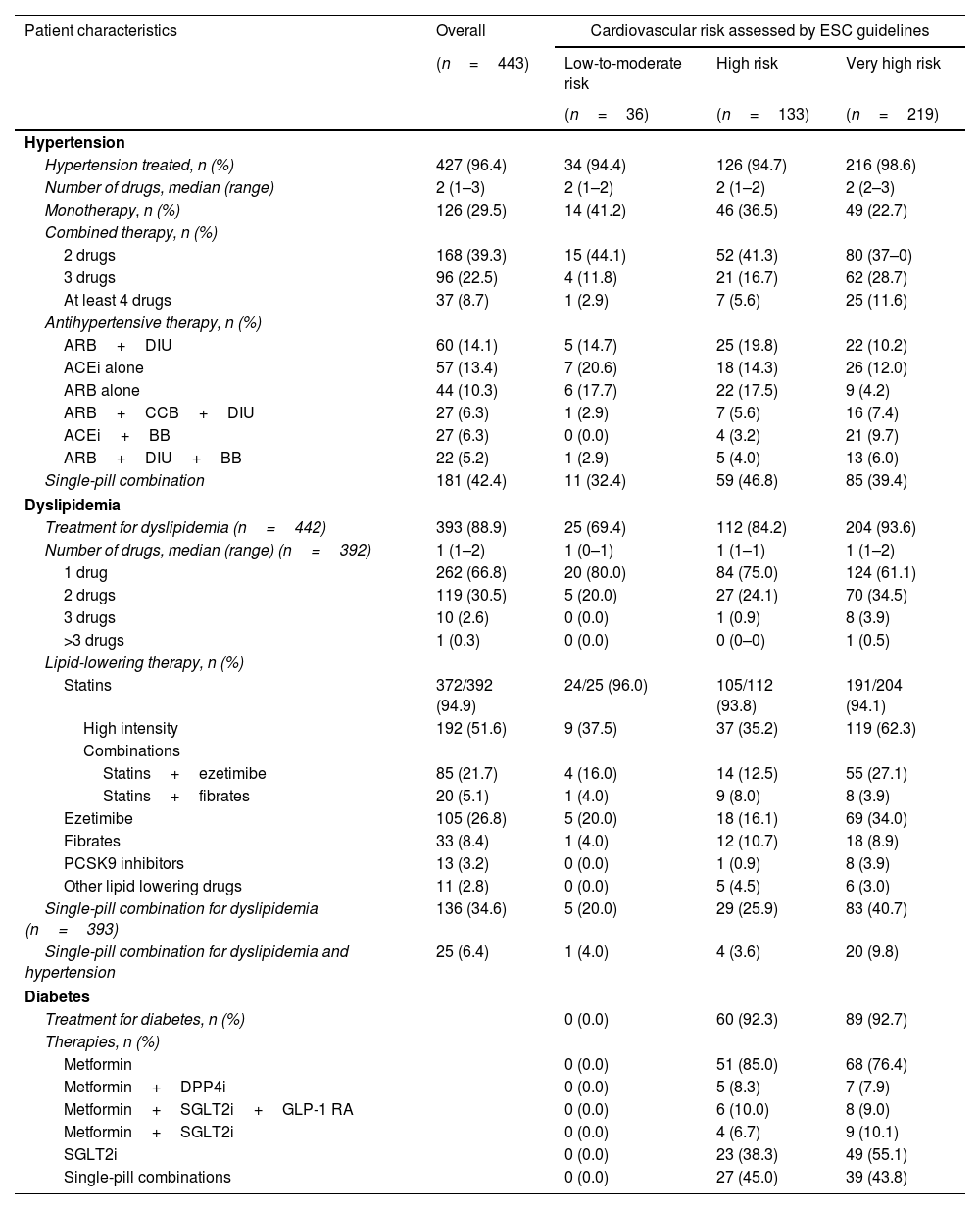
Treatment for hypertension, dyslipidemia, and diabetesThe treatment received for hypertension in the overall population and according to CV risk is shown in Table 2. Overall, 96.4% of the patients (n=427) received treatment for hypertension, involving a median of 2 (1-3) drugs, with 39.3% and 22.5% of the patients receiving 2 and 3 drugs, respectively. Overall, 42.4% of the patients (n=181) were treated with fixed-dose combinations for hypertension.
Treatment for hypertension, dyslipidemia, and diabetes in the overall population and by cardiovascular risk.
| Patient characteristics | Overall | Cardiovascular risk assessed by ESC guidelines | ||
|---|---|---|---|---|
| (n=443) | Low-to-moderate risk | High risk | Very high risk | |
| (n=36) | (n=133) | (n=219) | ||
| Hypertension | ||||
| Hypertension treated, n (%) | 427 (96.4) | 34 (94.4) | 126 (94.7) | 216 (98.6) |
| Number of drugs, median (range) | 2 (1–3) | 2 (1–2) | 2 (1–2) | 2 (2–3) |
| Monotherapy, n (%) | 126 (29.5) | 14 (41.2) | 46 (36.5) | 49 (22.7) |
| Combined therapy, n (%) | ||||
| 2 drugs | 168 (39.3) | 15 (44.1) | 52 (41.3) | 80 (37–0) |
| 3 drugs | 96 (22.5) | 4 (11.8) | 21 (16.7) | 62 (28.7) |
| At least 4 drugs | 37 (8.7) | 1 (2.9) | 7 (5.6) | 25 (11.6) |
| Antihypertensive therapy, n (%) | ||||
| ARB+DIU | 60 (14.1) | 5 (14.7) | 25 (19.8) | 22 (10.2) |
| ACEi alone | 57 (13.4) | 7 (20.6) | 18 (14.3) | 26 (12.0) |
| ARB alone | 44 (10.3) | 6 (17.7) | 22 (17.5) | 9 (4.2) |
| ARB+CCB+DIU | 27 (6.3) | 1 (2.9) | 7 (5.6) | 16 (7.4) |
| ACEi+BB | 27 (6.3) | 0 (0.0) | 4 (3.2) | 21 (9.7) |
| ARB+DIU+BB | 22 (5.2) | 1 (2.9) | 5 (4.0) | 13 (6.0) |
| Single-pill combination | 181 (42.4) | 11 (32.4) | 59 (46.8) | 85 (39.4) |
| Dyslipidemia | ||||
| Treatment for dyslipidemia (n=442) | 393 (88.9) | 25 (69.4) | 112 (84.2) | 204 (93.6) |
| Number of drugs, median (range) (n=392) | 1 (1–2) | 1 (0–1) | 1 (1–1) | 1 (1–2) |
| 1 drug | 262 (66.8) | 20 (80.0) | 84 (75.0) | 124 (61.1) |
| 2 drugs | 119 (30.5) | 5 (20.0) | 27 (24.1) | 70 (34.5) |
| 3 drugs | 10 (2.6) | 0 (0.0) | 1 (0.9) | 8 (3.9) |
| >3 drugs | 1 (0.3) | 0 (0.0) | 0 (0–0) | 1 (0.5) |
| Lipid-lowering therapy, n (%) | ||||
| Statins | 372/392 (94.9) | 24/25 (96.0) | 105/112 (93.8) | 191/204 (94.1) |
| High intensity | 192 (51.6) | 9 (37.5) | 37 (35.2) | 119 (62.3) |
| Combinations | ||||
| Statins+ezetimibe | 85 (21.7) | 4 (16.0) | 14 (12.5) | 55 (27.1) |
| Statins+fibrates | 20 (5.1) | 1 (4.0) | 9 (8.0) | 8 (3.9) |
| Ezetimibe | 105 (26.8) | 5 (20.0) | 18 (16.1) | 69 (34.0) |
| Fibrates | 33 (8.4) | 1 (4.0) | 12 (10.7) | 18 (8.9) |
| PCSK9 inhibitors | 13 (3.2) | 0 (0.0) | 1 (0.9) | 8 (3.9) |
| Other lipid lowering drugs | 11 (2.8) | 0 (0.0) | 5 (4.5) | 6 (3.0) |
| Single-pill combination for dyslipidemia (n=393) | 136 (34.6) | 5 (20.0) | 29 (25.9) | 83 (40.7) |
| Single-pill combination for dyslipidemia and hypertension | 25 (6.4) | 1 (4.0) | 4 (3.6) | 20 (9.8) |
| Diabetes | ||||
| Treatment for diabetes, n (%) | 0 (0.0) | 60 (92.3) | 89 (92.7) | |
| Therapies, n (%) | ||||
| Metformin | 0 (0.0) | 51 (85.0) | 68 (76.4) | |
| Metformin+DPP4i | 0 (0.0) | 5 (8.3) | 7 (7.9) | |
| Metformin+SGLT2i+GLP-1 RA | 0 (0.0) | 6 (10.0) | 8 (9.0) | |
| Metformin+SGLT2i | 0 (0.0) | 4 (6.7) | 9 (10.1) | |
| SGLT2i | 0 (0.0) | 23 (38.3) | 49 (55.1) | |
| Single-pill combinations | 0 (0.0) | 27 (45.0) | 39 (43.8) | |
ACEIs: angiotensin-converting enzyme (ACE) inhibitors; ARB: angiotensin II receptor blockers; BB: beta blockers; CCB: calcium channel blockers; DIU: diuretics; DPP4i: dipeptidyl peptidase 4 inhibitors; GLP-1RA: glucagon-like peptide 1 receptor agonists; SGLT2: sodium glucose co-transporter type 2 inhibitors.
Among the patients receiving LLT (n=393), 94.9% were receiving statin therapy, with 51.6% of them being treated with high-intensity statins. Statins plus ezetimibe was administered in 21.7% of the patients. Overall, 34.6% of the patients were treated with fixed-dose combination therapy for dyslipidemia management, and only 6.4% were receiving fixed-dose combination therapy for both dyslipidemia and hypertension (Table 2).
The treatment for dyslipidemia and hypertension of the overall study population by healthcare setting/physician specialty are shown in Supplementary Table 2.
Achievement of guideline-recommended risk-based LDL-C goals and BP targetsOverall, 24% of the patients (96/400) had achieved their risk-based LDL-C targets according to the 2021 ESC/EAS guidelines. Of note, 21.8% of the patients (29/133) at high-CV risk and 25.1% (55/219) of those at very high risk had reached the guideline-recommended LDL-C targets (Fig. 1). The LDL-C levels in the overall population and according to CV risk are detailed in Fig. 2.
Globally, 30.3% of the patients (134/433) had achieved the recommended BP targets. Notably, only 27.1% of the patients (36/133) at high risk and 36.1% (79/219) of those at very high risk showed hypertension control. Overall, 8.8% of the patients (38/433) achieved both the LDL-C and BP targets (Fig. 1).
When the achievement of LDL-C goals was analyzed according to CVRFs, we found that 36.8% of the patients with CAD, 42.9% of the patients with diabetes, and 21.3% of the patients with obesity reached the guideline-recommended LDL-C targets. Notably, only 14.8% of the female patients achieved the LDL-C targets (Supplementary Fig. 1). Overall, 45.6% of the patients with CAD, 42.9% of the patients with diabetes, and 26.1% of the patients with obesity attained the recommended BP goals (Supplementary Fig. 1).
The percentage of achievement for the LDL-C targets was 26.7% and 32.5% in the cardiology and internal medicine departments, and 15.9% in the primary care setting. The recommended BP targets were attained in 36.3% and 25.4% of the patients in the cardiology and internal medicine departments, and in 29.8% of the patients in primary care (Supplementary Fig. 2).
Achievement of recommended HbA1c concentrationOverall, 51.4% (74/433) of the patients with concurrent diabetes achieved glycemic control (HbA1c <7%). Only 9.4% of the diabetic patients (15/433) achieved simultaneous control of hypertension, dyslipidemia and diabetes, with 7.8% of the patients at high risk (5/133) and 10.4% of the patients at very high risk (10/219) achieving the LDL-C, BP and HbA1C targets (Fig. 3).
The attainment rate of the HbA1c targets was 39.5% and 57.1% in the cardiology and internal medicine departments, and 54.7% in primary care. Simultaneous achievement of the LDL-C, BP and HbA1c targets was recorded in 8.2% and 15.2% of the patients in the cardiology and internal medicine departments, and in 6.2% of the patients in the primary care setting (Supplementary Fig. 2).
DiscussionThe present study comprehensively evaluated the specific achievement of guideline-recommended LDL-C goals and systolic and diastolic BP targets in real-life hypertensive patients with dyslipidemia, as well as simultaneous control of HbA1c, BP and LDL-C in those patients with concurrent diabetes in Spain.
The study included a real-life cohort of patients with hypertension and dyslipidemia in different healthcare settings where these patients are usually managed under routine clinical practice conditions. Nearly 57% of the patients were at very high-CV risk, as most of the subjects included in the study (almost 60%) were enrolled in cardiology and internal medicine departments/units.
The results obtained indicate poor achievement of the LDL-C goals in patients with concurrent hypertension and dyslipidemia, with 76% of the patients failing to achieve the guideline-recommended LDL-C targets. It is noteworthy that approximately 75% of the patients at very high risk failed to reach their risk-based LDL-C goals, with the consequent increased risk of ASCVD in these individuals.
The suboptimal attainment of LDL-C goals observed in the SNAPSHOT study (24%) is consistent and within the range reported in previous European studies, including those specifically conducted in Spain, which have reported a very low proportion of patients reaching the 2019 ESC/EAS guideline-recommended LDL-C targets22–27 in individuals at high or very high-CV risk (<70mg/dL and <55mg/dL, respectively). Thus, the SANTORINI European observational study found that only 21.2% of the patients at high or very risk of CVD achieved the 2019 LDL-C goals in the primary care and specialized healthcare settings.23 Similarly, findings from a cross-sectional, observational study conducted in primary care, internal medicine, endocrinology and cardiology departments in Spain found that only 22% and 25% of the patients at high and very high-CV risk, respectively, attained the 2019 risk-based LDL-goals (Dyslipidemia Observatory),25 in line with the results from the Spanish cohort of the SNAPSHOT study. A recent retrospective study conducted in patients with acute coronary syndrome (ACS) in Spain has showed that approximately 50% of patients at very high risk did not meet the therapeutic target of LDL-C <55mg/dL.27 Low achievement of the LDL-C goals had been previously reported in several international and Spanish studies using previous guideline targets based on less ambitious control thresholds (i.e., 2016 ESC/EAS guidelines), and which differed depending on the patient CV comorbidity burden or the LLT used for CVD prevention.12,13,28 However, limited evidence is available on the achievement of LDL-C goals recommended in both the 2019 and 2021 ESC/EAS guidelines, which lowered the LDL-C targets in patients at very high risk.22–26 Additionally, to our knowledge, no studies specifically evaluating the achievement of LDL-C targets following the release of the 2021 EAS/ESC guidelines in patients with concurrent hypertension and dyslipidemia are available.
The inadequate LDL-C control seen in our study among the subgroups of patients at very high-CV risk, such as those with diabetes and CAD, is especially worrying. Fewer than 45% of the patients with diabetes reached the recommended targets, though their LDL-C goal achievement rate was higher compared to patients without diabetes (23%). Indeed, a higher attainment rate has been previously reported in patients with diabetes mellitus,29–31 which has been identified as an independent factor associated with the achievement of LDL-C goals.32 A more structured and dedicated follow-up in diabetic patients may be a possible explanation for this finding in the real-world setting, as previously suggested.24,33 Another interesting finding in this study was the higher achievement of LDL-C targets among patients with established CAD (36.8% in patients with CAD versus 18.9% in those without CAD). This finding is in line with the international CEPHEUS study that reported higher LDL-C goal achievement rates among those patients with established CVD/previous acute myocardial infarction.31,34 One potential explanation for this result may be a stricter follow-up and lipid control and an adequate use of LLT in these patients at very high risk. Indeed, the presence of CAD has been identified as an independent determinant for the achievement of LDL-C targets.32 Nevertheless, it is noteworthy that only 36.8% of the hypertensive patients with dyslipidemia and CAD achieved their risk-based LDL-C targets in our series.
Our study also recorded a very low achievement rate of the LDL-C goals among women: only 14.8% reached the recommended targets (31.7% in men). This low proportion of women achieving the LDL-C targets has also been recently reported among patients with ASCVD and/or type 2 diabetes mellitus in an Italian real-world study, which identified the female gender as the only independent factor associated with a significantly lower likelihood of achieving LDL-C target levels for all risk categories.33 A suboptimal attainment rate in women was also reported in the EUROASPIRE V study, with only 23% of the women achieving the recommended LDL-C goals. This can be attributed to the underuse of LLT and high-intensity LLT in women compared to men, evidencing inappropriate treatment of those patients, which may be due to a delay in CV risk evaluation and management.35 This suboptimal use of LLT is highlighted as a main reason causing patients not to achieve the recommended targets in the new consensus on lipid management by the RECCardioclinics (Spanish Society of Cardiology).36 In this regard, the mentioned consensus introduces four treatment algorithms aimed at optimizing dyslipidemia control and achieving target levels. The SANTORINI study also suggested lower attainment rate of LDL-C goals in women due to lower prescription rates of intensive therapies.37 The undertreatment in women for LDL-C lowering according to guidelines recommendation is particularly worrying, with a higher number of women with ASCVD than men38 and a higher risk of mortality after ACS compared to men.39,40 Considering that women remain at high risk of undertreatment regardless of their CV risk category, it is of paramount importance to implement strategies to address suboptimal LDL-C management in this population. These strategies may include implementation of plans to increase physician awareness of the importance of CV risk assessment in women, gender-tailored LLT and patient education aimed at improving health literacy and awareness of the risk for ASCVD events in the absence of adequate LLT.
Although most patients were receiving statin therapy, 37.7% of the very high-risk patients were not receiving high-intensity statins, and 27.1% of the patients were treated with high-intensity statins plus ezetimibe, which has been associated with a greater likelihood of reaching LDL-C targets41; indeed, it has been recommended by the current ESC/EAS guidelines for patients who are not at LDL-C targets despite taking maximally tolerated statin doses.20 The management of CVD prevention is therefore still far from optimal among hypertensive patients with dyslipidemia in the real-world setting. Single-pill combinations enable the intensification of treatment without increasing pill burden or treatment complexity, and their use has been associated with increased patient adherence to LLT and improvement of outcomes in terms of LDL-C goal achievement.42 Nevertheless, we found that only 34.6% of the patients received single-pill combination treatment for dyslipidemia, with a slightly greater use in patients at very high-CV risk (41%). A suboptimal use of single-pill combinations for dyslipidemia and hypertension has also been observed in our study, with only 6.4% of the patients receiving this form of treatment (9.8% in patients at very high-CV risk).
The results of this study also show that hypertension is poorly controlled in real-life patients with both hypertension and dyslipidemia, with only 30.3% of the patients achieving BP targets. Of note, only 27.1% and 36.1% of the patients at high and very high-CVD risk, respectively, had achieved guideline-recommended BP targets. The suboptimal BP control rate is within the range previously reported (30–50%).43 The IBERICAN Spanish prospective study reported an achievement rate of the BP goals of 58.3%.44 However, this study enrolled patients between 2014 and 2018 in the primary care setting; the BP control criteria of the 2013 ESH/ESC guidelines were considered; and the study included about 65.9% of patients with hypercholesterolemia.
The present study has also shown that a notable proportion of patients at very high risk due to concurrent CVRFs are not adequately controlled for hypertension, with 73.9% of the patients with obesity, 57.1% of those with diabetes, and 54.4% of the patients with CAD not achieving BP control under clinical practice conditions. Additionally, we found that BP control was achieved more frequently in patients with diabetes and CAD, in line with the IBERICAN study, which reported a higher control rate in patients with diabetes and CVD compared to non-diabetic patients.44 Our results have shown a very low rate of simultaneous control of LDL-C and BP (less than 8.8%), with also a higher rate of patients with diabetes and CAD achieving control of both risk factors, as evidenced by individual achievement rates. Again, a very low achievement rate was observed among female patients, with only 14.8% achieving the LDL-C targets and 4.1% achieving simultaneous control of both factors, thus stressing the need for management optimization in women.
A low utilization rate of single-pill combination treatment for hypertension has also been found in our study, with only 42.4% of the patients receiving this form of therapy; this may be due to therapeutic inertia with the use of less intensive strategies that may prevent achieving BP targets. Furthermore, while a considerable proportion of patients in this study did not achieve optimal hypertension control, it is important to note that the level of control may be even lower under the new 2024 ESC guidelines for the management of elevated BP and hypertension,45 due to the stricter blood pressure targets involved. The main treatment goal for patients with diabetes is to maintain good glycemic control in order to prevent organ damage and microvascular and macrovascular complications. Nevertheless, we found that 48.6% of patients failed to achieve adequate glycemic control. Additionally, simultaneous attainment of the recommended risk-based LDL-C, BP and HbA1c targets was achieved by only 9.4% of the diabetic patients with hypertension and dyslipidemia. This study therefore highlights that the simultaneous control of hypertension, dyslipidemia and diabetes is suboptimal in real-life patients presenting these major modifiable CVRFs in Spain, with the consequent increased risk of ASCVD and mortality in these patients due to the coexistence of such relevant CVRFs. When one risk factor is poorly controlled there seems to be a greater likelihood that other risk factors are also not controlled.19 The International Cholesterol Management Practice Study (ICLPS) investigated achievement of the ESC/EAS guideline-recommended LDL-C targets in patients receiving LLT (n=2377), and also reported a very low rate of achievement of the LDL-C, HbA1c and BP targets, with only 12% of the patients achieving simultaneous control of all three factors.19 The ICLPS study likewise suggested that the individual control of LDL-C, BP and diabetes is related, and that failure to control one of these risk factors is associated with poor control of the others.
The SNAPSHOT study therefore highlights that achieving the LDL-C targets recommended by the 2019 and 2021 ESC/EAS guidelines remains a challenge in clinical practice. Factors that may contribute to the suboptimal attainment of LDL-C goals include those related to physicians, such as the unawareness or incomplete knowledge of guidelines leading to underestimation of patient's ASCVD risk, misperception of preventive LDL-C control and therapeutic inertia,26,27,46,47 with the consequent underuse of intensive treatment and combination therapy (i.e., statin plus ezetimibe)27; those related to the patient, including reluctance to receive high-intensity statins, LLT non-adherence and discontinuation, mainly due to the risk for adverse effects and pill burden,48,49 and the variability in response among individuals50; and those associated to healthcare system such us regional differences in access to LLT and restricted access to specific therapies, as wells as management of CVRF, including diabetes, hypertension, and dyslipidaemia, in different healthcare settings that may lead to inconsistencies in patient care. Further efforts and implementation of effective strategies are needed to achieve current guideline-recommended LDL-C goals.
Strategies to optimize LDL-C target attainment may include enhancing knowledge on clinical practice guidelines, thereby improving CV risk stratification and enabling tailored treatment strategy according to risk-based LDL-C goals; personalized treatment according to patient characteristics and comorbidity (i.e., impaired renal function, hypertension, diabetes, etc.) and targeted treatment approaches for populations with lower risk of goal attainment based on guidelines recommendations, with intensification of LDL-C lowering therapy for patients at high risk of ASCVD (i.e., concurrent CAD and/or diabetes) including high-intensive statins and combination therapy (i.e., statin plus ezetimibe); multidisciplinary and coordinated management of CVRF (diabetes, hypertension, etc.) between specialties/healthcare settings; encourage healthy lifestyle (i.e., healthy diet, physical activity, smoking cessation); patient education on LLT for the prevention of ASCVD events, treatment simplification with single-pill combinations to improve treatment adherence; implementation of digital health tools to enhance patient engagement and management of CVRF (i.e., diet, physical activity, etc.); shared decision making, with patients and clinicians working as a team to make care decisions; regular follow-up of patients for monitoring LDL-C levels to ensure achievement of treatment goals, make timely treatment adjustments if required, assessment of potential adverse effects (i.e., muscle pain or liver enzyme elevations on statin therapy), and monitoring of patient treatment adherence.
A comprehensive and multifactorial approach to manage all CVRFs should be implemented in patients with concurrent dyslipidemia, hypertension, and any other CVRF including glycemia, obesity, and/or smoking.10 Different specialties are involved in the management of CVRFs; therefore, a coordinated and collaborative approach should be adopted between specialties/healthcare settings as a care continuum to improve the global control of CVRFs. As previously stated, patients should be encouraged to adopt a healthy lifestyle, including balanced and healthy diet, regular physical activity, and smoking cessation.10 Additionally, considering that patients with several CVRFs receive multiple therapies (i.e., statins, antihypertensives, antidiabetics, etc.), simplification of treatment using single-pill combinations may enable improvement of treatment adherence and attainment goals.51
This study has some limitations that must be acknowledged. Firstly, it uses retrospective data collected according to routine daily practice with no purposes other than clinical management; there consequently may be some missing data. Additionally, the cross-sectional design of the study does not allow us to establish cause-and-effect relationships. For instance, suboptimal use of LLTs and combination therapy cannot be directly related with inadequate control of LDL-C levels. Prospective studies are required to assess causality. A further limitation was the unavailability of complete data for CV risk assessment using the SCORE2 and SCORE2-OP algorithms according to the 2021 ESC/EAS guidelines in 55 patients. A longitudinal design may also allow data monitoring to ensure the quality of the collected data, which may also mitigate the inherent limitation of missing data in the context of a retrospective chart review study. Prospective design may also enable homogeneous follow-up. Nevertheless, our study descriptively reports the largest cohort of hypertensive patients with dyslipidemia in whom LDL-C and BP targets have been assessed in Spain, therefore providing a welcome addition to the limited data available on the simultaneous control of dyslipidemia and hypertension as well as diabetes, in routine clinical practice. On the other hand, no studies specifically evaluating the achievement of LDL-C targets following publication/release of the 2021 EAS/ESC guidelines20 in patients with concurrent hypertension and dyslipidemia are available in Spain.
ConclusionsThis study has shown that attainment of the LDL-C and BP goals is still suboptimal in patients with dyslipidemia and hypertension at high and very high risk of CVD in the real-world setting in Spain. Noteworthy, 74.9% of the patients at very high risk fail to reach their LDL-C targets, with the consequent increased risk of ASCVD in these patients. Additionally, the simultaneous control of LDL-C and BP is also very low, with 8.8% of the patients reaching the recommended targets. Likewise, only 9.4% of the patients with concurrent dyslipidemia, diabetes and hypertension achieved simultaneous control of LDL-C, BP and HbA1c, thus highlighting the current challenge of controlling multiple CVRFs that significantly contribute to ASCVD events and mortality. This study also shows that patients with hypertension and dyslipidemia are not adequately treated, with an underuse of high-intensity LLT, combination treatment and single-pill combination therapy for hypertension and for dyslipidemia, and suboptimal optimization of antihypertensive, lipid-lowering, and antidiabetic therapies in these high-risk patients. This study therefore emphasizes the need for more effective management of CVRFs in the real-world setting.
CRediT authorship contribution statementJ.M.M, M.C.B, J.P.J.P have contributed to the study design, data collection, data analysis and interpretation, and manuscript preparation and review. S.S.R, C.V.G, J.C.Y.W, M.C.A, C.E, M.L.F, F.G.T, M.G, M.M.M, and G.P have contributed to study data collection, manuscript preparation and review. All authors read and approved the final version of the manuscript and agree to be personally accountable for the author's contributions and for ensuring that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and documented in the literature.
Informed consentInformed consent was obtained from all subjects involved in the study.
FundingThis study was funded by Servier Laboratories.
Conflict of interestMiguel Chopo has participated in medical meetings sponsored by Bayer, Daiichi Sankyo, Boehringer, AstraZeneca, Alter and Lilly. Carlos Escobar has received honoraria as speaker or advisory from Adamed, Almirall, Amgen, AstraZeneca, Daiichi Sankyo, Menarini, Novartis, Organon, Sanofi, Servier and Viatris. Marta Martín Millán has received honoraria for as speaker in scientific meetings from Daiichi Sankyo and Amgen and is participating in clinical trials from Lilly and Novartis. José María Mostaza, Miquel Camafort Babkowksi, Soraya Sotto Rodriguez, Cristina Vehi Gasol, Juan Carlos Yáñez Wonenburguer, Maria Luisa Fernández Bujia, Fernando Gallo Trébol, Mar Gracia, Guillermo Pinillos and Juan Pedro Justel Pérez have no conflicts of interest to disclose.
The authors would like to acknowledge the SNAPSHOT study investigators (Carmen De la Hoz Regules, Centro de Salud Dr. Morante, Santander, Spain; Silvia Gómez Moreno, Hospital Virgen del Rocío, Sevilla, Spain; Estíbaliz Jarauta Simón, Complejo Hospitalario Miguel Servet, Zaragoza, Spain; Mónica Maure Rico, Centro de Salud Mallen, Sevilla, Spain; José Luis Díaz Díaz, Hospital Universitario de A Coruña, A Coruña, Spain; Daniel Mosquera Lozano, Hospital de San Pedro, Logroño, Spain; David León Jiménez, Hospital Virgen del Rocío, Sevilla, Spain; Nuria López Batet, CAP Comte Borrel, Barcelona, Spain; Nicolás Ortega, Hospital Virgen de la Arrixaca, Murcia, Spain; Javier Rodríguez Calvillo, Centro de Salud Sangonera La Verde, Murcia, Spain; Saribel Lorente Calvo, Hospital Universitario Doctor Peset, Valencia, Spain; Natalia Royuela, Hospital Marqués de Valdecilla, Santander, Spain; Antonio Tello Montoliu, Hospital Virgen de la Arrixaca, Murcia. Spain; Vicente Mora Llavata, Hospital Universitario Doctor Peset, Valencia, Spain; and Melchor Rodríguez Gaspar, Hospital Universitario de Canarias, La Laguna, Spain).
We thank Servier Laboratories for supporting the study. Medical writing and editorial support were provided by Evidenze Health España (Scientific Advisory and Medical Writing Department; Clinical Research Unit).