Solid pseudopapillary tumors (SPT) of the pancreas are rare exocrine neoplasms of the pancreas. Correct preoperative diagnosis is not always feasible. The treatment of choice is surgical excision. These tumors have a good prognosis with a high disease-free survival rate.
ObjectiveTo describe the clinicopathological and radiological characteristics as well as short- and long-term follow-up results of patients who have undergone SPT resection.
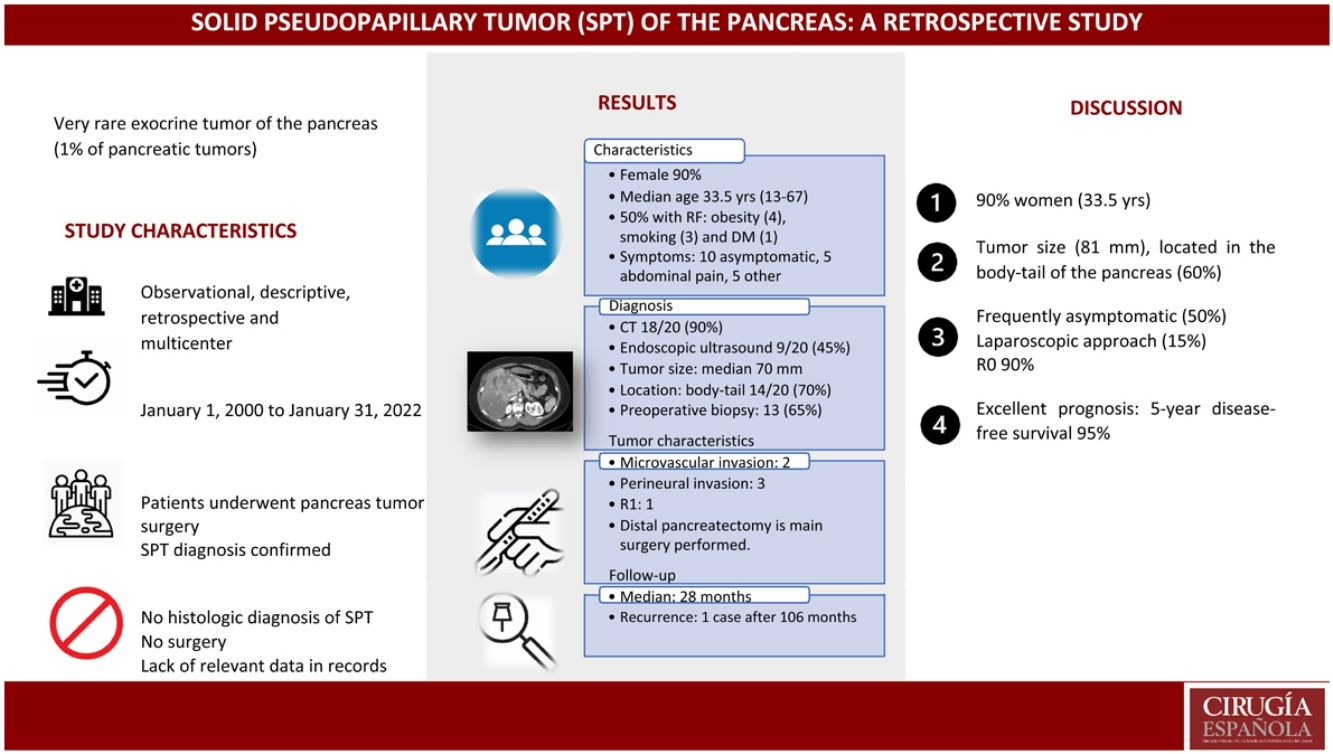
MethodsMulticenter retrospective observational study in patients with SPT who had undergone surgery from January 2000–January 2022. We have studied preoperative, intraoperative, and postoperative variables as well as the follow-up results (mean 28 months).
Results20 patients with histological diagnosis of SPT in the surgical specimen were included. 90% were women; mean age was 33.5 years (13–67); 50% were asymptomatic. CT was the most used diagnostic test (90%). The most frequent location was body-tail (60%). Preoperative biopsy was performed in 13 patients (65%), which was correct in 8 patients. Surgeries performed: 7 distal pancreatectomies, 6 pancreaticoduodenectomies, 4 central pancreatectomies, 2 enucleations, and 1 total pancreatectomy. The R0 rate was 95%. Four patients presented major postoperative complications (Clavien-Dindo > II). Mean tumor size was 81 mm. Only one patient received adjuvant chemotherapy. With a mean follow-up of 28 months, 5-year disease-free survival was 95%.
ConclusionSPT are large, usually located in the body-tail of the pancreas, and more frequent in women. The R0 rate obtained in our series is very high (95%). The oncological results are excellent.
El tumor sólido pseudopapilar de páncreas (TSPP) es una infrecuente neoplasia exocrina de páncreas. El diagnóstico preoperatorio correcto no siempre es factible. El tratamiento de elección consiste en la exéresis quirúrgica. Este tumor presenta buen pronóstico con alta tasa de supervivencia libre de enfermedad.
ObjetivoDescribir las características clínicopatológicas y radiológicas, los resultados de seguimiento a corto y largo plazo de los pacientes a los que se resecó un TSSP.
MetodologíaEstudio observacional retrospectivo multicéntrico de pacientes intervenidos quirúrgicamente de TSPP en enero 2000- enero 2022. Estudiamos variables preoperatorias, intraoperatorias, postoperatorias, y los resultados del seguimiento (mediana 28 meses).
ResultadosSe incluyeron 20 pacientes con diagnóstico histológico de TSSP en la pieza quirúrgica. 90% eran mujeres. Edad (mediana): 33,5 años (13–67). 50% eran asintomáticos. La TC fue la prueba diagnóstica más empleada (90%). La localización más frecuente fue cuerpo-cola (60%). Se efectuó biopsia preoperatoria en 13 pacientes (65%), y fue correcta en 8 pacientes. Cirugías realizadas: 7 pancreatectomías distales, 6 duodenopancreatectomías cefálicas, 4 pancreatectomías centrales, 2 enucleaciones y 1 pancreatectomía total. La tasa R0 fue 95%. Cuatro pacientes presentaron complicaciones postoperatorias mayores (Clavien-Dindo > II). El tamaño tumoral fue 81 mm. Sólo un paciente recibió quimioterapia adyuvante. Con una mediana de seguimiento de 28 meses, la supervivencia libre de enfermedad a 5 años fue del 95%.
ConclusiónLos TSSP son de gran tamaño, localizados habitualmente en cuerpo-cola pancreática, y más frecuentes en mujeres. La tasa R0 obtenida de nuestra serie es muy elevada (95%). Los resultados oncológicos son excelentes.
Solid pseudopapillary tumors of the pancreas (SPT), also called Frantz tumors, are very rare exocrine tumors of the pancreas that represent approximately 1%–2% of all pancreatic tumors. First described by Frantz in 1959,1 the etiology and pathophysiology of SPT have not yet been fully clarified. They are usually diagnosed in young women (second and third decades of life),1,2 with a prevalence of 9.7:1 (female:male), probably due to the relationship of SPT with estrogens and progesterone.3,4
SPT present as large lesions (8−10 cm in diameter),1 usually located in the tail of the pancreas, and are characterized by being solitary, well-circumscribed tumors that combine solid and cystic areas.2 Although a correlation between tumor size and the risk of malignancy had initially been suggested,3 this has not been confirmed.3,5 Symptoms are very variable, from practically asymptomatic presentations to patients who experience symptoms secondary to the compression of adjacent organs or structures (abdominal pain, jaundice, palpable mass, etc).2,6
The diagnosis of SPT is usually made through a combination of diagnostic tests, including ultrasound, computed tomography (CT), magnetic resonance imaging (MRI) and endoscopic ultrasound, which facilitates fine needle aspiration (FNA) biopsy.4,7 There is no consensus on which radiological characteristics of SPT suggest malignancy, but dilation of the pancreatic duct, vascular invasion, extensive necrosis and/or an incomplete capsule are the most frequent findings in malignant tumors.6,8,9 SPT has a wide variety of immunohistochemical expression, since its origin is probably multipotential primitive cellular. Non-specific markers such as B-catenin (100%), vimentin (98%), CD 99 (98%) and CD 10 (93%) have been associated; however, there are no specific markers, and no association with prognosis has been found.10
It is common for the preoperative diagnosis to be incorrect, and patients are often diagnosed with pancreatic adenocarcinoma; subsequently, it is the histological study of the surgical specimen that confirms the diagnosis of SPT.9,11
The treatment of choice for SPT is surgery, using different techniques depending on the tumor location (enucleation, distal pancreatectomy [DP], pancreaticoduodenectomy [PD], central pancreatectomy [CP] and total pancreatectomy [TP]).2 The laparoscopic approach is feasible and safe, without higher rates of tumor recurrence, and it is not inferior to laparotomy.11–13 However, since the lesions are large, it is not the approach usually used. In unresectable tumors, neoadjuvant treatment with chemotherapy and radiotherapy is used to attempt subsequent rescue surgery.14
The prognosis of SPT is usually good, with a 5-year survival rate of 90% and a local recurrence rate of less than 10%.6 Prognostic factors described in the literature include: histological tumor characteristics (presence of vascular and/or perineural invasion), extrapancreatic disease, and R0 surgery with free margins.1,15
There is little published information on SPT. Nationally, the few publications in the literature are based on individual cases, so it is difficult to draw conclusions. Likewise, other European publications do not report a large number of cases. The 2 international studies published with the largest numbers of patients were carried out by an Asian group16 and a Turkish group5 (53 and 24 patients, respectively).
The objective of our study is to present the cases of SPT operated on in the Valencian Community in order to determine the preoperative characteristics, diagnostic and therapeutic strategies, and prognostic factors for SPT.
MethodsWe have designed an observational, descriptive, retrospective, multicenter study, which was conducted at both public and private hospitals in the Valencian Community (region of Spain). The study was approved by the Research Ethics Committee of the Health Department of the Dr. Balmis General University Hospital.
Inclusion criteriaThis study included all patients who underwent surgery and had a final histopathological diagnosis of SPT from January 1, 2000 to January 31, 2022. The pathological study showed the presence of solid areas alternating with pseudopapillary areas. Immunohistochemical analyses were performed to confirm the diagnosis in all cases.
Exclusion criteriaPatients were excluded when their diagnosis was not confirmed by histopathological study. All patients who did not undergo surgery and those with incomplete medical histories were also excluded.
Study variablesThe hospitals that participated in the study received an anonymized database, which included data forms to register data extracted from patient healthcare records. The variables studied were:
- o
Epidemiological: sex, risk factors (smoking, diabetes mellitus, alcoholism, obesity and family history of pancreatic cancer), and symptoms (abdominal pain, palpable abdominal mass, nausea/vomiting, weight loss, jaundice or pancreatitis)
- o
Diagnostic: tests performed, and results obtained (abdominal CT, abdominal ultrasound, endoscopic ultrasound, magnetic resonance imaging and preoperative biopsy)
- o
Surgical: type of approach (laparoscopy vs laparotomy), type of intervention (DP, PD, CP, TP and enucleation), performance of vascular resection and/or other organs.
- o
Postoperative and immediate follow-up: all complications collected during the first 90 days were registered. Postoperative complications were classified using the Clavien-Dindo scale.17 We used the ISGPS15 classification to evaluate pancreatic fistula and biliary fistula, delayed gastric emptying, and postoperative hemorrhage.
- o
Histological: tumor size was measured, and all immunohistochemical markers were collected (beta-catenin, progesterone receptor, vimentin, CD10, CD56, CD99, AE1/AE3, CKIT, Rec, lysozyme, synaptophysin, cytokeratin, CAM 5.2, enolase, and alpha-trypsin).10,18
- o
Survival: data were collected for both total survival and local or systemic recurrence when present, understood as the appearance of SPT on the imaging tests performed during follow-up and its confirmation by histopathological examination. Data were also collected on any adjuvant therapies administered.
- o
We also describe our data together with the series published in the literature, without establishing any type of statistical analysis.
Statistical analysisThe statistical analysis was performed with the SPSS v25® program.
Quantitative variables are expressed as medians and interquartile range, and the qualitative variables as percentages and frequencies.
ResultsOut of the 25 hospitals contacted, we received responses from 14, only 9 of which had treated patients surgically for SPT. Twenty patients met the inclusion criteria.
Patient characteristics90% of the patients were women, and their mean age at presentation was 33.5 years (range: 13–67 years). In terms of risk factors, 50% presented no risk factors. Among those who did, the most frequent were obesity (4 patients), smoking (3 patients) and diabetes mellitus (one patient). As for symptoms, 10 patients were asymptomatic, while those who presented symptoms most frequently reported abdominal pain (5 patients), followed by palpable mass and weight loss.
Diagnostic tests and tumor locationThe most commonly used radiological technique was CT, which was performed in 90% (18/20 patients), followed by abdominal ultrasound in 80% (16/20) and MRI in 70% (14/20). Endoscopic ultrasound was the least performed study, at 45% (9/20). The radiological tumor size was 70 mm (mean), and its most frequent location was the body/tail of the pancreas (70%; 14/20). In the remaining patients, 30% (6/20) of tumors were located in the head of the pancreas.
Preoperative biopsy was performed in 13 patients, in 10/13 (77%) by endoscopic ultrasound and 3/13 (23%) by interventional radiology. However, the test was only diagnostic in eight cases (62% of those biopsied).
Characteristics of the surgical interventionThe interventions performed were: 8 DP (7/8 with splenic preservation), 6 PD, 3 CP, 2 enucleations, and one TP. Three of the DP were performed by laparoscopy.
Three of the patients who underwent DP (37%) presented complications within the first 90 days: one patient with Clavien-Dindo I complication, and the other 2 with Clavien-Dindo II. Three of the patients who underwent PD (50%) presented complications: 2 with Clavien-Dindo II complications, and one with Clavien-Dindo III. Two of the patients who underwent CP (67%) presented complications, both of which were with Clavien Dindo III complications. All patients who underwent enucleation presented complications (100%): one presented a Clavien Dindo II complication, and the other Clavien-Dindo III. Also, the only patient who underwent TP (100%) presented a grade I complication.
Eight patients presented pancreatic fistula, 7 of which had a biochemical fistula, type A (3 DP, 2 PD, and 2 enucleations); and one patient presented a type B pancreatic fistula (central pancreatectomy). Delayed gastric emptying was described in 3 patients, all of whom had undergone PD. No patients presented biliary fistula or postoperative bleeding.
In the pathological study, mean tumor size was 81 mm. Two patients had microscopic vascular invasion, and 3 demonstrated perineural invasion. In the clinical records, lymph nodes were only resected in 11/20 cases, and none presented neoplastic infiltration. Surgical margin involvement was observed microscopically in only one patient (R1), who had undergone DP; however, he did not present recurrence. The most frequently altered immunohistochemical markers were beta-catenin and vimentin (11 patients [55%]), and the remaining markers analyzed were less frequently affected (Table 1).
Immunohistochemical tumor characteristics.
| Immunohistochemistry | Total n (%) |
|---|---|
| B-catenin | 11 (55) |
| Vimentin | 11 (55) |
| CD 10 | 10 (50) |
| Progesterone receptor | 9 (45) |
| CD 99 | 1 (5) |
| AE1/AE3 | 3 (15) |
| cKit | 1 (5) |
| Rec | 1 (5) |
| Lysozyme | 1 (5) |
| Synaptophysin | 6 (30) |
| Cytokeratin | 1 (5) |
| Cam 5.2 | 2 (10) |
| Enolase | 4 (20) |
| Alpha-trypsin | 3 (15) |
None of the patients received neoadjuvant treatment. After the histological findings, only one patient received adjuvant therapy with FOLFIRINOX due to sarcomatous characteristics. Mean follow-up after surgery was 28 months (2–141 months). Only one patient presented tumor recurrence 106 months after DP surgery, after having initially been R0.
Since there was no mortality associated with the tumor, we have not been able to carry out advanced statistical studies (univariate and multivariate analyses) that would allow us to identify negative prognostic factors in SPT.
DiscussionWe present a multicenter series with the largest number of patients treated surgically for SPT in Spain to date. With the participation of 9 medical centers in the Valencian Community, we have managed to collect data on 20 patients who had undergone surgery for SPT. 90% of the patients were young women (mean 33.5 years), with a large tumor (81 mm) located in the body/tail of the pancreas (60%). Correct preoperative diagnosis of SPT was only made in 61.5% of all patients who had had a biopsy; the remaining cases were diagnosed by the postoperative histopathological study. Frequently asymptomatic (50%), abdominal pain was the most common symptom among symptomatic patients. The laparoscopic approach was performed in a small percentage of patients (15%). The R0 resection rate was high (95%). Prognosis was excellent, with a 5-year disease-free survival rate of 95%. In the absence of deaths, we were not able to perform univariate and multivariate analyses to determine negative prognostic factors.
A review of the literature reveals that the published series are retrospective, descriptive and single-center. Although the inclusion periods of the studies reviewed are long (6–20 years), the number of cases collected is small; the largest series includes 53 patients.16 The data offered by the 6 series described in the literature tell us that 79.2%–100% of patients operated on for SPT are female, and their age at diagnosis ranges from 25 to 47 years. The vast majority of patients are either asymptomatic or only present with abdominal pain. The most common tumor location in these series is the body/tail (approximately 60%), with an average size ranging from 48–72 mm. Only one patient was reported to have liver metastases in the aforementioned series. The mortality described in all is extremely low (Table 2).3,5,16,18–20
Comparison with other SPT series: see attached document.
| Author Year Country | Type Years of study | n | Females | Age (years) | Tumor sizes (mm) | Location | Vascular invasion | Metastasis | Type of surgery | Postoperative complications | Follow-up time | Mortality due to SPT |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cavallini et al 2011 Italy 18 | Retrospective 8 years | 10 | 80% | 25,4 | 43,8 | Tail 100% | No | No | DP 100% | Bleeding 2/10 PF grade A 1/10 Infections 1/10 | 47 months | 0 |
| Ren et al 2014 China 21 | Retrospective 6 year | 19 | 89% | 28 | 63 | Body and Tail 64% Head 31% Neck 5% | No | No | DP 64% PD 21% | PF 3/19 | 38,4 months | 0% |
| Song H et al 2017 China 17 | Retrospective 13 years | 53 | 87% | 35,4 | 64 | Head 28,3% Body and Tail 60,4% Neck 9,4% | 4/53 | No | DP 53% PD 28% Enucleation 19% | PF 9/53 Intraabdominal abscess 4/53 Gastric fistula 1/53 | 48 months | 3,80% |
| Fahrat et al 2020 Tunisia 20 | Retrospective 18 years | 10 | 80% | 41,2 | 72 | Tail 50% Head 20% Body and Tail 20% Entire pancreas 10% | 1/10 | 1 liver metastasis | DP + Splenectomy 40% PD 20% PD 10% DP 10% Enucleation 10% Unresectable 10% | Bleeding 1/10 PF grade A 1/10 | 118 months | 10% |
| Uguz et al 2020 Turkey 5 | Retrospective 13 years | 24 | 79,20% | 47,2 | 58 | Tail 45,8% Head 37,5% Body 16,7% | 1/24 | NR | DP NR Others | Clavien Dindo I 5/24 Clavien Dindo III 1/24 | 60 months | 8,50% |
| Silano et al 2021 Brazil 3 | Retrospective 20 years | 14 | 100% | 31,5 | 67,2 | Body and Tail 57,1% Head 42,8% | 2/14 | No | DP 57,2% PD 42,8% | PF grade C 2PF grade B 1 | 56,6 months | 0% |
| Duque et al 2022Spain | Retrospective 22 years | 20 | 90% | 33,5 | 70 | Body and Tail (60%) Head (40%) | No | 1 | DP 35% PD 30% CP 15% Enucleation 10% DP + Splenectomy 5% TP 5% | Clavien Dindo I 2 Clavien Dindo II 5 Clavien Dindo IIA 4 PF grade A 7PF gradeB 1 | 28 months | 0% |
PF: Pancreatic fistula, PD: Pancreaticoduodenectomy, NR: Not reported, CP: Central pancreatectomy, DP: Distal pancreatectomy, TP: Total pancreatectomy.
Although few series have been published about SPT, they all agree that the use of MRI improves the preoperative diagnosis, as the SPT are observed as well-circumscribed lesions with areas of soft tissue and necrotic foci, with a thickened capsule that captures the contrast material. Furthermore, up to 30% may present peripheral calcifications.4,8 These data are not pathognomonic of SPT, but they can help us distinguish it from pancreatic adenocarcinoma. In addition to MRI, the latest articles support the use of endoscopic ultrasound in the preoperative diagnosis of pancreatic lesions, since it provides the advantage of being able to perform FNA.9
In our series, 70% of the patients were studied by MRI, but we have observed an increase in its use in recent years. Likewise, the percentages of endoscopic ultrasound have also increased in our series (45% of patients), even though this technique was not available at all the medical centers participating in the study.
Surgical resection of SPT is the only potentially curative treatment, and the surgical technique varies depending on the location of the tumor. The approach performed (laparotomy, laparoscopy, or robotic) will depend on the technical capabilities at each center, yet all are feasible and safe.11 In our series, only 15% were performed by laparoscopy. We believe this is due to 2 factors: first, the series covers a long period of time; and second, the large size of the tumors that makes minimally invasive approaches difficult.3,4 SPT enucleation is a controversial technique due to the risk of recurrence and its difficulty in large tumors.14 In our series, 2 patients were treated by enucleation with no evidence of recurrence after 28 and 23 months of follow-up.
Unlike pancreatic adenocarcinoma, the presence of extrapancreatic metastases is not considered an absolute contraindication for the excision of SPT; if feasible, it and the metastases will be resected, since this strategy is associated with increased survival and better quality of life.3,8,15,20 Liver transplantation has been considered in the case of multiple bilobar liver metastases if the primary tumor has been resected and there are no more metastases in other organs, due to the excellent prognosis of these tumors.14
While its use is uncommon, neoadjuvant chemotherapy can be initiated in SPT that are considered unresectable at diagnosis in order to attempt subsequent rescue surgery.2 Postoperative adjuvant therapy may contribute to an increase in disease-free time and survival in patients with metastatic disease.2,4 In our series, only one patient received adjuvant chemotherapy and remains disease-free after 25 months of follow-up. Radiotherapy has been used in surgically resected patients and unresected patients as a palliative treatment, but its role in the treatment of SPT is not well defined.4,21 A follow-up period of more than 48 months is recommended, since most recurrences appear during this period.2 In our series, with a median follow-up of 28 months, we have detected a single recurrence 106 months after surgery, and no patient died during the follow-up period.
The limitations of this study are its retrospective and multicenter nature, as the study centers do not use the same diagnostic and therapeutic algorithms. Furthermore, it commits an important selection bias by including only those patients who had undergone surgical resection; therefore, it was not possible to determine the characteristics and evolution of patients diagnosed with SPT who did not undergo surgery. The strength of this study is that it is a national series with the highest number of cases to date.
In conclusion, our series has confirmed that SPT is a rare, large, solitary pancreatic tumor that is much more common in young women and is associated with an excellent prognosis when it is completely removed, with free margins, in the absence of metastatic disease. Thus, the treatment of choice is surgical resection, even in patients who present metastatic dissemination, as it improves prognosis and quality of life. The low prevalence makes it difficult to propose prospective studies that allow us to better understand the prognostic factors of SPT.
Ethical considerationsThis study was carried out following the requirements expressed in the Declaration of Helsinki (Seoul revision, October 2008), the good clinical practice guidelines of the ICH (International Conference for Harmonisation), and current legislation in Spain according to the provisions of Ministerial Order SAS/3470/2009 regarding the conduct of observational studies. The highest levels of professional conduct and confidentiality were always maintained, complying with article 7 of Organic Law 15/1999, of December 13 regarding the protection of personal data.
Approval was requested from the Ethics Committee of the General University Hospital of Alicante (CEIm). The database will be registered anonymously, including no identifying patient data, which will be stored under the responsibility of each of the participating centers.
Conflict of interestThe authors of this study have no conflicts of interests to declare, nor have they received any funding for this study.