In esophagogastric surgery, the appearance of an anastomotic leak is the most feared complication. Early diagnosis is important for optimal management and successful resolution. For this reason, different studies have investigated the value of the use of markers to predict possible postoperative complications. Because of this, research and the creation of predictive models that identify patients at high risk of developing complications are mandatory in order to obtain an early diagnosis.
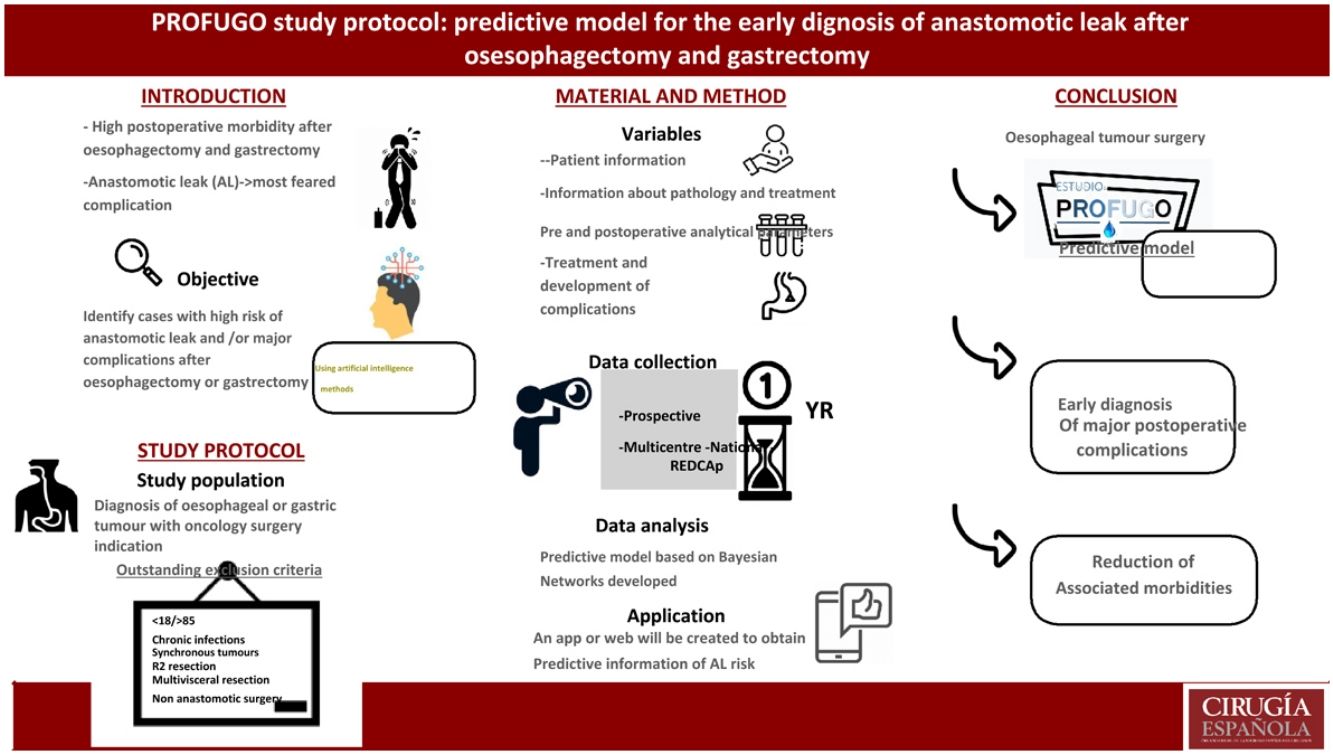
The PROFUGO study (PRedictivO Model for Early Diagnosis of anastomotic LEAK after esophagectomy and gastrectomy) is proposed as a prospective and multicenter national study that aims to develop, with the help of artificial intelligence methods, a predictive model that allows for the identification of high-risk cases. of anastomotic leakage and/or major complications by analyzing different clinical and analytical variables collected during the postoperative period of patients undergoing esophagectomy or gastrectomy.
En cirugía esofagogástrica, la aparición de una fuga de la anastomosis es la complicación más temida. Realizar un diagnóstico temprano es importante para un manejo óptimo y resolución exitosa. Por ello, diferentes estudios han investigado el valor del uso de marcadores para predecir posibles complicaciones postoperatorias. Debido a esto, se hace mandatoria la investigación y creación de modelos predictivos que identifiquen pacientes con riesgo elevado de padecer complicaciones con el fin de obtener un diagnóstico precoz.
El estudio PROFUGO (Modelo PRedictivO para el Diagnóstico Precoz de la FUGa anastomótica tras esofaguectomía y gastrectomía) se plantea como un estudio prospectivo y multicéntrico nacional que pretende elaborar, con ayuda de métodos de inteligencia artificial, un modelo predictivo que permita identificar casos con elevado riesgo de fuga anastomótica y/o complicaciones mayores mediante el análisis de diferentes variables clínicas y analíticas recogidas durante el postoperatorio de pacientes sometidos a esofaguectomía o gastrectomía.
Oesophagogastric cancer is one of the main causes of death from cancer worldwide, with surgery being the basic pillar of curative therapy. However, the postoperative morbidity associated with surgery is high, with anastomotic leak (AL) being one of the most feared complications, with a variable incidence and mortality, depending on the series.1–3 This complication is not only associated with a longer hospital stay and increased costs, but also with a poorer prognosis for the disease and the patient's quality of life.4
AL diagnosis, together with other complications, is frequently made when the patient is symptomatic, which requires immediate and perhaps more aggressive intervention than would occur with an earlier diagnosis. Thus, early diagnosis of AL through clinical symptoms, analytical data, radiology and/or endoscopy is essential to provide optimal and immediate treatment through antibiotic therapy, feeding tube placement, application of endoscopic therapies, percutaneous drainage of collections, etc. possibly reducing the rate of surgical re-interventions. For all these reasons, early prediction, diagnosis and treatment of possible major complications (Clavien-Dindo greater than 3), especially AL, are essential to improve the disease results and prognosis.
Different studies have investigated the usefulness of both pre- and postoperative markers, to predict possible postoperative complications, and some of them have evaluated different markers as predictors of AL and other major complications in the early postoperative stages.4–7
As a result, due to the importance of early diagnosis and management of possible complications after oesophagogastric surgery, research and the creation of predictive models to identify patients with a high risk of suffering from complications are mandatory. With these markers action may be taken, thus avoiding further deterioration of the patient and a possible septic situation in more advanced states. With this purpose in mind, this study has been designed to create a predictive model that can identify patients with a high risk of anastomotic leak and/or major complications after oesophagogastric tumour resection surgery, through the analysis of different clinical and analytical variables collected in the postoperative period.
MethodsStudy design and main objectiveA prospective, multicentre study will be conducted at the national level (1 year in each centre with consecutive inclusion of patients). Its purpose, with the help of artificial intelligence methods, will be to develop a predictive model to identify cases with a high risk of anastomotic leak and/or major complications through the analysis of different clinical and analytical variables collected during the postoperative period of patients undergoing oesophagectomy or gastrectomy.
Secondary objectivesIn addition to the main objective described above, the following secondary objectives are established:
- -
Describe the postoperative evolution of the clinical and analytical parameters studied.
- -
Describe the prevalence of the different complications and types of diagnosed AL.
- -
Record the day on which AL is diagnosed, the treatment used for its possible resolution, and its relationship with hospital stay.
- -
Evaluate the AL resolution capacity of each technique used.
The study population will include patients diagnosed with oesophageal or gastric tumours indicated for oncology surgery with curative intent in any of the participating centres.
Exclusion criteria are patients:
- -
Under 18 or over 85 years of age
- -
Chronic infections
- -
Synchronous tumours in other sites
- -
Autoimmune pathology
- -
Deaths during surgery
- -
Non-signing or revoking of informed consent for study participation
- -
Clinical stage IVB
- -
R2 surgical resection (there are macroscopic remains of the tumour in the surgical field after performing the resection of the surgical specimen)
- -
Combined intraoperative resection of other organs (multivisceral resections)
- -
Surgeries without anastomosis
The purpose of the study is to recruit the largest possible number of patients from all national centres who wish to participate. For an alpha error of 5% (95% confidence) with a precision of 3% and estimating a number of patients with major complications (including AL) of around 30%, the sample size calculation yields a total of 847 patients. However, the final sample size may be smaller depending on the proportion of complications detected, in which case the statistical and artificial intelligence models will be adapted to create the predictive model based on the event rate provided by the recruited sample.
Recruitment and interventionPatients who meet all the inclusion criteria and none of the exclusion criteria will receive detailed information and, if they decide to participate in the study, they will sign the informed consent form (Annex 1, Supplementary data).
The patient will undergo the indicated surgical intervention with curative intent with or without prior neo-adjuvant treatment. The surgical intervention and postoperative care will be carried out in each of the collaborating centres according to their usual clinical practice.
Study variables and timetableThe variables to be included in the study refer to the following aspects and are described in Appendix 2 (Supplementary data):
- -
General data on the characteristics of the patients, tumours and surgical intervention performed on each of them
- -
Pre- and postoperative clinical and analytical parameter data
- -
Data on results and possible complications.
- -
Data on the treatment and evolution of possible complications if they have occurred
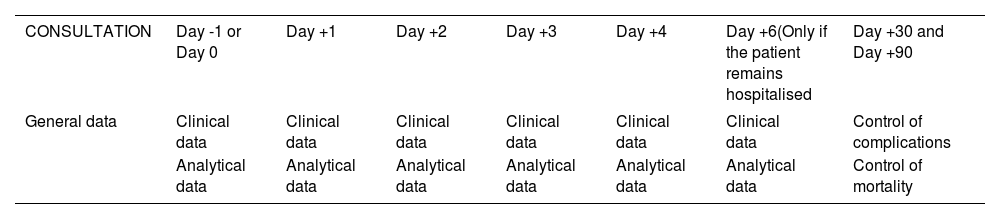
The moments for collecting the different variables appear reflected in Table 1 and are summarised as follows:
- -
Analysis and control of preoperative clinical variables: they must be carried out the day before or on the same day of the surgical intervention prior to it.
- -
During the immediate postoperative period, patients must be evaluated daily and clinical and analytical variables must be collected during days 1, 2, 3, 4 and 6 of the postoperative period. Likewise, in this postoperative course, possible complications that may arise will be collected, following up in the outpatient clinics at 30 and 90 days (last control included in the protocol of this study).
Outline of temporary protocol for collection of variables included in the study.
| CONSULTATION | Day -1 or Day 0 | Day +1 | Day +2 | Day +3 | Day +4 | Day +6(Only if the patient remains hospitalised | Day +30 and Day +90 |
|---|---|---|---|---|---|---|---|
| General data | Clinical data | Clinical data | Clinical data | Clinical data | Clinical data | Clinical data | Control of complications |
| Analytical data | Analytical data | Analytical data | Analytical data | Analytical data | Analytical data | Control of mortality |
Day -1: Day before surgery, Day 0: Day of intervention (assessment prior to the intervention), Day +1: 1st postoperative day, Day +2: 2nd postoperative day, Day +3: 3rd postoperative day, Day +4: 4th postoperative day, Day +6: 6th postoperative day, Day +30: 30th postoperative day, Day +90: 90ºth postoperative day.
Data collection will be carried out prospectively in each of the 47 participating centres, having designed a platform for this purpose within the REDCap of the Spanish Association of Surgeons (AEC for its initials in Spanish). Access to said database will be carried out by assigning secret pin numbers, with each centre having a specialist doctor who will be responsible for updating it.
Data analysisThe study of data and development of predictive mathematical models will be carried out by members of the Intelligent Data Analysis Laboratory of the Department of Electronic Engineering of the Higher Technical School of Engineering of the University of Valencia. The most current versions of open source programming languages and environments such as R and python will be used for this purpose.
Firstly, after an analysis of data quality, a descriptive analysis will be performed with both sociodemographic and clinical variables, together with the analytical variables and study results.
To describe normal distribution quantitative variables, the mean and standard deviation will be used, and to describe those that do not follow a normal distribution the median and interquartile range will be used, together with histograms with normality curves for their graphic description.
For qualitative variables, frequencies and percentages will be used, using bar and/or sector graphs for the graphic description of those with greater relevance.
A univariate study will be performed to relate the variables studied with the appearance of AL and major postoperative complications.
In the results obtained from the univariate study, those variables that show a p < .1 after the application of the corresponding tests will be considered as related or candidates for predicting AL or major complications. This value will be considered more conservative, differing from the conventionally accepted value of .05, with the intention of not ruling out potential variables that could have a certain influence on the study results.
Once the univariate study is completed, a multivariate study will be carried out, using the logistic regression (RL) method.
Furthermore, a predictive model based on Bayesian Networks will also be developed. Specifically, classification structures of the FAN (forest augmented network naïve Bayes) type will be used to facilitate comparison with the classic RL approach while maintaining the interpretability of the mathematical model.
Furthermore, once the model is designed, an application will be created for mobile devices and/or a website where new data on developing cases can be prospectively introduced. As a result, predictive information will be obtained on the possibility of developing AL or major postoperative complication in each particular case, thus helping the clinician to made decisions during the postoperative control of these patients.
Ethical and legal aspectsThe data will be collected in keeping with current regulations on confidentiality and data protection, guaranteeing their protection according to Regulation (EU) No. 2016/679 of the European Parliament and the Council of April 27, 2016 on Data Protection (RGPD).
This study will be conducted following current regulatory requirements, respecting the codes and standards of good clinical practice and guaranteeing the rights of patients, as well as the basic ethical principles (Declaration of Helsinki approved by the World Medical Assembly in its Fortaleza version in 2013), and the Oviedo Convention of 1997).
The study has been registered in Clinical Trials with registration number NCT05390684 and approval will be obtained from the Research and Ethics Committee (CEIC) of all participating centres before the inclusion of the cases in the study.
Study dissemination and results publicationThe protocol will be disseminated through the Spanish Association of Surgeons.
Once the data collection is completed, the project collaborators may propose the development of different sub-studies.
The data will be communicated at different scientific symposiums and published in peer-reviewed journals, in the hope that the study results may help improve care for patients with this type of pathology, making applied treatments safer.
DiscussionSurgery with curative intent for oesophagogastric cancer is burdened with a non-negligible morbidity. Being able to detect serious complications early during the postoperative period is essential to reduce surgical mortality, and therefore the creation of a predictive tool for this morbidity is mandatory to increase the safety of these procedures.
Anastomotic leak is one of the most feared complications in the postoperative period of these surgeries, since it is associated with high mortality and poorer long-term survival. The existing variability in the rate of AL in the literature is due to the lack of a precise definition generally accepted by all groups, as well as the need to establish a reliable and unanimous diagnostic method. In addition to possible technical failures, there are many potential risk factors that may be related to the appearance of this complication.
Many analytical parameters have been studied in an attempt to identify or predict early anastomotic fistula or a major postoperative complication. C-reactive protein (CRP) is one of the most studied inflammatory markers in this regard. CRP levels increase after surgery and commonly peak after 48 h,8,9 subsequently decreasing in patients with an uncomplicated postoperative course. CRP is primarily valuable as a negative test, and a normal or declining CRP level on the third and fifth postoperative days (POD) can help predict which patients are unlikely to develop AL.10
Liesenfeld et al.11 observed a less marked decrease in white blood cell (WBC) count after the second POD in patients with AL. It was also observed that CRP is an accurate negative predictive marker, obtaining the best diagnostic accuracy in the fourth POD, with a cut-off value of 145 mg/l.
Serum albumin has also been used as a nutritional marker to predict postoperative complications in certain gastrointestinal surgeries. In 2011, Noble and Underwood12 developed the NUn score calculated from the individual values of CRP, WBC and albumin in the fourth POD in patients undergoing oesophagogastric resection.13
In other studies, it has been shown that peritoneal levels of IL-6 and TNFα were significantly higher in patients with colorectal anastomosis leak, which may contribute to its early detection, and it has been confirmed that the increase in serum levels of IL-6 is a predictor of AL in gastrointestinal surgery.14
In a retrospective study carried out by Yansen et al.,15 the neutrophil-lymphocyte ratio (NLR) was used as a biochemical marker, concluding that the NLR value is more relevant in its negative predictive values and facilitates more assured postoperative decisions. In contrast, a rising rate of NLR between the first and third POD is an independent factor of AL that should raise suspicion for it.
Another study conducted by Sugimoto et al.7 analysed preoperative inflammatory and nutritional markers and studied their relationship with the appearance of postoperative AL in oesophageal cancer. The study compared the predictive ability of CAR, prognostic nutritional index (PNI) and preoperative mGPS for AL, and identified that a high value of preoperative CAR (≥.0139) but not PNI or mGPS, is a useful indicator for predict the appearance of AF after oesophagectomy.
Thus, the evidence on the usefulness of different markers to early predict AL and/or major complications after oesophagogastric resection surgery is still limited and quality prospective studies with adequate sample sizes are required to draw more accurate conclusions. We therefore propose to conduct this multicentre study which, despite its prospective design, may present certain limitations, among which the following stand out:
- -
Possible existence of confounding variables that have not been foreseen in the study approach.
- -
Possible limitations in information collection.
- -
The low incidence of the pathology studied in our environment, which requires a long period of time to achieve an optimal sample size.
- -
The existence of differences in the surgical technique and perioperative management protocols specific to each centre.
In conclusion, the PROFUGO study is proposed as a project of high scientific interest that seeks to respond to the problem of early diagnosis of major postoperative complications in patients undergoing surgery with curative intent for oesophagogastric cancer, attempting to thereby increase the safety of these procedures.
Conflict of interestsNone.
FundingNone.
Cristina Alegre Torrado: Hospital Universitario 12 de Octubre
Silvia Carbonell Morote: Hospital General Universitario de Alicante
Carlos Díaz Lara: Hospital General Universitario de Elche
Jennifer Triguero Cabrera: Hospital Universitario Virgen de las Nieves Granada
Elisenda Garsot Savall’s: Hospital Universitario Germans Trias i Pujol
Jean Carlos Trujillo Díaz: Hospital de Medina del Campo
Fernando Lopez Mozos: Hospital Clínico Universitario de Valencia
Rocío González López: Hospital Universitario Lucus Augusti de Lugo
Monica Rey Riveiro: Hospital del Vinalopó
Elizabeth Redondo Villahoz: Hospital Clínico Universitario de Valladolid
Laura Jimenez Álvarez: Hospital Universitario Príncipe de Asturias
Marta de Vega Irañeta: Hospital Universitario de Fuenlabrada
Adrian Herrero Fabregat: Hospital San Pedro (Logroño)
Claudia Mulas Fernández: Consorcio Hospital General Universitario de Valencia
María Asunción Acosta Mérida: Hospital Universitario de Gran Canaria Doctor Negrín
Elena Fernández Elvira: Hospital General Universitario de Ciudad Real
María del Campo Lavilla: Hospital Santa Bárbara
Felipe Parreño Manchado: Hospital Clínico Universitario de Salamanca
Cristina Sancho Moya: Hospital Arnau de Vilanova (Valencia)
Rodolfo Rodriguez Carrillo: Hospital de Sagunto (Valencia)
Amparo Roig Bataller: Hospital Lluis Alcanyis De Játiva (Valencia)
Erick Montilla Navarro: Hospital de Denia (Alicante)
María García Nebreda: Hospital Universitario Infanta Leonor (Madrid)
Teresa Carrascosa Mirón: Hospital Universitario de Getafe
Rafael López Pardo: Hospital Universitario de Toledo
Diego Antonio Bernal Moreno: Hospital Universitario Puerto Real (Cádiz)
Helena Salvador Rosés: Hospital Universitario Arnau de Vilanova (Lleida)
Ander Bengoechea Trujillo: Hospital Universitario Puerta del Mar (Cádiz)
Irene Álvarez Abad: Hospital Universitario de Cruces
Maria Tudela Lerma: Hospital General Universitario Gregorio Marañón (Madrid)
Luis Munuera Romero: Hospital Universitario de Badajoz
Ana Senent Boza: Hospital Universitario Virgen del Rocio (Sevilla)
Sandra del Barrio: Hospital General de Segovia
Jose Luis Romera Martínez: Hospital Universitario Clinico San Carlos
Loles Periañez Gómez: Hospital Universitario Doctor Peset (Valencia)
Cristina Marín Campos: Hospital Universitario de la Princesa (Madrid)
Sergio Rodríguez Rojo: Hospital Universitario de A Coruña
Carla Bettonica Larrañaga: Hospital Universitario de Bellvitge
Sol Bagnaschino Pose: Hospital Universitario de Torrevieja
Gabriel Salcedo Cabañas: Hospital Universitario Fundación Jiménez Díaz
Ramón Castañera González: Complejo Hospitalario Universitario de Palencia
Vanessa Concepción Martín: Hospital Universitario Nuestra Señora de Candelaria
Alessandro Bianchi: Hospital Son Espases en Palma de Mallorca
Dulce Momblán García: Hospital Clínic de Barcelona.