Proctologic issues entail a frequent reason for consultation in the emergency department (ED). We aim to analyze how the SARS-COV-2 pandemic has impacted in the demand for proctological consultations.
Material and methodDescriptive comparative retrospective study of cross-sectional cohorts of patients attending the ED for proctological complaints from March to April in 2020 and 2019. Demographic variables, comorbidities, reasons for consultation and diagnosis, treatment and readmission were included. Four periods were analyzed according to the different stages of the pandemic derived limitations.
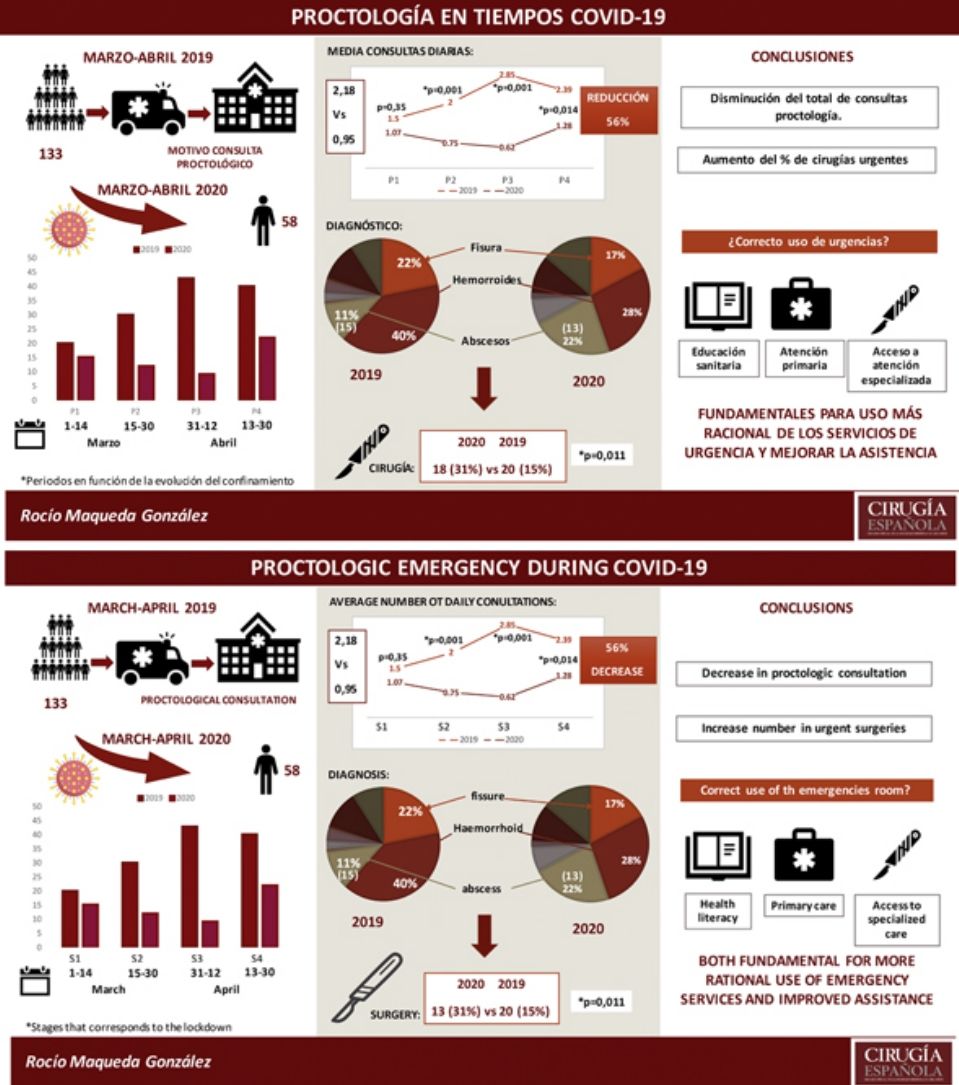
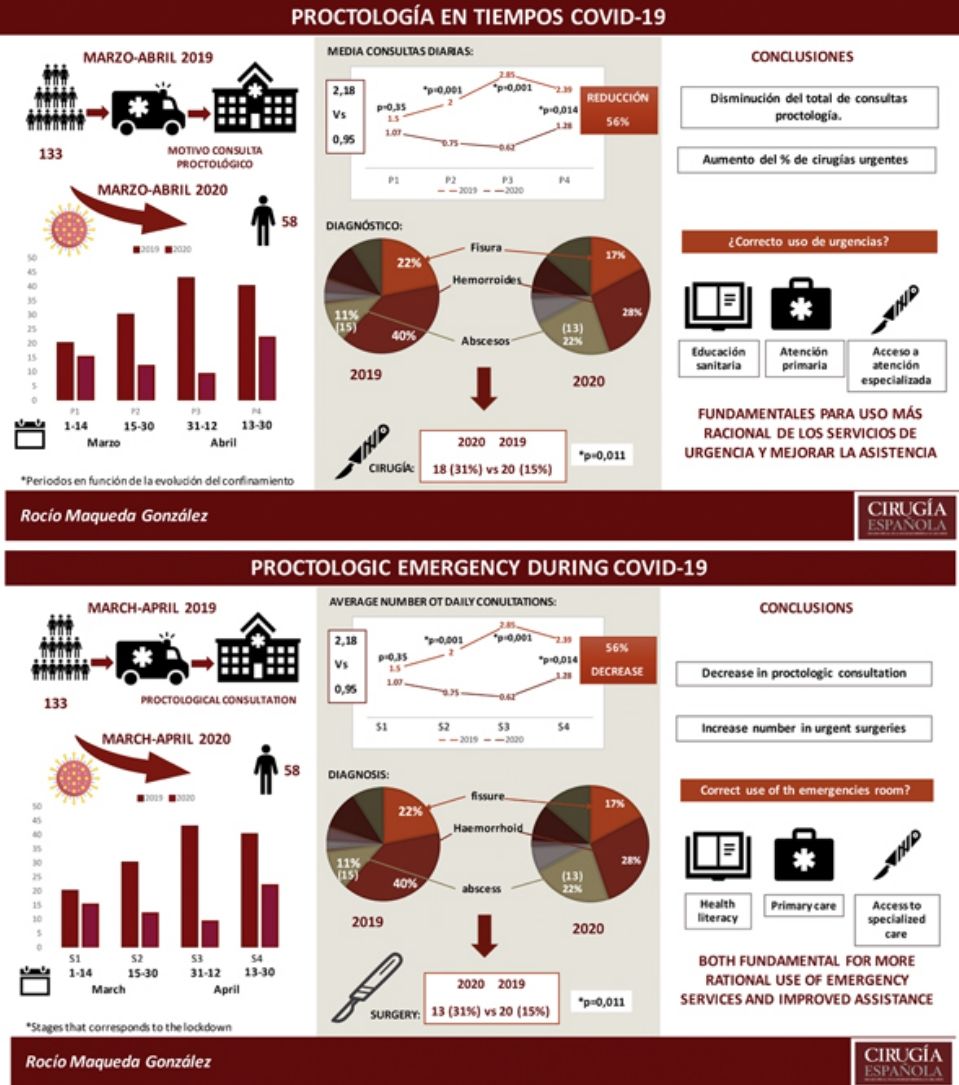
ResultsA total of 191 patients were reviewed, 58 in 2020 and 133 in 2019 with an average age of 48 years (SD 20.1) and 112 (58.6%) males. The average number of daily consultations was 2.18 patients in 2019 versus 0.95 in 2020 (p=0.025) meaning a 56% reduction in consultations for proctological reasons. This difference in average consultations was significant in both periods of lockout (p=0.001) and previous de-escalation (p=0.014). The diagnosis distribution was similar between both periods; however, perianal abscesses doubled their rate in 2020, 22.4% versus 11.3% (p=0.045). There was an increasing need for surgery, 31% vs 15% (p=0.011) with no difference in outpatients regimen after emergency surgery (12.5% vs 7.5%, p=0.201). Three patients in 2020 required readmission to the ED (5.2% vs 12.9%, p=0.086).
ConclusionThere was a decrease of a 56% in proctologic emergency consultation, however, the need for surgery was twice more frequent during the study period. Reflection on the use of emergencies for proctological reasons is warranted.
La enfermedad proctológica supone un motivo de consulta frecuente en los servicios de urgencia. Nuestro objetivo es analizar como la pandemia por SARS-CoV-2 ha impactado en la demanda de consultas proctológicas.
Material y métodoEstudio comparativo retrospectivo de cohortes transversales en el periodo de marzo y abril de 2020 y 2019 de las consultas urgentes por motivos proctológicos. Se incluyeron variables demográficas, antecedentes, motivo de consulta y diagnóstico, tratamiento y readmisión. Se analizaron 4 periodos en función de las distintas etapas del estado de alarma.
ResultadosSe atendieron 191 pacientes, 58 en 2020 y 133 en 2019, con una edad media de 48 años, siendo 112 (58,6%) varones. La media de consultas diarias fue de 2,18 pacientes en 2019 frente a 0,95 en 2020 (p=0,025) suponiendo una reducción del 56%. Esta diferencia fue significativa en ambos periodos de confinamiento (p=0,001) y en la desescalada (p=0,014). La distribución de los motivos de consulta fue similar, sin embargo, los abscesos perianales duplicaron su tasa en 2020, 22,4 frente al 11,3% (p=0,045). Se observó un incremento de la necesidad de cirugía, 31 frente al 15% (p=0,011) sin diferencias en el manejo ambulatorio tras cirugía urgente (12,5 frente al 7,5%; p=0,201). Hubo 3 pacientes en 2020 que requirieron readmisión en urgencias (5,2 frente al 12,9%; p=0,086).
ConclusionesEl número de consultas por enfermedad proctológica urgente ha sufrido una reducción del 56%, sin embargo, las enfermedades que requieren tratamiento quirúrgico se han duplicado en proporción. La reflexión sobre el uso de urgencias por motivos proctológicos es necesaria.
Anorrectal emergencies are well defined: thrombosed external hemorrhoids, acute thrombosed haemorrhoidal prolapse, anal fissure, retained anorectal foreign bodies, and the septic ones as anorectal abscess, pilonidal sinus disease and Fournier gangrene.1
Despite the scarce existing evidence on the matter,2–6 professional experience dictates all these types of pathologies are a frequent reason for consultation in the emergency department (ED).4 Some can be managed with medical treatment meanwhile others require urgent surgical intervention.7,8
SAR-COV-2 pandemic has conditioned a redistribution of the usually attended pathologies in the ED.9–11 Concerning colorectal subspecialty, oncological and inflammatory bowel disease have constituted main concerns.12,13 Proctologic disorders have been another major victim of the pandemic, since in a significant number of cases can be considered non-priority issues, and therefore, following several international clinical guidelines for prioritization of surgical interventions, they have been postponed.14–18 Nevertheless, some authors argue about the potential functional and psychological consequences of the delay in diagnosis and treatment of these afflictions.14,15
In this context, we aim to analyze how the pandemic and its consequences, such as confinement, has impacted in the demand for proctological consultations, as well as, the degree of complexity of these consultations in the ED of our hospital.
MethodsDescriptive comparative cross-sectional cohorts’ study in a single Universitary Tertiary Hospital with a capacity of 564 beds in a metropolitan, middle-high socioeconomic level area with a sanitary population of 323,000 people. Study period was established to be March and April of this year 2020. This period of time has been selected in order to establish a trend during the present year and its modification according to the evolution, both media and officially influenced, of the pandemic. We included data from the same period in 2019 in order to establish a comparison under normal conditions.
Inclusion criteria are proctologic pathology consultation at the emergency department during both study periods and age over 18 years old; no exclusion criteria are determined for the present study. All the patients included in the present study were evaluated by the general surgery team, resident or attendant, during their consultation in the emergency department. We carried out a search for Diagnosis Related Groups (DRG) according to IDC-10 using our centre's computerized information coding system to identify proctological consultation in the ED. The codes included were as follows: fissure and fistula of anal and rectal regions (k60), abscess of anal and rectal regions (K61), other diseases of anus and rectum (k62), hemorrhoids and perianal venous thrombosis (k64), pilonidal cyst (L05) and pruritus ani (L29.0).
We collected demographic variables, comorbidities and chronic treatments, previous proctological pathology, reason for consultation in the ED, definitive diagnosis, medical or surgical treatment required, outpatient or in-hospital regimen, change in attitude with respect to usual behavior in our center in each situation and the need for re-admission or new ED consultation within 30 days after the initial visit. The treatment was stablished by the general surgery team based on definitive diagnosis and usual clinical guidelines for each pathology. No special directions were given for this kind of pathology during the pandemic. The only variable that we have considered differently in the Cohort analyzed in 2020 with respect to 2019 is that of change in attitude, since we understand that this does not make sense in a context of normal epidemiology.
The whole study period was additionally divided in four stages: Stage 1, from the 1st to the 14th of March, that corresponds to the pandemic previous to the lockdown measures, there was not specific measures except among healthcare givers (courses and meetings were canceled) (S1); Stage 2, from the 15th to the 30th of March, that is the settlement of the lockdown (includes limitation of mobility, promotion of teleworking, cancelation of any activity considered non-essential, and closure of borders among provinces) (S2); Stage 3, from the 31st of March to the 12th of April, when a tightening in the lockdown was established (during this period cancelation of any activity considered non-essential such as primary sector, food trading and related activities, took place) (S3); and Stage 4, from the 13th to the 30th of April, previous to formal de-escalation process, with measures similar to S2, until April 26th when kids were allowed to go out, obviously with an accompanying adult (S4).
Proctologic interventions scheduling stopped on March 11th and were not restarted by the end of the study. In-person consultation in the clinic were canceled from march 16th and substituted by tele-medicine (phone-call consultation) during the whole study period, with the only exception of newly diagnosed oncologic patients.
We conducted a descriptive study of both Cohorts. Continuous variables with a non-normal distribution (Kolmogorov–Smirnov test) are presented as median and interquartile range (IQR), while those following a normal distribution are presented as mean and standard deviation (SD). Categorical variables are presented in frequencies. The Mann–Whitney test for continuous variables and the χ2 test (or the Fisher exact test when appropriate) for categorical variables were used for comparisons between groups.
The null hypothesis was rejected when the α or type I error was <0.05.
Statistical analysis was performed with IBM SPSS Statistics v24.0.
The study was approved by the local Clinical Research Ethics Committee (CREC) of the hospital.
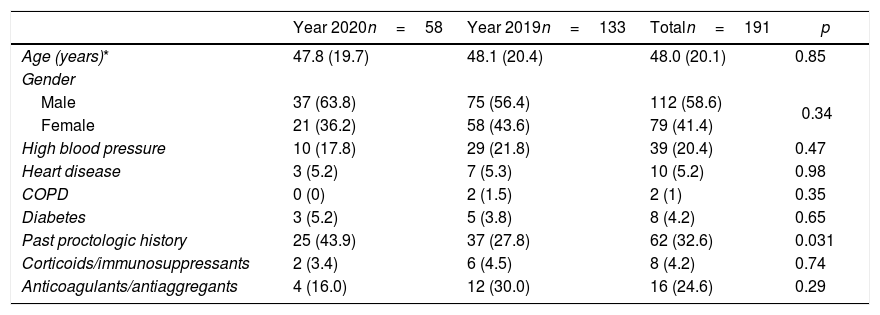
ResultsThe study included 191 patients, 58 from 2020 and 133 from 2019. The median age was 48 (SD 20.1), with 112 males (58.6%) and 79 females (46.4%). Patients’ demographic variables and comorbidities were summarized in Table 1.
Demographic and relevant comorbidities in the whole sample and in each year of study period.
| Year 2020n=58 | Year 2019n=133 | Totaln=191 | p | |
|---|---|---|---|---|
| Age (years)* | 47.8 (19.7) | 48.1 (20.4) | 48.0 (20.1) | 0.85 |
| Gender | ||||
| Male | 37 (63.8) | 75 (56.4) | 112 (58.6) | 0.34 |
| Female | 21 (36.2) | 58 (43.6) | 79 (41.4) | |
| High blood pressure | 10 (17.8) | 29 (21.8) | 39 (20.4) | 0.47 |
| Heart disease | 3 (5.2) | 7 (5.3) | 10 (5.2) | 0.98 |
| COPD | 0 (0) | 2 (1.5) | 2 (1) | 0.35 |
| Diabetes | 3 (5.2) | 5 (3.8) | 8 (4.2) | 0.65 |
| Past proctologic history | 25 (43.9) | 37 (27.8) | 62 (32.6) | 0.031 |
| Corticoids/immunosuppressants | 2 (3.4) | 6 (4.5) | 8 (4.2) | 0.74 |
| Anticoagulants/antiaggregants | 4 (16.0) | 12 (30.0) | 16 (24.6) | 0.29 |
As further illustrated, both were similar except for a higher proportion of patients with previous proctological pathology among the patients attended this year 2020, 43.9% vs 27.8% (p=0.031).
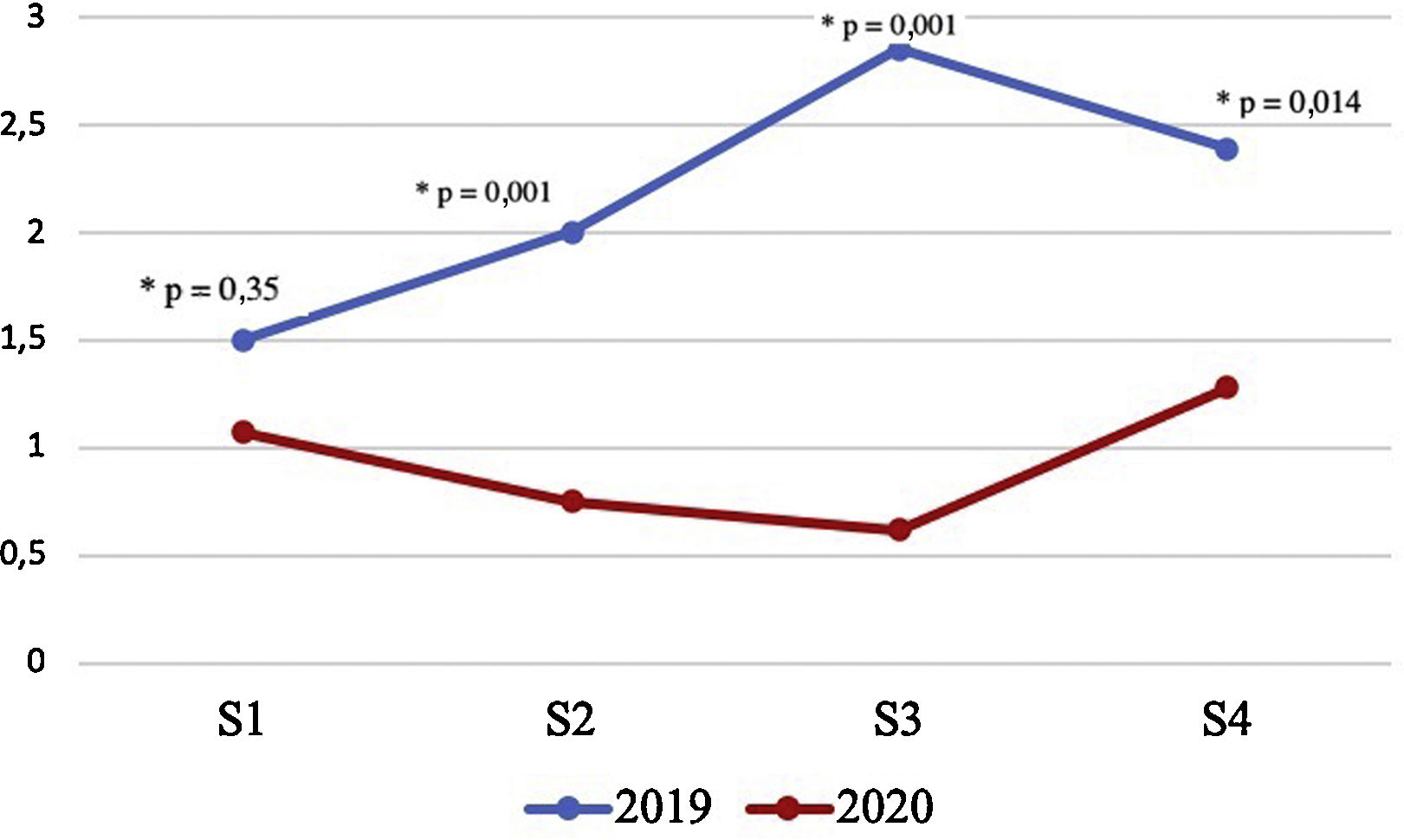
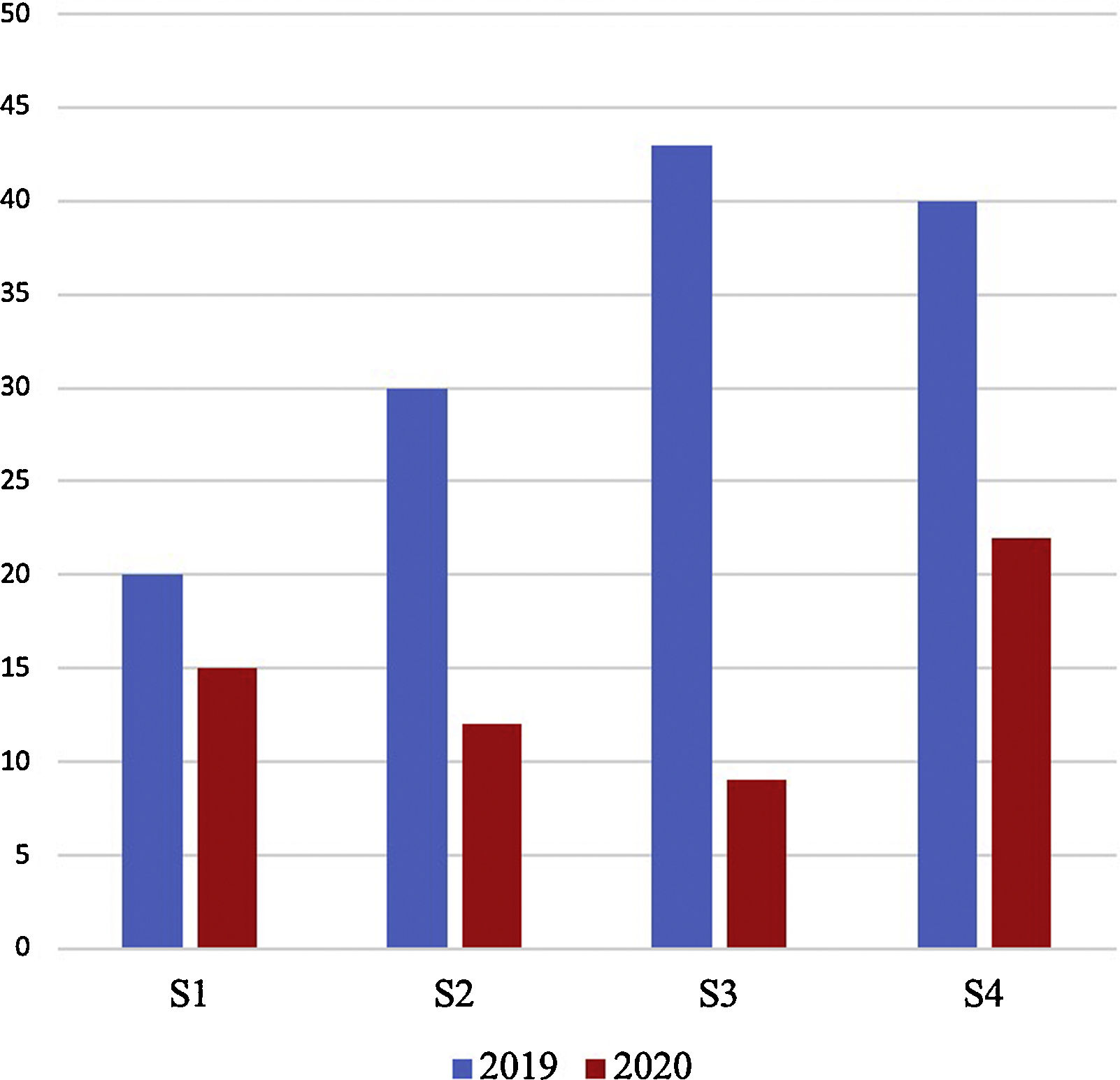
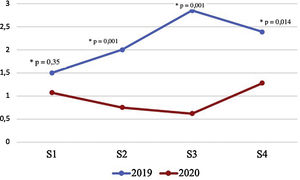
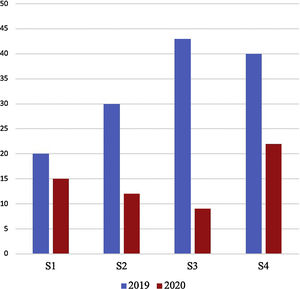
In 2019 the average number of daily consultations for proctological reasons was 2.18 compared to 0.95 in 2020 (p=0.025). This represents a percentage difference in consultations for proctological reasons of 56% compared to the same period of time in the previous year. According to the stages of the pandemic, we found significant differences in the average number of daily consultations during S2 and S3 (p=0.001) and during S4 (p=0.014) (Fig. 1). The total number of patients attended in each of the stages also showed differences between both years (Fig. 2).
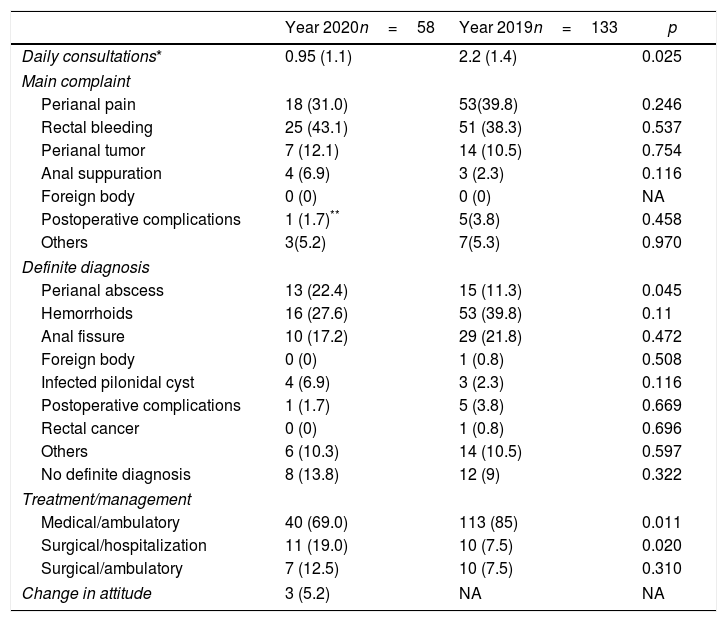
Table 2 summarizes the main reasons for consultation and the diagnoses at discharge that were registered.
Details of emergency department proctologic consultations during the pandemic and the previous historic cohort. Main complaint, definitive diagnosis, required treatment and change in standard of care are shown.
| Year 2020n=58 | Year 2019n=133 | p | |
|---|---|---|---|
| Daily consultations* | 0.95 (1.1) | 2.2 (1.4) | 0.025 |
| Main complaint | |||
| Perianal pain | 18 (31.0) | 53(39.8) | 0.246 |
| Rectal bleeding | 25 (43.1) | 51 (38.3) | 0.537 |
| Perianal tumor | 7 (12.1) | 14 (10.5) | 0.754 |
| Anal suppuration | 4 (6.9) | 3 (2.3) | 0.116 |
| Foreign body | 0 (0) | 0 (0) | NA |
| Postoperative complications | 1 (1.7)** | 5(3.8) | 0.458 |
| Others | 3(5.2) | 7(5.3) | 0.970 |
| Definite diagnosis | |||
| Perianal abscess | 13 (22.4) | 15 (11.3) | 0.045 |
| Hemorrhoids | 16 (27.6) | 53 (39.8) | 0.11 |
| Anal fissure | 10 (17.2) | 29 (21.8) | 0.472 |
| Foreign body | 0 (0) | 1 (0.8) | 0.508 |
| Infected pilonidal cyst | 4 (6.9) | 3 (2.3) | 0.116 |
| Postoperative complications | 1 (1.7) | 5 (3.8) | 0.669 |
| Rectal cancer | 0 (0) | 1 (0.8) | 0.696 |
| Others | 6 (10.3) | 14 (10.5) | 0.597 |
| No definite diagnosis | 8 (13.8) | 12 (9) | 0.322 |
| Treatment/management | |||
| Medical/ambulatory | 40 (69.0) | 113 (85) | 0.011 |
| Surgical/hospitalization | 11 (19.0) | 10 (7.5) | 0.020 |
| Surgical/ambulatory | 7 (12.5) | 10 (7.5) | 0.310 |
| Change in attitude | 3 (5.2) | NA | NA |
NA: not applicable.
No differences were found in the distribution of the different reasons for consultation; however, according to definitive diagnoses there was an increase in the diagnosis of perianal abscesses, 11.3% in 2019 versus 22.4% in the present year (p=0.045).
Regarding the treatment applied, there was an increase in the need for surgery (31% vs 15%, p=0.011) during 2020, with no difference in the proportion of outpatient regimen after emergency surgery (12.5% vs 7.5%, p=0.310).
Only three of the patients in 2020 required readmission to the ED, 5.2% vs 12.9% in 2019 (p=0.086).
It was interpreted as a change in attitude in only three of the patients attended during 2020: two of them were managed in ambulatory regimen after surgical treatment and in the other one outpatient medical treatment was indicated. One of the patients with ambulatory surgical treatment was readmitted to the ED within the established 30-day follow-up period.
DiscussionThe number of consultations for proctological pathology in the emergency department of our hospital has clearly decreased this year during the pandemic period, with a percentage of difference of 56%. The average number of patients daily attended this year compared to the same period last year has been significantly lower (2.2 in 2019 versus 0.95 patients this year; p=0.025).
A general decrease in ED visits for other diseases has been described,16,17 with an increase in severity due to a delay in medical consultation and therefore in diagnosis. Within our specialty surgery some authors have drawn attention to a similar situation,11,18 but this is the first study that specifically analyzes what has happened in the field of emergency proctological pathology. In all these cases, it seems logical that the reason for this decrease in urgent consultations is not a decrease in frequency but rather a modification in consultation habits. On one hand, it has been demonstrated that fear of contracting COVID-19 disease has generated an increase in anxiety in the population19 and fear of contagion may have been a fundamental cause of the decrease in ED visits. On the other hand, the absolute interruption of care in consultations of this type of patient, the possible evolution of their symptoms, or even the uncertainty and concern generated by such a situation,12,13 could also have been a factor in “pushing” patients toward consultation in the ED.
In our study, another very significant fact is that the proportion of patients who required surgical treatment to solve their problem was higher this year, without any changing in the absolute number of patients. All these observations require a consideration about the use of medical emergencies in our country. Given the fact that consultations for perianal sepsis remained at similar figures to those of last year, although double in rate, our interpretation is that in a high percentage of cases these visits to the ED are not entirely justified and, for that reason, given the threat posed by going to a hospital in a pandemic period during the current year, patients preferred to postpone the consultation. Appropriateness of ED consultation has been previously studied. As an example, Bahadori et al. found that a huge minority of patients who attended to an ED, just 5%, argued a real sense of urgency to do so; conversely, several unsuitable reasons were listed such as geographical closeness in 8.5%, past medical history records to be at the hospital in 29.5%, seeking early or free or inexpensive care in 36%. An extra 8.4% declared to have been referred by their general practitioner.20
Obviously, the intention with this reflexion is not to blame patients of this situation, but rather analyzing the weak points, the needs and what are the possible ways of improving our health system. Accordingly, we discuss three feasible alternatives that may result in an improvement in the use it is made of the ED: improving health literacy in general population, improving referral times from primary care to specialized care, and strengthening general practitioners’ training in certain types of highly prevalent pathologies such as proctology.
Health literacy is defined as the degree to which each individual has the capacity to obtain, process and understand basic health information.21 It constitutes a multifactorial approach involving individual and contextual population factors, factors related to health professionals and factors related to the health system.22 The effects that competent health education can achieve range from a more rational and efficient use of resources, to a lower degree of dependency including a positive impact on mortality associated with some processes. With all these data, health literacy has become one of the priorities for the 21st century in the field of health.22 According to a European survey carried out in 2015, 58.3% of Spaniards had inadequate health literacy,23 and this might be a future field for improvement.
Considering that another of the key aspects that condition the search for emergency services among patients is immediacy of care, regardless of the feeling of “real urgency”,20 one of the measures that seems necessary to implement in our system is better and faster access from the primary care setting to specialized care. This would have an impact on improving the perceived delay by the patient and would probably help to avoid overcrowding in the emergency departments. This is an aspect that has been widely studied in cancer patients of different types,24 even in other benign colorectal pathologies,25 but has not been analyzed in proctological processes, despite the known impact on quality of life.
Another reason for patients to avoid primary care is the low expectation of obtaining resolution of their problem.25 There is also evidence that specific and specialized education in primary care physicians and nurses is an essential strategy with a direct impact on emergency department crowding.26
Finally, in addition to all these measures which can bring about great improvements in the system, more specifically in the area of coloproctology, a possible area of improvement that could be very relevant in new outbreaks of the disease would be the performance of proctological surgical procedures on an outpatient basis from the emergency departments.5,12 Similarly, a better provision of resources (infrastructure, materials and personnel) in outpatient departments would even allow small invasive procedures to be taken on3 and relieve the burden of hospital activity. Despite all that, this is an aspect scarcely analyzed to date and the available results are limited and therefore the implementation of any activity of this type should be carried out under strict protocols and with the utmost caution.5 Nevertheless, the satisfaction perceived by patients could justify its future development.27 In this area, in our series, surgical treatment was performed on an outpatient basis in 7.5% of patients in 2019 and in 12.5% in 2020, with only one case of readmission; therefore, it can be considered a safe policy.
Each of these measures separately and, even more, the combination of all of them, would probably allow us to see a more rational use of the emergency services and improve care and patient satisfaction in terms of the perceived quality of healthcare received overall not only in pandemic times.
The main limitations of our study are its unicentric and retrospective nature. Among its strengths we would highlight that it is an original analysis to date and that it translates in a simple and graphic way what happened in our emergency departments during the pandemic period.
In conclusion, the impact of the pandemic on the epidemiology of proctological consultations in the emergency department has been evident, with an overall reduction of 56%. Taking into account that those pathologies requiring surgical treatment, and which evolution may vary without the application of such treatment, have doubled in proportion, reflection on possible causes and planning eventual solutions for a more suitable use of the ED consultation in this subspecialty is warranted.
Finally, the fear, probably unfounded, about the possible sequelae of the pandemic in other “minor pathologies”, e.g. proctologic ones, and its implications in terms of delayed diagnosis and prognosis are dismissed in the light of our results.
Ethical declarationAll procedures carried out in studies with human participants were in accordance with the ethical standards of the institutional and/or national research committee and the Declaration of Helsinki of 1964 and its subsequent modifications or comparable ethical standards.
FundingNone declared.
Conflict of interestsThe authors declare that they have no conflict of interest.