Most parathyroid adenomas are located in the neck. Only 6–30% of them are located in the mediastinum. Mediastinal ectopic parathyroid tumours can arise in all three mediastinal compartments. Posterior location is less frequent and involves greater technical difficulty.1 We present the robotic approach and complete resection of the ectopic parathyroid tumour with complete analytical resolution. Robotic resection is feasible in these rare and infrequent locations.
A 61-year-old female ex-smoker with no previous medical history is diagnosed with hypercalcemia after a densitometry requested by a gynaecological review. The biochemical study showed elevated calcium 2.92mmol/L (reference range 2.15–2.51), decreased phosphates 0.59mmol/L (reference range 0.85–1.50), hypercalciuria 436mg/dl (>400mg/dl), elevated parathyroid hormone (PTH) level 23pmol/L (reference range 1.6–6.9), decreased vitamin D 29.3nmol/L (reference range 50–250) and normal albumin.
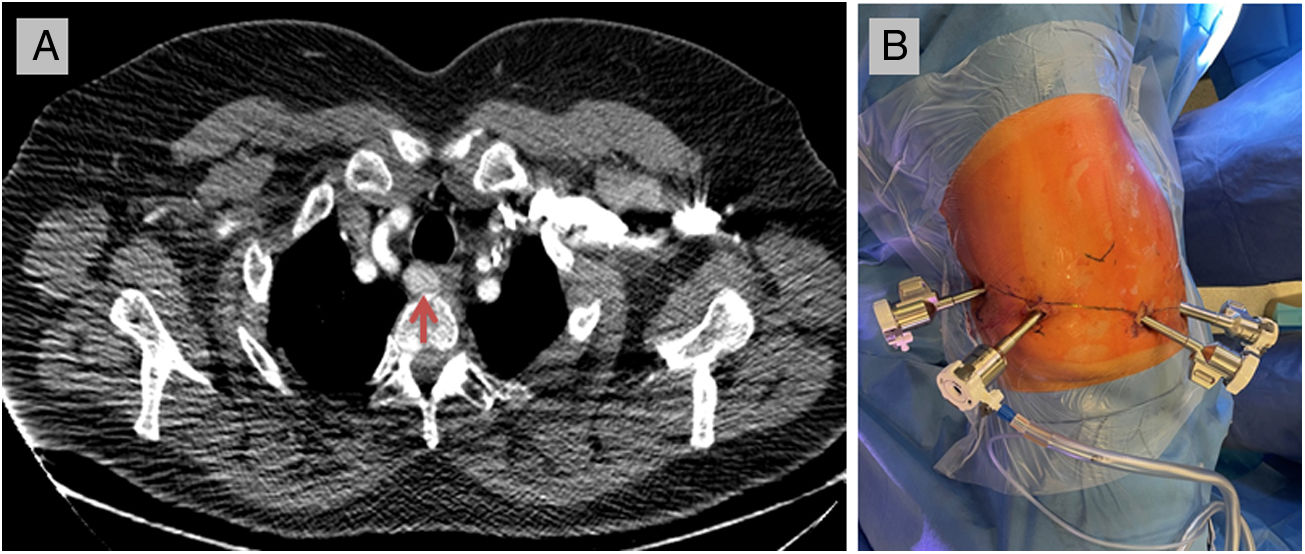
A 99 mTc sestamibi scintigraphy confirmed a localized hyperfunctioning parathyroid tissue retro tracheal at the level of 3rd thoracic vertebra. Neck and chest Computed tomography (CT) showed a 19mm×16mm×32mm nodule in the upper posterior mediastinum, retrotracheal and right paraesophageal (Fig. 1). She was diagnosed with Primary Hyperparathyroidism (PHPT) caused by a rare ectopic mediastinal parathyroid tumour.
Based on these findings, an informed consent was obtained from the patient before surgery. The operation was performed via full robotic thoracic surgery (da Vinci Xi robot system® – Intuitive Surgical Sarl, Aubonne, Switzerland).
Under general anaesthesia with double-lumen endotracheal intubation for left single-lung ventilation, four robotic operating ports of 8mm were placed in the 6th intercostal space. A port for the 30-degree endoscope was placed at the mid-axillary line. The right lung was deflated, and CO2 insufflation was set at 5–10mm Hg through the non-camera port with careful haemodynamic monitoring.
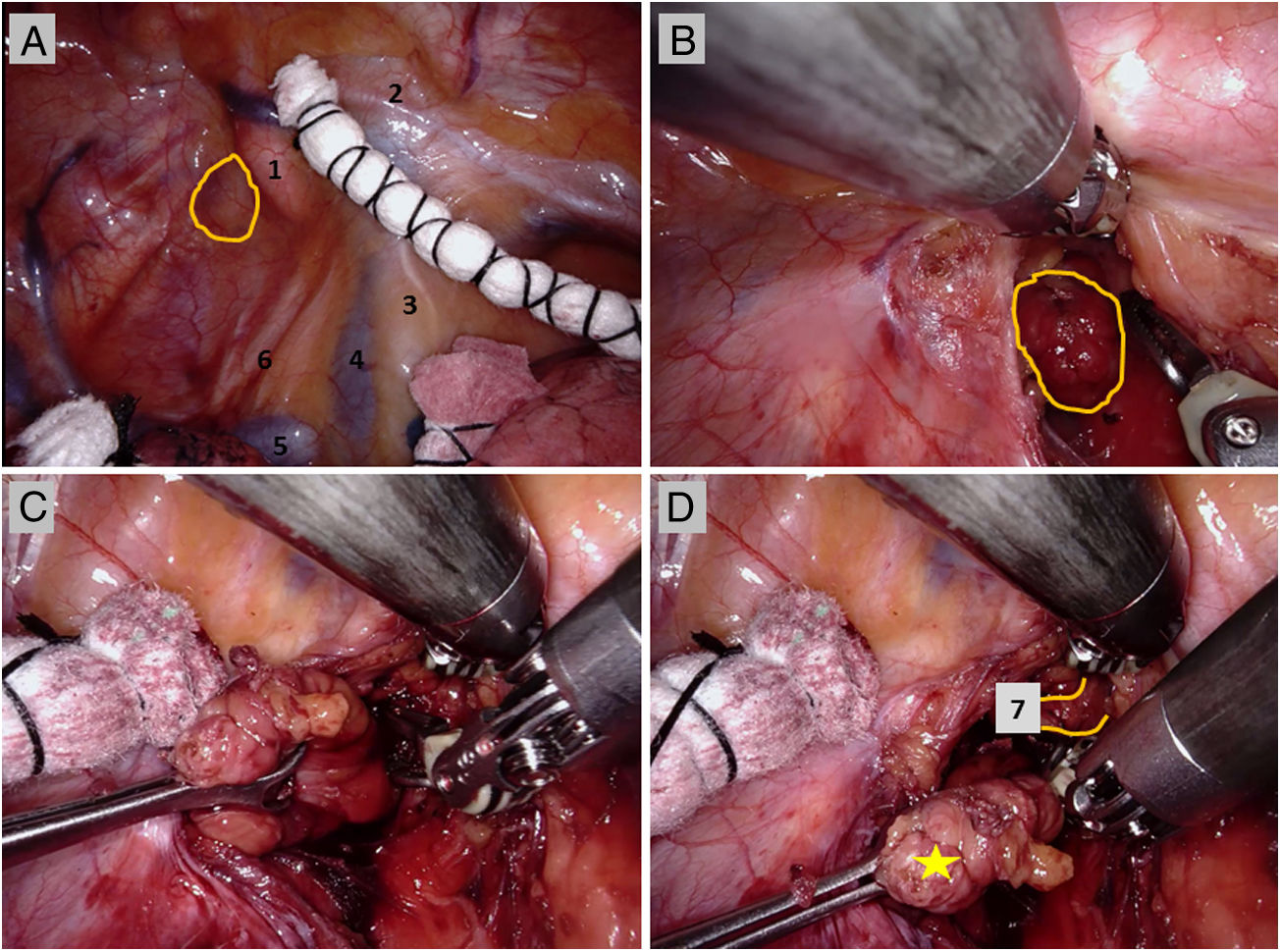
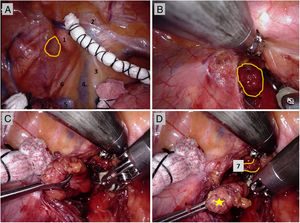
Fenestrated bipolar forceps (EndoWrist® Bipolar) on the left hand (robotic port 3) and Maryland bipolar forceps (EndoWrist® Bipolar) on the right hand were used for dissection (robotic port 1). A Tip-Up Fenestrated Grasper was placed on the right hand (robotic port 4) to separate the lung (Fig. 2). Dissection was started by opening the mediastinal pleura behind the superior vena cava, identifying the vagus nerve, trachea, and oesophagus. The parathyroid gland was identified behind the trachea and the right subclavian artery and to the right of the oesophagus. A careful dissection of the gland was performed, identifying the right lower laryngeal nerve and achieving complete resection (Fig. 2). The tumour was extracted with an endoscopic babcock forceps and endobag through robotic port 3. A 24-F chest tube was left in place after expansion of the lung under direct visualization. Twenty-four hours after surgery the patient was discharged without complications and calcium level was 2.39mmol/L and PTH level was 1.4pmol/L.
(A) “1” right subclavian artery; “2” internal thoracic artery; “3” phrenic nerve; “4” superior vena cava; “5”: acygos vein; “6” vagus nerve. Yellow circle shows the imprint of the tumour on the mediastinal pleura. (B) Yellow circle shows the tumour. (C) The tumourwas extracted with an endoscopic babcock forceps. (D) Yellow star shows the resected tumour and “7” right common carotid artery.
Primary hyperparathyroidism is characterized by hypersecretion of parathyroid hormone resulting in hypercalcemia and hypophosphatemia. The superior parathyroid glands derive from the fourth pharyngeal sac and descend along with the thyroid gland and oesophagus. Consequently, parathyroid tissue can be found in the posterior mediastinum. The lower parathyroid glands derive from the third pharyngeal sac, located next to the thymus in the anterior mediastinum.2 In our case, it was considered to be ectopic mediastinal parathyroid tumour derived from superior parathyroid gland.
The treatment of choice for mediastinal parathyroid adenoma with PHPT is surgery.1 In 1994 the first video-assisted thoracoscopic surgery (VATS) resection of a mediastinal parathyroid adenoma was performed by Prinz et al. 3and ten years after, Profanter et al.4 performed the first robot-assisted thoracoscopic resection of a mediastinal parathyroid adenoma. Since the introduction of minimally invasive surgery, multiple studies have been reported with good results and low morbidity and mortality.5
The implantation of robotic surgery is a superior evolution of minimally invasive surgery with the known facilities of greater and better vision, better mobility, more accurate dissection and less postoperative pain.6,7 Scott et al.,8 in 2019 described the largest cohort of patients who underwent robot-assisted mediastinal parathyroidectomy. In our opinion, the robotic approach by introducing all the arms through the same intercostal space minimizes possible postoperative pain in addition to the already known advantages of robotic surgery, and we believe that it is feasible to perform it without an assisted incision or placing the trocars in different intercostal spaces, which causes greater postoperative pain, as described by other authors.9,10
We consider that minimally invasive surgery is the approach of choice in mediastinal tumours.1 Thoracotomy and sternotomy, as an open approach, should be considered as “second option surgical approach”, except in those cases where the tumour size or oncological criteria contraindicates the endoscopic approach. The advantage of robotic surgery allows approaching all mediastinal compartments more easily than VATS with better vision,6 although there is lack of high quality evidence that robotic surgery is superior to VATS in terms of complications, conversion rates, and oncological radicality.7 Nevertheless, in our opinion, robotic surgery allows a more accurate mediastinal dissection as reported by Wilson et al.11 When mediastinal parathyroid lesion is located in the superior and posterior mediastinum, the placement of trocars in the 6th or 7th intercostal space seems to be an option for resection.
FundingNone.
Conflict of interestThe authors declare no conflicts of interest.