Faecal incontinence (FI) is a highly prevalent disorder that severely affects the health related quality of life (HRQOL) of the patients who suffer from it. Neuromodulation is a minimally invasive treatment that has demonstrated its efficacy in the treatment of FI symptoms over the past 10 years. The aim of this study is to check whether there is an improvement in the quality of life, using EuroQuol (EQ-5D), in patients with faecal incontinence treated with sacral root neuromodulation.
MethodologyAn observational study with prospective recording of quality of life data, before and after, using the EuroQuol 5D on a series of patients diagnosed with moderate to severe FI with a complete or repaired sphincter who had a definitive MEDTRONIC Interstim® 3023 implant after a subchronic stimulation phase with a good response.
ResultsThe initial mean number of leaks was 3.1±1, and the final was 0.5±0.6. The mean number of escapes per week decreased to 2.6 escapes (95% CI: 2.1–3.1) after the definitive implant of the sacral root stimulator (P<.001). The mean baseline health status score was 55.9±13, and after neuromodulation it was 63.1±13. Thus, the visual analogue scale score increased by 7.1 points (95% CI: 0.37–14) after the definitive implant of the sacral root stimulator (P<.05). In the HRQOL variables studied with the EQ-5D questionnaire, we found an improvement with neuromodulation in the mobility and the presence of anxiety and/or depression variables. On the other hand we found an improvement with the neurostimulator implant, which was not significant, in personal care, performing daily activities and the presence of pain and/or discomfort. The current health was better in 11 patients (57.9%), the same in 7 (36.8%) and worse in 1 (5.3%).
ConclusionsNeuromodulation is a therapy that has demonstrated a significant improvement in HRQOL measured with the EQ-5D.
La incontinencia fecal es un trastorno de elevada prevalencia que afecta gravemente a la calidad de vida relacionada con la salud (CVRS) de los pacientes que la padecen. La neuromodulación es un tratamiento mínimamente invasivo que ha demostrado su eficacia en el tratamiento de los síntomas de IF durante los últimos 10 años. El objetivo de nuestro trabajo es comprobar si existe una mejora en la calidad de vida, utilizando el EQ-5D, en los pacientes con incontinencia fecal tratados con neuromodulación de raíces sacras.
MetodologíaEstudio observacional con recogida prospectiva de datos de calidad de vida, antes y después, utilizando el EuroQuol 5D sobre una serie de pacientes con diagnóstico de IF moderada o severa con esfínter íntegro o reparado a los que se ha implantado de forma definitiva el neuroestimulador MEDTRONIC Interstim® 3023 tras una fase de estimulación subcrónica con buena respuesta.
ResultadosEl número medio de escapes inicial es de 3,1±1 y el final 0,5±0,6. El número medio de escapes por semana se reduce en 2,6 escapes (I.C. 95%: 2,1–3,1) tras el implante definitivo del estimulador de raíces sacras (p<0,001). La media de la puntuación del estado de salud en el momento basal es de 55,9±13, y tras la neuromodulación es de 63,1±13. Así, La puntuación de la escala analógica-visual aumenta en 7,1 puntos (I.C.95%: 0,37–14) tras el implante definitivo del estimulador de raíces sacras (p<0,05). En las variables de CVRS estudiadas con el cuestionario EQ-5D, encontramos mejoría con la neuromodulación en las variables de movilidad y presencia de ansiedad y/o depresión. En cambio encontramos una mejoría pero no significativa con la implantación del neuroestimulador en el cuidado personal, realización de actividades cotidianas y presencia de dolor y/o malestar. Además la salud actual es mejor en 11 pacientes (57,9%), igual en 7 (36,8%) y peor en 1 (5,3%).
ConclusionesLa neuromodulación es una terapia que ha mostrado una mejora significativa en la CVRS medida con el EQ-5D.
Neuromodulation is a minimally invasive and effective treatment for faecal incontinence (FI).1 It is a proven effective treatment for other conditions such as persistent constipation and severe anal or perineal pain unresponsive to other therapies.2
FI is a highly prevalent disorder in the general population: over 1 in 10 adult women in the population suffers from it, and almost 1 in 15 of them has moderate or severe faecal incontinence. It has a major impact on the quality of life (QOL)3 and the use of medical resources, especially in women with moderate to severe symptoms.4–6 However, in Spain there is variability in the evaluation of FI by different specialists.4
Instruments for measuring health status can be classified into two main types: generic and specific. The first type compares different conditions and obtains reference population values, but is not as sensitive for a particular health problem, such as FI.7
The impact of incontinence (with its different types and degrees of severity) on the quality of life and the changes experienced by patients after treatment have begun to be measured objectively only in recent years, using generic and specific questionnaires.
One of the most important generic questionnaires is EuroQol 5D (EQ-5D),8,9 which is an internationally accepted tool, validated and culturally adapted to the Spanish population. It has standard scores obtained from the general population, which can be used as benchmarks to compare scores obtained by patients in the study and to define the impact of disease on the health-related quality of life (HRQoL).
Although we know the impact of FI on patients, only one study has measured the impact that neuromodulation has on their quality of life using other measuring instruments.10
The aim of our study was to find out if the QOL of patients with FI improved after treatment with sacral root neuromodulation.
Materials and MethodsThis was an observational study with prospective data collection from 23 patients who underwent neuromodulation with the definitive sacral root neurostimulator (InterStim INS, Model 3023, Medtronic, Minneapolis, USA) for FI in our hospital between September 2006 and March 2010.
Our hospital approved the use of neuromodulation for moderate or severe FI (>2 episodes per week) after conservative treatment had failed, with the anal sphincter intact or when it had been repaired by a sphincteroplasty. Patients were excluded for having any of the following: previous surgery on the sacrum, impaired cognitive level (unable to understand how the technique worked), irreversible blood dyscrasias, pregnancy, pacemakers or cardiac arrhythmias, contraindications to anaesthesia, or not giving informed consent.
Patients eligible for neuromodulation also underwent a study which included the following: a general medical history to assess possible etiological factors, duration of symptoms and previous treatments; anal examination (inspection and rectal examination); anal manometry (Alban Medical Ltd.) and endoanal ultrasound (Bruel & Kjaer, Leopard model, with rigid 360° probe).
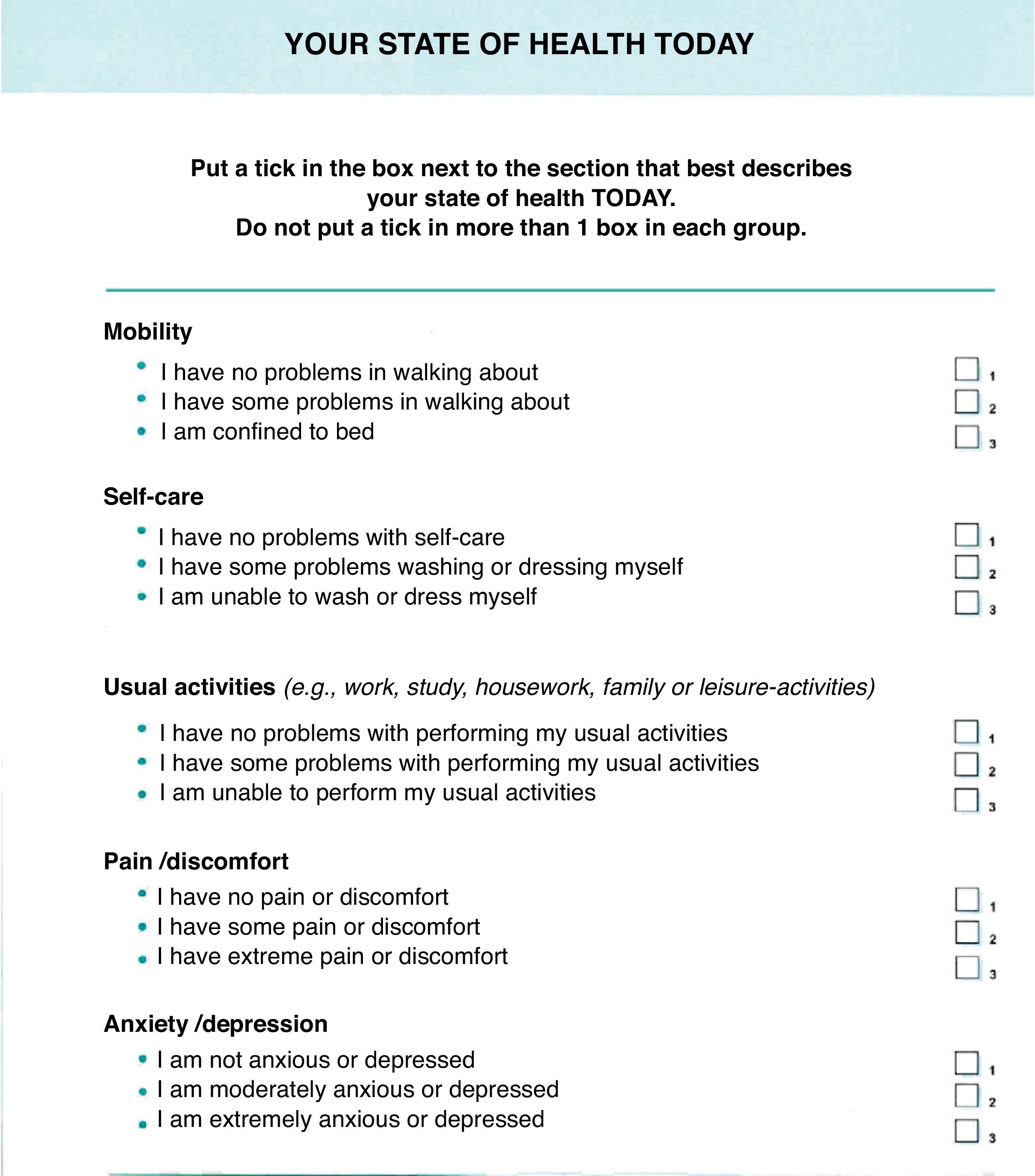
Patients were given the self-completion questionnaire EuroQol EQ-5D (Fig. 1) to measure their HRQoL before surgery and 6 months afterwards. It consisted of two parts: the first was to define their health status according to the EQ-5D multi-attribute classification system, which is composed of five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression), each with three levels (“no problems”, “some problems” and “serious problems”). The second part is a visual analogue scale (VAS) from 0 (worst imaginable health state) to 100 (best imaginable health state). Respondents were asked to indicate their current health status by crossing out the box for the most appropriate level of problems for each dimension. This assessment produced a one-digit number (1, 2 or 3) which expressed the selected level for each dimension. Thus, information about their own health assessment was used to analyse changes in the health status of the group of individuals.
Surgical TechniqueThis was divided into the following stages:
- -
Acute stimulation: To evaluate the integrity and functional relevance of the sacral nerve roots in the functioning of the striated muscles in the anal sphincter. Under local anaesthesia, the sacral foramina of the sacral roots S3 and S4 were located and referenced. Under fluoroscopic control, the needle carrying the 4-pole stimulating electrode (R 3889-28, Medtronic, Minneapolis, USA) was inserted in these sacral foramina. The responses to stimulation at different voltages were measured, and the stimulating electrode was left in the sacral foramen root that gave the best sensory-motor response, while connected to an external current generator.
- -
Subchronic stimulation: The patient assessed the effectiveness of the stimulating current.
- -
Permanent stimulation: Under local anaesthesia, a subcutaneous space was created in the buttocks, and an internal battery inserted, which replaced the external one. The definitive location for the neuromodulator was decided after a 50% improvement in the number of faecal leaks over a 3-week evaluation period was seen.11 In our cohort, neuromodulation was indicated in 28 patients, 5 of whom were not included in the study due to the lack of response at the subchronic stimulation stage.
The stimulus amplitude ranged from 0.5V to 1.5V, with constant pulse width and frequency (210ms and 25Hz, respectively). Stimulation was performed continuously in all patients.
Data CollectionData collection was performed at the following times:
- -
Baseline, at the time of inclusion in the study;
- -
Surgical procedure: During this stage only the technical variables related to the therapy were collected–the implantation procedure for the electrodes (stimulation test stage and final implant stage);
- -
Visit 6 months after final implantation.
The results were expressed as mean±standard deviation and percentages with 95% confidence intervals. Comparison of the variables before and after the intervention was performed using the Friedman test for related quantitative data and the McNemar test for paired qualitative data. Comparison of the outcome variables with the other variables was performed using Pearson's chi-square test or Fisher's exact test, and by Student's t-test or the Mann–Whitney test for the relationship between quantitative variables, depending on whether the distribution was normal or not and for dichotomous qualitative variables. The relationship between quantitative variables, with or without normal distribution, and a qualitative one with more than two options was performed using a one-way ANOVA or Kruskal–Wallis test. The correlation analysis to quantify the association between variables was performed using Spearman's rho correlation coefficient. All analyses were two-tailed. The software packages used were Granmo 7.04 and SPSS 15.0 for Windows.
ResultsThe final implant was performed in 23 patients, 21 women (91.3%) and 2 men (8.7%), with a mean age of 51.17±12.9 years for the onset of symptoms and 60.79±10.9 years for the implant.
The indication for intervention was faecal incontinence in the 23 patients.
Regarding medical history, there were 8 women (38.09%) who were multiparous, with an average of 3.4 births; 2 patients (8.7%) underwent surgery for cystocele; 3 patients (13%) for an anal fistula, 4 patients (17.4%) for haemorrhoids, 1 patient (4.3%) for rectal cancer, and 1 patient (4.3%) for prostate cancer.
One electrode was implanted in 21 patients (91.3%), while 2 electrodes were needed for 2 patients (8.7%) due to suboptimal improvement in their symptoms with 1 electrode. After implanting a second 4-pole electrode in these 2 patients, they underwent a significant improvement (>50%) and a permanent stimulator was implanted. The average time between implantation of the temporary and permanent stimulator (subchronic stimulation stage) was 32.39±20 days.
Initially, the average number of faecal leaks was 3.1±1 and finally was 0.5±0.6. The weekly average number of faecal leaks fell by 2.6 (95% CI: 2.1–3.1) after the definitive implantation of the sacral root stimulator (P<.001).
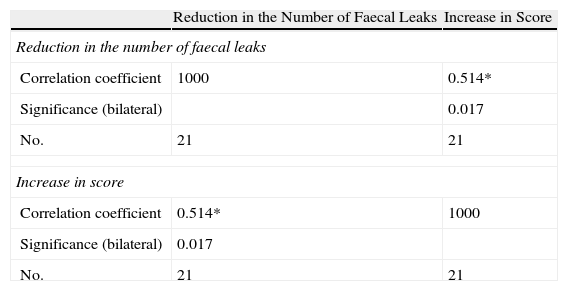
Table 1 shows the statistical significance for a Spearman's rho correlation coefficient value of 0.514 (95% CI: −0.02; 0.71), meaning that the two variables are correlated. The correlation is positive and smooth: the greater the reduction in the number of leaks, the greater the increase in the visual analogue scale for the quality of life.
Correlation Between the Number of Incontinence Episodes and Quality of Life Visual Analogue Scale.
| Reduction in the Number of Faecal Leaks | Increase in Score | |
| Reduction in the number of faecal leaks | ||
| Correlation coefficient | 1000 | 0.514* |
| Significance (bilateral) | 0.017 | |
| No. | 21 | 21 |
| Increase in score | ||
| Correlation coefficient | 0.514* | 1000 |
| Significance (bilateral) | 0.017 | |
| No. | 21 | 21 |
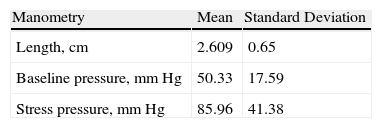
The manometric results were as follows: average length 2.609±0.65cm, mean baseline pressure 50.33±17.59mm Hg and a stress pressure of 85.96±41.382mm Hg. Also, endoanal ultrasonography revealed partial defects in the anterior portion of the external sphincter in 10 patients (43.5%), although no case had a disruption throughout the whole thickness (Table 2). A statistically significant relationship was found between the low baseline pressure variable and improvement in the EQ-5D variable for pain and discomfort (P=.02). No significant relationship was found among the other findings by ultrasound or by manometry and the EQ-5D results.
Manometer and Endo-Anal Ultrasound Data.
| Manometry | Mean | Standard Deviation |
| Length, cm | 2.609 | 0.65 |
| Baseline pressure, mm Hg | 50.33 | 17.59 |
| Stress pressure, mm Hg | 85.96 | 41.38 |
| Endo-Anal Ultrasound | Frequency | Percentage |
| Intact sphincters | 12 | 52.2 |
| Partial defect sphincters | 10 | 43.5 |
| Repaired sphincters | 1 | 4.3 |
The mean health score at baseline was 55.9±13 and 63.1±13 after neuromodulation. Thus, the visual analogue scale score increased by 7.1 points (95% CI: 0.37–14) after the definitive sacral root stimulator implant (P<.05).
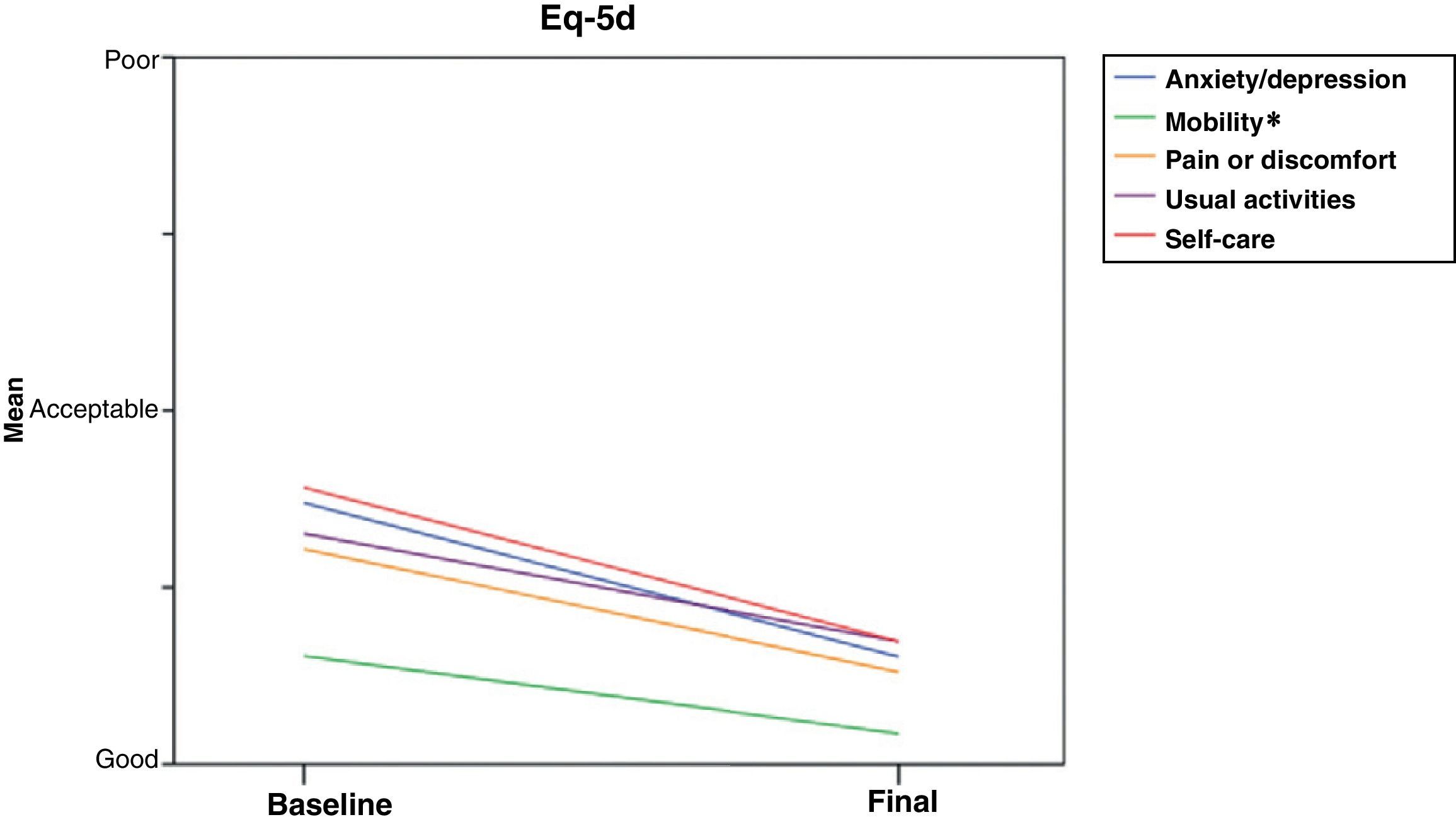
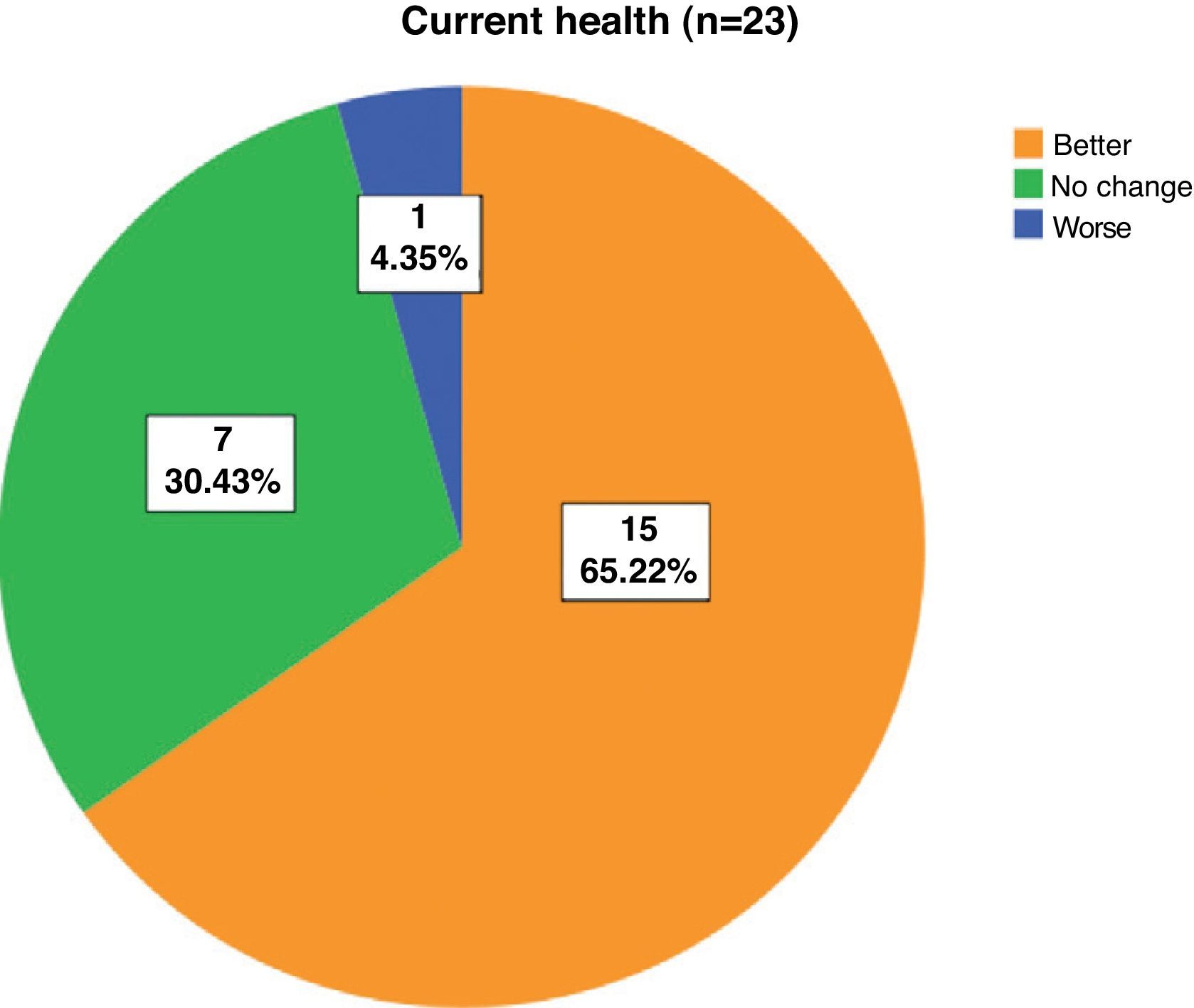
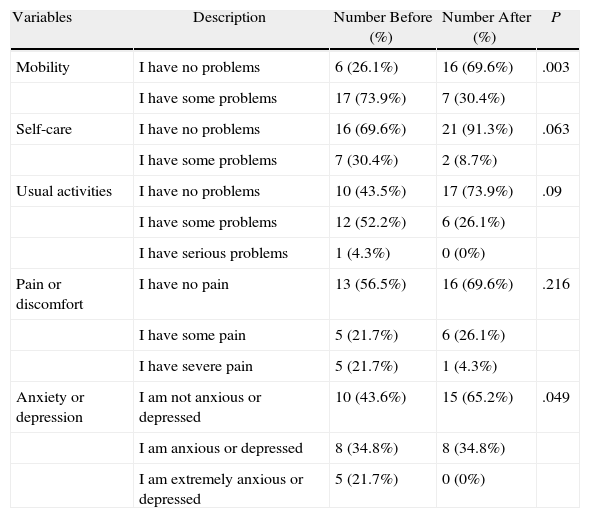
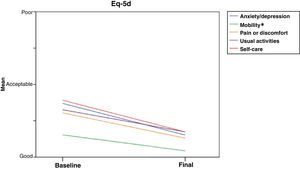
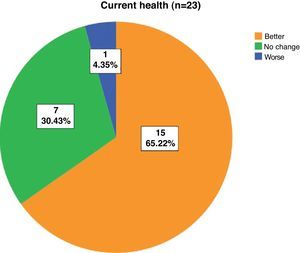
For the HRQoL variables studied with the EQ-5D questionnaire (Table 3), a significant improvement was found with neuromodulation in the variables of mobility, and presence of anxiety and/or depression. Although not statistically significant, improvements were also found in self-care, usual activities and pain/discomfort (Table 3, Fig. 2) after the neurostimulator implantation. In addition, the current health was better in 11 patients (57.9%), the same in 7 (36.8%) and worse in 1 (5.3%), see Fig. 3.
Description of Variables and Their Relationship With Neuromodulation.
| Variables | Description | Number Before (%) | Number After (%) | P |
| Mobility | I have no problems | 6 (26.1%) | 16 (69.6%) | .003 |
| I have some problems | 17 (73.9%) | 7 (30.4%) | ||
| Self-care | I have no problems | 16 (69.6%) | 21 (91.3%) | .063 |
| I have some problems | 7 (30.4%) | 2 (8.7%) | ||
| Usual activities | I have no problems | 10 (43.5%) | 17 (73.9%) | .09 |
| I have some problems | 12 (52.2%) | 6 (26.1%) | ||
| I have serious problems | 1 (4.3%) | 0 (0%) | ||
| Pain or discomfort | I have no pain | 13 (56.5%) | 16 (69.6%) | .216 |
| I have some pain | 5 (21.7%) | 6 (26.1%) | ||
| I have severe pain | 5 (21.7%) | 1 (4.3%) | ||
| Anxiety or depression | I am not anxious or depressed | 10 (43.6%) | 15 (65.2%) | .049 |
| I am anxious or depressed | 8 (34.8%) | 8 (34.8%) | ||
| I am extremely anxious or depressed | 5 (21.7%) | 0 (0%) |
FI is a complex disorder with variable symptoms which may be difficult to quantify. Neuromodulation is a simple, safe, and minimally invasive procedure with low morbidity and excellent results12,13 for appropriate indications. The results appear to be maintained for 6 years after the procedure, significantly improving FI and the quality of life, even when there is a sphincter defect or pudendal nerve neuropathy.14
The results of a recent Spanish cost-effectiveness study show that neuromodulation is a highly efficient measure for treating FI,15 which has been corroborated by other European cohort studies.16,17
The impact of incontinence (with its different types and degrees of severity) on the quality of life18 and the changes experienced by patients after treatment have begun to be measured objectively only in recent years, using generic and specific questionnaires.
Our study measured the influence of FI on HRQoL using EQ-5D for its proven ability to detect changes in the quality of life of patients8,9 and for being simpler to apply than other specific questionnaires, such as FIQL. However, its inability to detect specific problems of this condition is a disadvantage. Significant improvement with neuromodulation was found in the five dimensions studied in our cohort of patients, although this was statistically significant only for the patient's mobility, and decrease in anxiety and/or depression due to FI. The higher sensitivity of these dimensions in detecting the improvement experienced by patients after treatment may be related to the difficulty that patients have in travelling outside their home, with the risk of having an incontinence episode, more than due to the difficulty in mobility itself.
In addition, 57.9% of patients reported an improvement in health with the neurostimulator. We believe that the lack of statistical significance in the improvement for self-care, usual activities and presence of pain and/or discomfort was due to the small size of the cohort. We believe that a more extensive cohort would provide statistically significant improvements for the other three EQ-5D dimensions measured.
As with other studies, no significant relationship between ultrasound and manometric findings and HRQoL results was found.10
The small sample size meant that the study could be considered as a preliminary one and was a limitation of the study. Another limitation was the failure to associate a specific incontinence test to study the association of symptoms with the generic quality test EQ-5D and neuromodulation therapy.
In conclusion, the use of a validated HRQoL test is a simple and useful tool to evaluate the effectiveness of treating FI with neuromodulation, which improves the quality of life for patients with FI. Our cohort showed an improvement for the five dimensions studied after treatment, although only those related to mobility and anxiety/depression were statistically significant. We believe, therefore, that neuromodulation is an effective technique for improving the quality of life and perceived health benefits in patients with faecal incontinence.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please, cite this article as: Soria-Aledo V, et al. Mejora de la calidad de vida en los pacientes con incontinencia fecal tratados con estimulación de raíces sacras. Cir Esp. 2011;89:581–7.