Peutz-Jeghers syndrome (PJS) is a rare autosomal dominant disease with an estimated prevalence of 1:100,000 births.1,2 It is characterized by pigmentation of the skin and mucosa and multiple hamartomatous polyps in the gastrointestinal tract.3 The average age of presentation is usually between 11 and 13 years of age, and approximately, half of the patients will experience symptoms before the age of 20.2 Although most polyps are usually jejunal, they can also be found in the ileum, stomach, duodenum, and colon. Intussusception or bleeding are often complications associated with the presence of polyps4.
Intussusception cases occur more frequently in the pediatric population, mainly in the first 6 years of life, with a percentage of 73% of intussusception from any cause, while in those over 18 years this percentage drops to 23%.
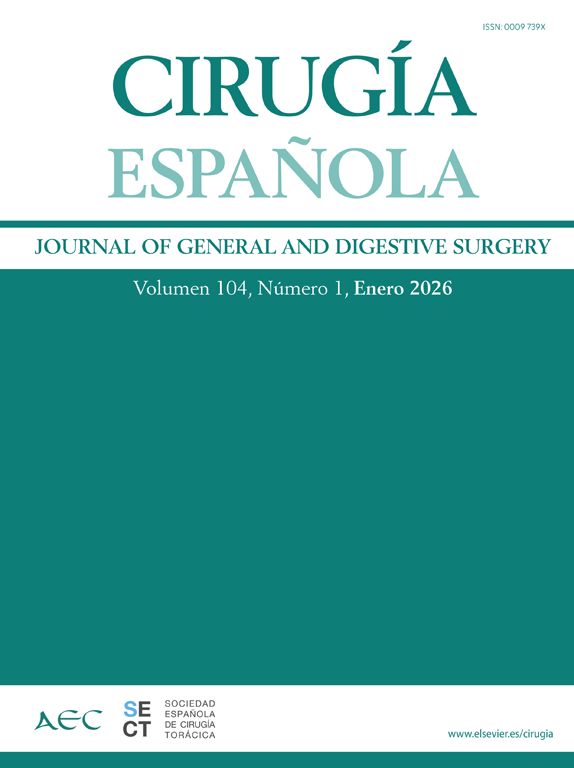
We present the case of a 44-year-old woman with a history of PJS that is admitted to the Emergency Room with signs of intestinal occlusion. As background she referred two laparotomies in early childhood with extensive intestinal resections due to intussusception, living however a normal life without intestinal failure; and a recent hospitalization 30 days prior to admission in our Hospital for intestinal occlusion, where she underwent exploratory laparotomy and surgical reduction of the intussuscepted intestine. The patient was discharged but continued with oral intolerance and abdominal pain, so she was referred to our institution. She was admitted with moderate intensity intermittent abdominal pain and vomiting, hemodynamically stable. There were no alterations in the laboratory. A computed tomography (CT) showed two small bowel intussusceptions. The longest one, projected in the lower right quadrant, involved the ileum and generated moderate distention of proximal small bowel; and the other one, shorter in length, projects into the epigastrium involving the jejunum. A moderate free fluid is associated. No vascular compromise was found (Fig. 1).
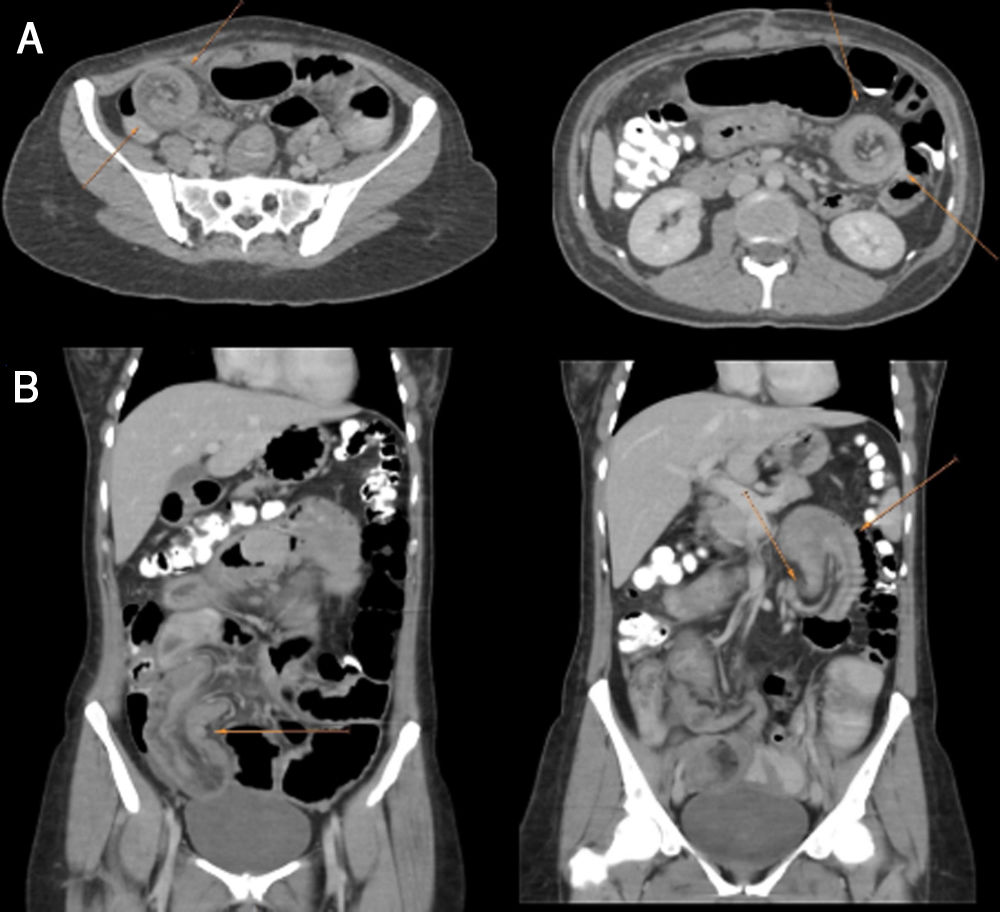
Due to the prior history of extensive intestinal resections and the appearance by CT of short small bowel and both intussusceptions showing intestinal polyps as lead point, an hybrid approach is decided (surgical and endoscopic) to treat the cause while preserving intestinal length. An exploratory laparotomy was performed, and revision of the small bowel showed two intussuscepted bowel segments: one close to the Treitz angle (proximal) and another close to the ileocecal valve (distal) (Fig. 2A and B) with intestinal dilation proximal to the occlusion site. Both intussusceptions are manually desinvaginated. New revision of the small bowel shows approximately 1 meter total of intestine from the Treitz angle to the ileocecal valve. A hand-assisted intraoperative enteroscopy is performed at the same time, in which several polyps of different sizes are observed. In the proximal and distal invagination sites, polyps larger than 4 centimeters are encountered, which are resected with a mucosectomy technique (Fig. 2C and D). A total of 8 polyps were resected. The anatomopathological study reveals hamartomatous polyps, confirming the PJS. The postoperative was uneventful and the patient was discharged on the thirteenth day postoperatively due to the need to correct prior nutritional deficit. The patient evolved favorably in the postoperative controls and had no recurrente to date.
Intussusception cases are rare in adult life, and those reported by PJS represent 7% of total intussusception, being less than 1% in the adult population.5 Surveillance of these patients includes endoscopies of the upper and lower gastrointestinal tract to treat accessible polyps, but there is no consensus on the use of enteroscopy on a routine basis. In more than half of the cases, the diagnosis of intussusception is preoperative, but this may depend on the availability of diagnostic methods such as Computed Tomography.
Regarding the surgical approach, the vast majority of the series agree that laparotomy is the route of choice. However, there are reports of pneumatic and hydraulic reduction in the case of colonic intussusception,6 as well as endoscopic reduction of ileocolonic intussusceptions.7 Regarding the intraoperative decision of resection or reduction, certain factors should be taken into account, such as: the site and etiology of the intestinal invagination, and history of previous intestinal resections. In small bowel intussusceptions, since they are mostly benign lesions, manual reduction is feasible in patients without signs of intestinal ischemia or suspicion of malignancy, to avoid resection of a large intestinal segment.8 In these cases, it is convenient to associate the resection of the lesion that acts as lead point of invagination to avoid recurrence.9 Two modalities have been described for the treatment of hamartomatous polyps in the small intestine: intraoperative enteroscopy, which consists of a combination of the endoscopic and surgical approaches, either laparotomy or laparoscopy, by means of which the endoscope is manually assisted to resect the polyps10,11; and double balloon enteroscopy, which allows the enteroscope to be progressed in the distal intestine without the formation of loops.2 It is noteworthy that these patients often have repeated episodes, and in order to avoid a short bowel syndrome a non-resective approach should be considered. Such is the case of the presented patient, with previous extensive intestinal resections, and a recent laparotomy with manual reduction of invagination, in which we decided to reduce the intussuscepted segment but associating also the resection of the polyps by enteroscopy with a mucosectomy technique, to treat the invagination cause.
As a conclusion, intestinal intussusception in the adult patient with PJS is extremely rare. However, when treating patients who generally have multiple bowel resections, approaches that allow preservation of the small intestine and in turn treat the cause are of paramount importance. The hybrid approach using manual reduction and enteroscopic polypectomy is a viable option for this type of case. These patients should be referred to high volume centers with trained surgeons and endoscopists.
Informed consentInformed patient consent was obtained for case publication.
Financial supportNone.
Conflict of interestsNone.