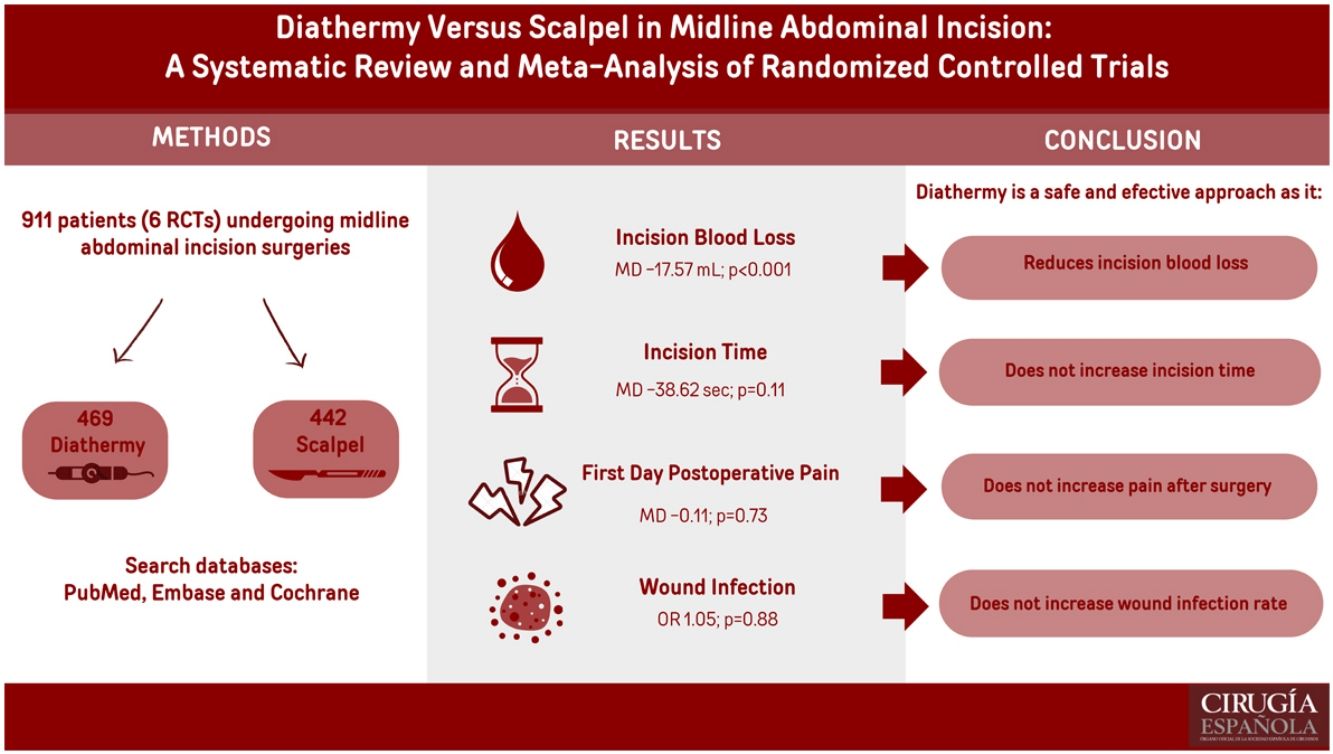
Our study aimed to compare the midline abdominal incision with scalpel and diathermy.
MethodsPubMed, EMBASE, and Cochrane were searched through January 2024 following PRISMA guidelines (PROSPERO, ID: CRD42024516771), and only randomized controlled trials were included. Heterogeneity was assessed using Cochran's Q test and the I2 heterogeneity index. Statistical analysis was performed using Review Manager 5.4 software.
ResultsSix randomized controlled trials were included, from which 469 patients (51.5%) received diathermy incision and 442 patients (48.5%) underwent the scalpel technique. Patients treated with the electrocautery approach had less incision blood loss (MD −17.57 mL; P < .01). No statistically significant differences were found between groups regarding wound infection incidence, incision time, incision area or first-day postoperative pain.
ConclusionDiathermy use in midline abdominal incision may be advocated as it demonstrated a significant reduction in incision-related blood loss, with no differences in wound infection or early postoperative pain incidences compared to the scalpel.
Nuestro estudio tuvo como objetivo comparar la incisión abdominal en línea media con diatermia y bisturí frío.
MétodosSe realizaron búsquedas en PubMed, EMBASE y Cochrane hasta enero de 2024 siguiendo la Guía PRISMA (PROSPERO, ID: CRD42024516771) y solo se incluyeron ensayos clínicos aleatorizados. La heterogeneidad se evaluó mediante la prueba Q de Cochran y el índice de heterogeneidad I2. El análisis estadístico se realizó utilizando el software Review Manager 5.4.
ResultadosSe incluyeron seis ensayos clínicos aleatorizados, de los cuales 469 pacientes (51,5%) recibieron incisión con diatermia y 442 pacientes (48,5%) recibieron incisión con bisturí frío. Los pacientes operados con electrocauterio tuvieron menor pérdida de sangre relacionada con la incisión (DM -17,57 ml; p < 0,01). No se encontraron diferencias estadísticamente significativas entre los grupos con respecto a la incidencia de infección de la herida, el tiempo o el área de la incisión o el dolor postoperatorio en el primer día.
ConclusiónSe puede recomendar el uso de la diatermia en la incisión abdominal en línea media, ya que demostró una reducción estadísticamente significativa en la pérdida de sangre relacionada con la incisión, sin diferencias en la infección de la herida o la incidencia de dolor postoperatorio temprano en comparación con el bisturí frío.
Laparotomy, also called celiotomy, can be performed through different types of incisions. The midline approach along the linea alba provides rapid access and great exposure of structures, being widely used for various pathology sites at multiple surgical centers.1,2
Traditionally, skin incisions in abdominal surgical procedures have been made with a scalpel. This surgical tool typically causes less damage to the surrounding tissue ad provides a precise incision, in addition to controlled incision depth.3,4 On the other hand, electrocautery has been increasingly adopted as an alternative for cutting tissue. It manipulates electrons through an alternating current, generating heat and causing tissue cell destruction.4 Electrocautery is commonly used for dissecting subcutaneous tissue, muscle and fascial layers, as well as for intraoperative hemostasis.4 Despite its advantages, there are concerns regarding its potential for causing excessive burning and scarring, as well as its increased potential for bacteremia.4–7 Results from previous trials suggest that diathermy may be a beneficial alternative for midline laparotomy in terms of incision time and blood loss.8
Since the publication of a prior meta-analysis9 evaluating the role of electrosurgery on incision execution, subsequent studies have been published, including randomized controlled trials (RCT). Furthermore, the aforementioned meta-analysis focused on several types of abdominal skin incisions, although not specifically midline incisions. Additionally, despite a few studies comparing these 2 methods of abdominal surgical access, there is no consensus regarding the safety and efficacy concerning wound healing and intraoperative parameters when using electrocautery for skin incisions. Therefore, we aimed to conduct a systematic review and meta-analysis to compare cold scalpel versus diathermy for midline abdominal incisions.
MethodsThis meta-analysis was registered in the international prospective register of systematic reviews (PROSPERO) under protocol CRD42024516771. The study was designed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines.10
Study eligibilityThe inclusion criteria for this meta-analysis were: (1) RCT, that (2) included patients undergoing surgeries with midline abdominal incision, and (3) compared diathermy to cold scalpel. We excluded studies that: (1) were nonrandomized; (2) did not have an intervention or control group; (3) had overlapping populations; (4) patients did not have a midline incision; or (4) reported no outcomes of interest. In addition, there were no restrictions concerning the date of publication or language.
Search strategy and data extractionWe systematically searched PubMed, Embase and Cochrane databases through January 2024 with the following search strategy: (scalpel OR scalpels) AND (diathermy OR diathermies OR cautery OR cauterization OR cauterizations OR electrocautery) AND ("midline incision" OR "midline incisions" OR "midline wound" OR "midline wounds" OR "midline laparotomy" OR "midline laparotomies" OR abdominal). Article selection and data extraction were done independently by 2 authors (NSP and JMO), whose disagreements were resolved by consensus.
EndpointsData from appropriate studies were independently collected by 2 researchers (NSP and RCC) and organized on spreadsheets. The following information was extracted from eligible studies, including: 1) study characteristics — authors, journal, study design, location, groups sample size, follow-up, time frame, and outcomes available; 2) patient characteristics — age and male sex; 3) outcomes — incisional blood loss was the primary outcome, while secondary outcomes of interest were incision time, incision area, postoperative pain, and wound infection.
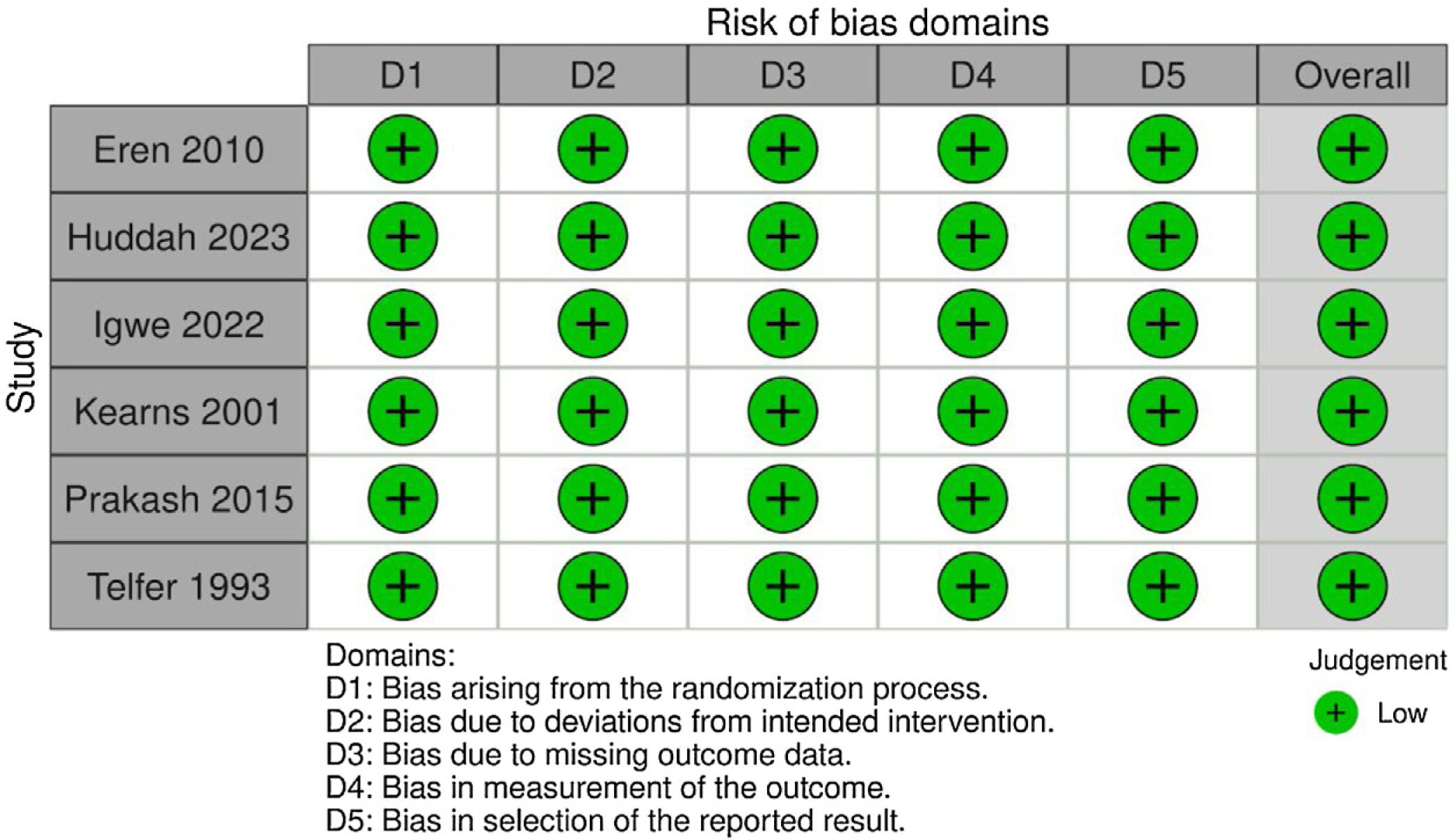
Quality assessment and publication biasThe Cochrane Collaboration tool for assessing risk of bias in randomized trials (RoB 2) was used to assess the quality of individual RCT.11 Two independent authors (NSP and ACFFS) conducted the quality assessment, and disagreements were resolved through a consensus after discussing reasons for discrepancy. Each trial received a score of high, low, or unclear risk of bias in five domains: randomization process; deviations from the intended interventions; missing outcomes; measurement of the outcome; and selection of reported results. The layout was generated using the robvis tool.12 Potential publication bias was assessed through visual inspection of funnel plots and analysis of the control lines.
Statistical analysisWe used the Cochrane Review Manager Software (RevMan 5.4; Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark) to perform the statistical analysis.19 The binary endpoints for treatment effects were compared using odds ratio (OR) with 95% confidence intervals (CI). Cochran Q test and I2 statistics were used to assess for heterogeneity; P values inferior to 0.10 and Higgins and Thompson’s I2 values up to 25% were considered significant for heterogeneity. We applied a DerSimonian and Laird random-effect model for outcomes with significant heterogeneity. Otherwise, a fixed-effect model was used.
Sensitivity analysisWe performed a leave-one-out sensitivity analysis for the primary outcome to evaluate the robustness of the result. Overall, there was no change in incision blood loss significance with the removal of each individual study in this subanalysis. R software version 4.3.0 (R Foundation for Statistical Computing) was used for sensitivity statistical analysis performance.
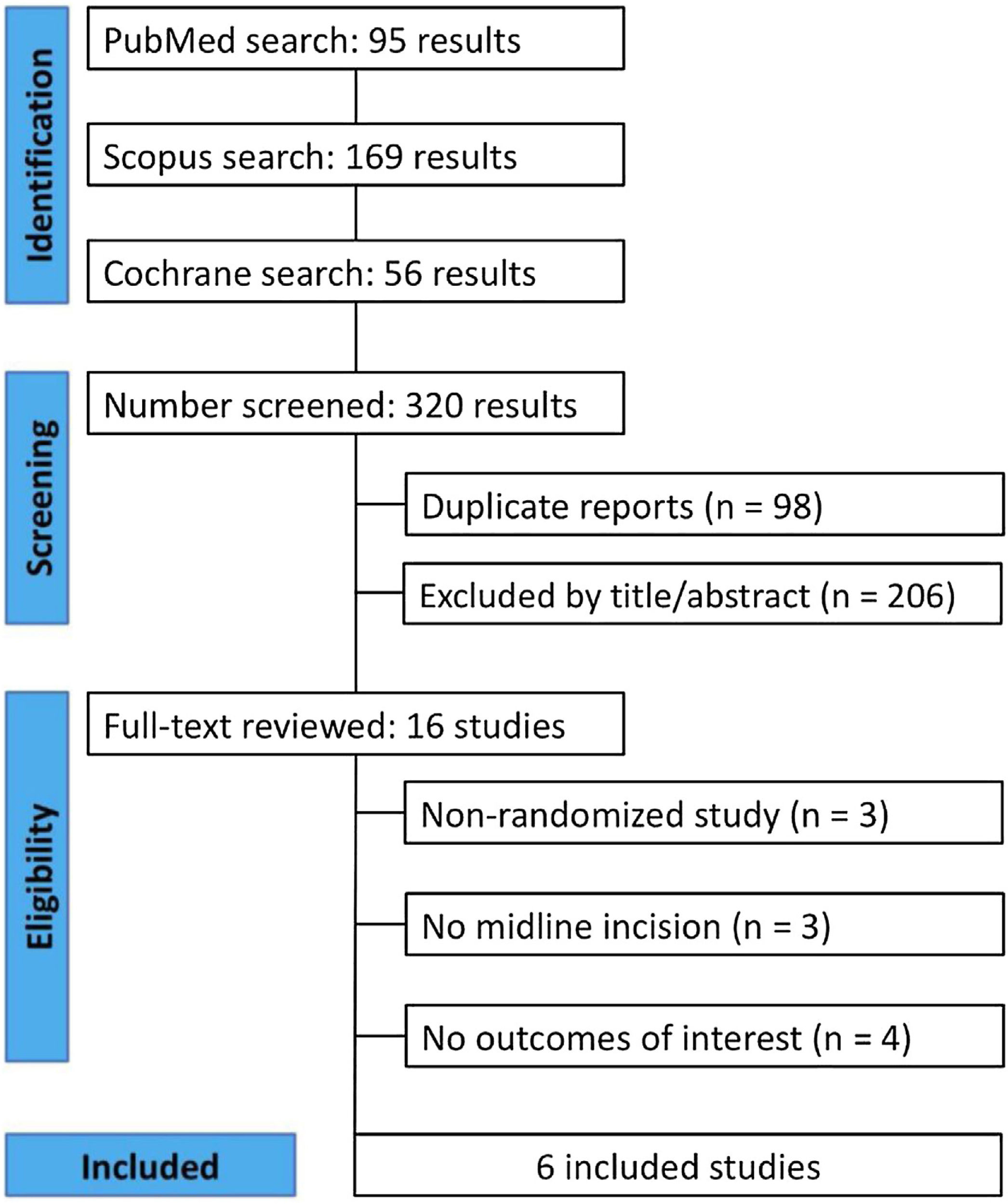
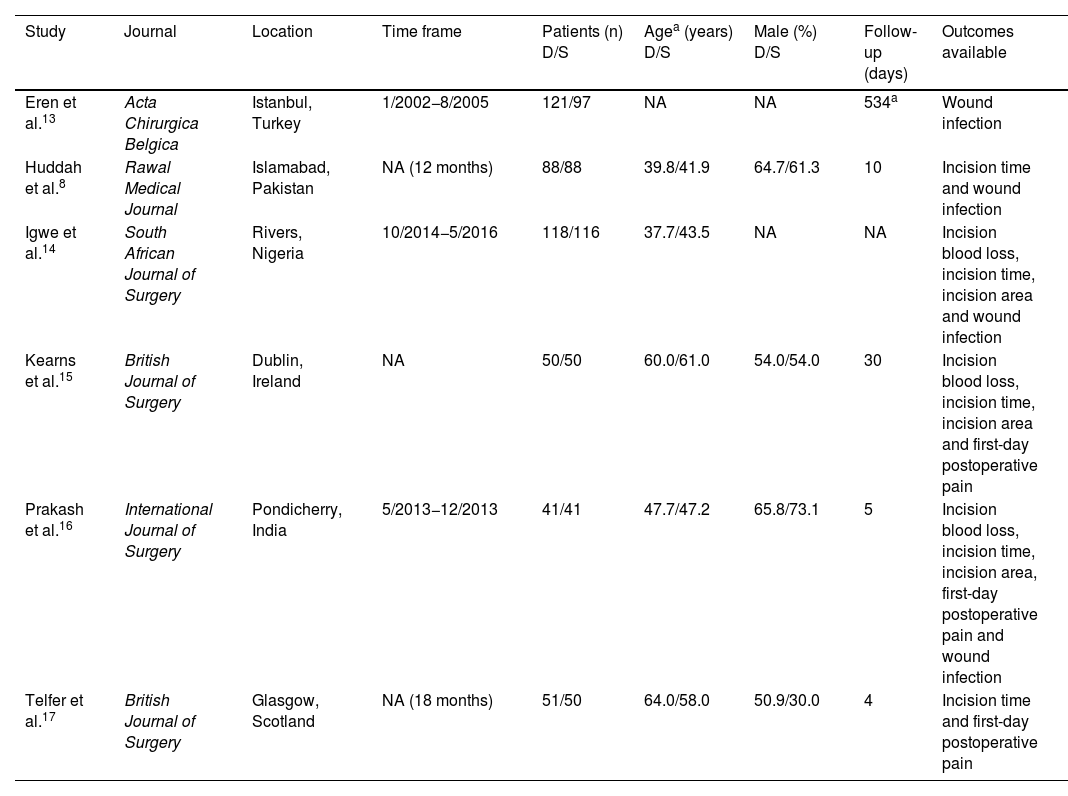
ResultsStudy selection and characteristicsAs detailed in Fig. 1, the initial search yielded 320 results. Duplicate records and ineligible studies were excluded, including those that lacked randomization, abdominal surgeries with non-midline incisions, and those missing at least one outcome of interest. After that, 16 studies remained and were fully reviewed based on inclusion criteria. Among these, a total of 6 studies were included, comprising 911 patients from 6 RCT. A total of 469 (51.5%) patients received a diathermy incision, while 442 (48.5%) had a scalpel incision. Mean patient age ranged from 37.7 to 64 years, and the proportion of males ranged from 30.0% to 64.7%. Significant inter-study variability existed in terms of follow-up periods, which ranged 4–534 days. Study baseline characteristics are reported in Table 1.
Baseline characteristics of the studies included.
| Study | Journal | Location | Time frame | Patients (n) D/S | Agea (years) D/S | Male (%) D/S | Follow-up (days) | Outcomes available |
|---|---|---|---|---|---|---|---|---|
| Eren et al.13 | Acta Chirurgica Belgica | Istanbul, Turkey | 1/2002−8/2005 | 121/97 | NA | NA | 534a | Wound infection |
| Huddah et al.8 | Rawal Medical Journal | Islamabad, Pakistan | NA (12 months) | 88/88 | 39.8/41.9 | 64.7/61.3 | 10 | Incision time and wound infection |
| Igwe et al.14 | South African Journal of Surgery | Rivers, Nigeria | 10/2014−5/2016 | 118/116 | 37.7/43.5 | NA | NA | Incision blood loss, incision time, incision area and wound infection |
| Kearns et al.15 | British Journal of Surgery | Dublin, Ireland | NA | 50/50 | 60.0/61.0 | 54.0/54.0 | 30 | Incision blood loss, incision time, incision area and first-day postoperative pain |
| Prakash et al.16 | International Journal of Surgery | Pondicherry, India | 5/2013−12/2013 | 41/41 | 47.7/47.2 | 65.8/73.1 | 5 | Incision blood loss, incision time, incision area, first-day postoperative pain and wound infection |
| Telfer et al.17 | British Journal of Surgery | Glasgow, Scotland | NA (18 months) | 51/50 | 64.0/58.0 | 50.9/30.0 | 4 | Incision time and first-day postoperative pain |
D: diathermy; NA: not available; S: scalpel.
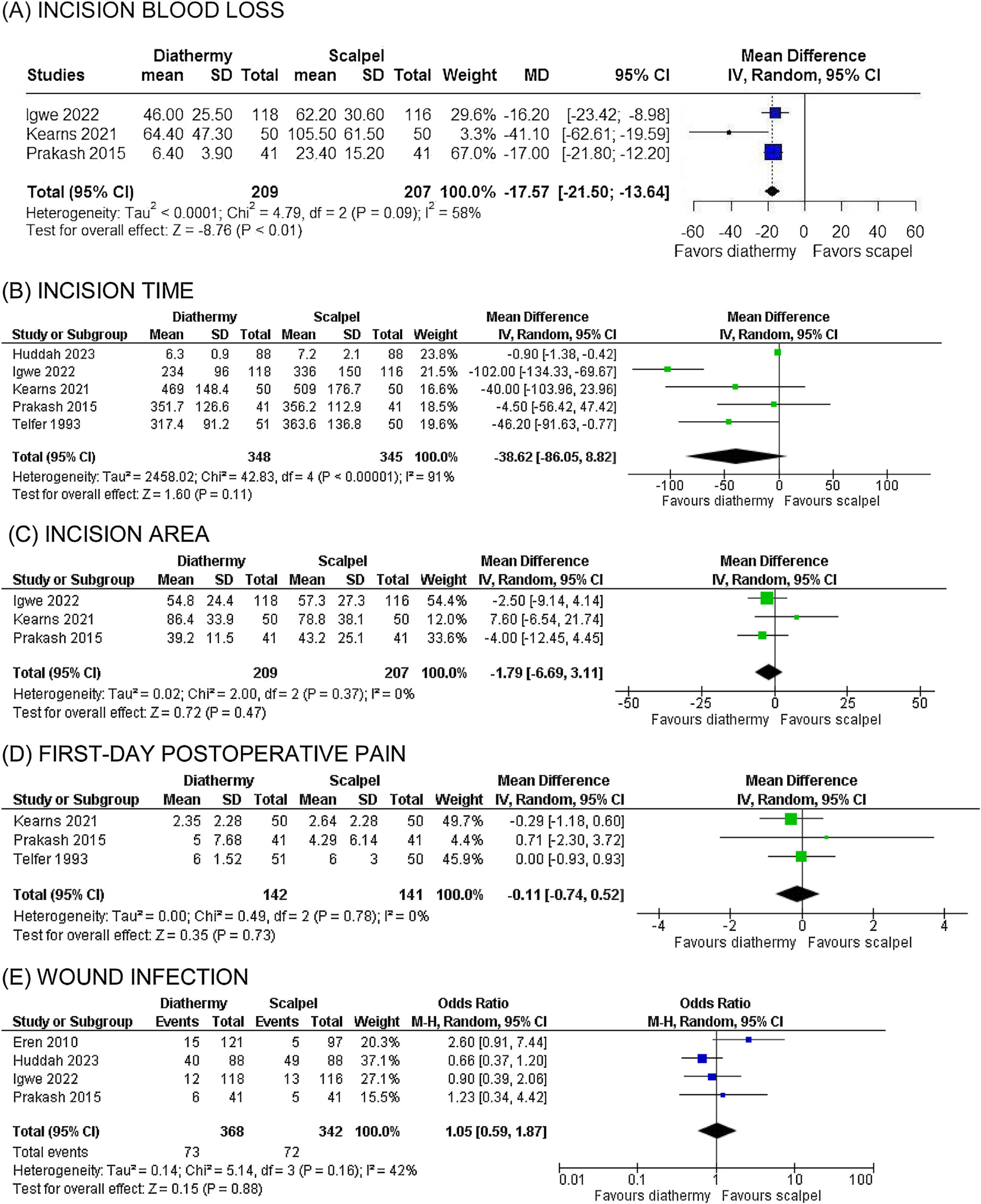
Blood volume loss during the incision process was significantly lower in the diathermy group compared to the control group (3 studies; MD −17.57 mL; CI 95% −21.50 to −13.64; I2 = 0.58; P < 10−3; Fig. 2A). There was no statistically significant difference between the electrocautery and scalpel groups regarding incision time (5 studies; MD −38.62 s; CI 95% −86.05, 8.82; I2 = 0.91; P = .11; Fig. 2B), incision area (3 studies; MD −1.79; CI 95% −6.69, 3.11; I2 = 0; P = .47; Fig. 2C), first-day postoperative pain (3 studies; MD −0.11; CI 95% −0.74, 0.52; I2 = 0; P = .73; Fig. 2D), and wound infection incidence (4 studies; OR 1.05; CI 95% 0.59, 1.87; I2 = 0.42; P = .88; Fig. 2E).
Bias assessmentWe evaluated 6 RCT using the RoB2 tool, and all the articles demonstrated a low risk of bias across all assessed domains. Individual RCT appraisals are reported in the RoB2 traffic light diagram (Fig. 3).
According to the GRADE assessment,18 2 outcomes evaluated in this study were classified as high-quality evidence: incision area and wound infection. Two outcomes had moderate quality of evidence (incision blood loss and incision time) due to high heterogeneity. The main domain responsible for reducing the quality of evidence of the outcomes was the inconsistency of results because of heterogeneity (Supplementary Fig. 1).
Additionally, the funnel plot for incision blood loss demonstrates an asymmetrical distribution of studies with different weights, suggesting evidence of publication bias (Supplementary Fig. 3). No quantitative assessment of small studies or publication bias was attempted because the number of studies included in the meta-analyses was lower than ten.10
DiscussionIn this systematic review and meta-analysis of 6 RCT including 911 patients, diathermy was compared with the scalpel in midline abdominal incisions. Electrocautery incision demonstrated a significant decrease in incision blood loss. No statistically significant differences were found between the 2 approaches regarding incision time, incision area, postoperative pain within the first 24 h, and wound infection rate.
The intervention effectiveness in incision blood loss remains controversial, as, to the best of our knowledge, no previous meta-analyses had analyzed its performance specifically in midline abdominal incisions.9 One review found no significant difference in blood loss when comparing cold scalpel to electrocautery for incisions in various procedures.4 In contrast, one meta-analysis20 concluded that diathermy incisions decrease incision-related blood loss in open inguinal hernia repair. Our meta-analysis supports this finding, demonstrating that diathermy promotes a significant reduction in incision blood loss volume. This reduction can be attributed to the interrupted, slower current output of cutting diathermy, which creates a safe incision mechanism and effectively limits blood flow through the cutting area.21 Additionally, the intrinsic hemostatic effect of electrosurgery may contribute to the controlled blood volume.22 Regardless of our findings about statistically significant decrease in incision blood loss, its clinical relevance may not be so relevant, since the reduction in bleeding was only 17.57 mL. When analyzing these results, it is also crucial to consider the existence of differences among studies when estimating incisional blood loss. For instance, Igwe et al. used a gravimetric method, while Kearns et al. and Prakash et al. weighed the gauze swabs.14–16
Concerns have been raised regarding the potential heat damage or impaired wound healing caused by electrocautery, which could increase the risk of secondary wound infection.23 However, the high-density current at the tip of the diathermy forceps, combined with its small size, results in a large production of heat at the tip. Meanwhile, the large surface area at the patient's surgical site prevents heat production due to lower current density.24 Our analysis revealed no significant difference in wound infection rates between scalpel and diathermy approaches, consistent with the findings of a prospective study comparing cold scalpel with electrocautery in tension-free inguinal hernioplasty.25 Although the consistency of our results with the existing literature was previously mentioned, the lack of information about the method of measurement for wound infection used by Huddah et al. and the visual incision grade applied by Prakash et al. may be considered inaccurate when compared to the wound cultures taken in Eren et al. and Igwe et al.8,13,14,16 Additionally, despite the appearance of infectious symptoms typically within 3–7 days after surgery, by definition it must be set 30–90 days following the procedure.26 Therefore, wound infection rates should be interpreted by considering the variation in follow-up among different studies, including the absence of follow-up information or insufficient duration.8,14,16
Although existing evidence suggests that incision time is protracted in scalpel incisions,9,21 our meta-analysis found no difference in time to incision when comparing diathermy and scalpel. Individually, all included studies that reported this outcome found a time decrease with diathermy.13–17 This finding may be attributed to the instrument exchanges required to achieve hemostasis with cold scalpel incision, which can be overcome by using cutting electrocautery.21 Additionally, incision time shown by Huddah et al.13 in both groups was discrepant when compared to other studies, which is most likely to be attributed to the depth of incision considered to account for cutting time.
Previous meta-analyses focusing on various abdominal incisions or non-abdominal incisions reported a significant reduction in postoperative pain associated with diathermy incisions.4,9 However, the analysis by Aird et al. exhibited less consistency due to variations in measurement methods. Nonetheless, despite these limitations, these findings may be elucidated by the ability of electrocautery to destruct cutaneous nerves at the incision site.11 Specifically concerning midline abdominal incisions, only 3 studies15–17 reported a pain score in the first 24 h after surgery using a visual analogue scale. Prakash et al.16 and Telfer et al.17 found no difference in the postoperative pain score on the first day, unlike Kearns et al., who found pain benefits when using diathermy. However, our meta-analysis, which focused spe1cifically on midline abdominal incisions, found no significant difference in postoperative pain scores within the first 24 h. This finding may be explained by the typically more painful nature of midline abdominal incisions,17 which could outweigh any pain-reducing benefits of electrocautery observed in other incision locations.5,9
To interpret the findings of our study, it is essential to consider its limitations. Firstly, moderate to high heterogeneity was observed in certain outcomes, such as incision blood loss. Nonetheless, we mitigated this concern by performing leave-one-out sensitivity analyses, which consistently yielded reliable results even after excluding individual studies from the analysis. Secondly, the absence of patient-level data impeded the ability to guarantee little variance and heterogeneity between each study group's sample, despite its randomized nature, as well as to perform subgroup analyses on primary and secondary endpoints. Thirdly, while this study presents the largest pooled analysis of patients undergoing midline abdominal incision surgeries with diathermy, its statistical power remains underpowered for examination of long-term cosmetic endpoints. Moreover, while it is crucial to analyze the results pertaining to pain scores due to their clinical significance, the subjective nature of this endpoint poses a challenge for consistent measurement across different patients. Likewise, the diverse methods used to quantify incisional blood loss, wound infection variables and follow-up must be taken into account when analyzing the limitations of our meta-analysis. Additionally, given the inclusion of fewer than 10 studies in the meta-analysis, the potential for reporting bias cannot be overlooked.
ConclusionIn conclusion, this meta-analysis suggests that the use of diathermy in midline incisions decreases incision-related blood loss. No significant differences between the 2 approaches were found in terms of incision time, incision area, postoperative pain within the first 24 h and wound infection. These findings suggest that diathermy may be a safe and effective alternative to the scalpel for midline abdominal incisions, particularly in terms of reducing incision-related blood loss.
Funding sourcesThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of interestAll authors report no relationships that could be considered conflicts of interest; all authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Data sharing statementArticle includes all data and is accompanied by a supplementary file, making the information readily available to readers. Additional questions can be directed to the corresponding author.
Ethics approvalNot applicable.
CRediT authorship contribution statementNicole dos Santos Pimenta: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Writing – original draft, Writing – review & editing. Ana Clara Felix de Farias Santos: Data curation, Software, Validation, Visualization. João Pedro Costa Esteves Almuinha Salles: Visualization, Writing – original draft, Writing – review & editing. Juliana Millani de Oliveira: Conceptualization, Visualization. Pedro Henrique Costa Matos da Silva: Writing – original draft. Renan Carlo Colombari: Methodology, Project administration, Supervision, Writing – review & editing.