The closure of a temporary stoma involves 2 different surgical procedures: the stoma reversal procedure and the abdominal wall reconstruction of the stoma site. The management of the abdominal wall has different areas that should be analyzed such us how to avoid surgical site infection (SSI), the technique to be used in case of a concomitant hernia at the stoma site or to prevent an incisional hernia in the future, how to deal with the incision when the stoma reversal procedure is performed by laparoscopy and how to close the skin at the stoma site. The aim of this paper is to analyze these aspects in relation to abdominal wall reconstruction during a stoma reversal procedure.
Revertir un estoma temporal implica 2 procedimientos quirúrgicos diferentes: la reconstrucción del tránsito intestinal y el cierre de la pared abdominal en el sitio del estoma. Este último presenta diferentes aspectos que deben ser analizados: a) la infección del sitio quirúrgico (ISQ), b) el manejo de una hernia coincidente en el sitio del estoma en el momento de su cierre, c) la prevención del desarrollo de una hernia incisional posterior, d) el cierre del estoma en el caso de que se realice la reconstrucción del tránsito por vía laparoscópica, o e) el cierre de la piel del sitio del estoma. El objetivo de este trabajo es analizar estos aspectos en relación con la reconstrucción de la pared abdominal por la que emerge un estoma temporal cuando se procede al cierre de este.
The creation of a temporary ostomy is a surgical tool used to redirect intestinal contents away from a more distal problematic area or to avoid an anastomosis.1 Temporary ostomies can be considered both our “friend” as well as our “enemy”.2 The former is because of the advantages its use provides in certain situations,2 while the latter is due to the morbidities that can arise from its presence3 and the negative impact on patient quality of life4 (in 20%–40%, the ostomy will never be reversed).1,5–7 A temporary ostomy is probably only truly beneficial if the morbidity and mortality involved in its closure are minimal.1
The objective of this paper is to exclusively analyze the problems related with the closure of the abdominal wall through which the ostomy is constructed during closure.
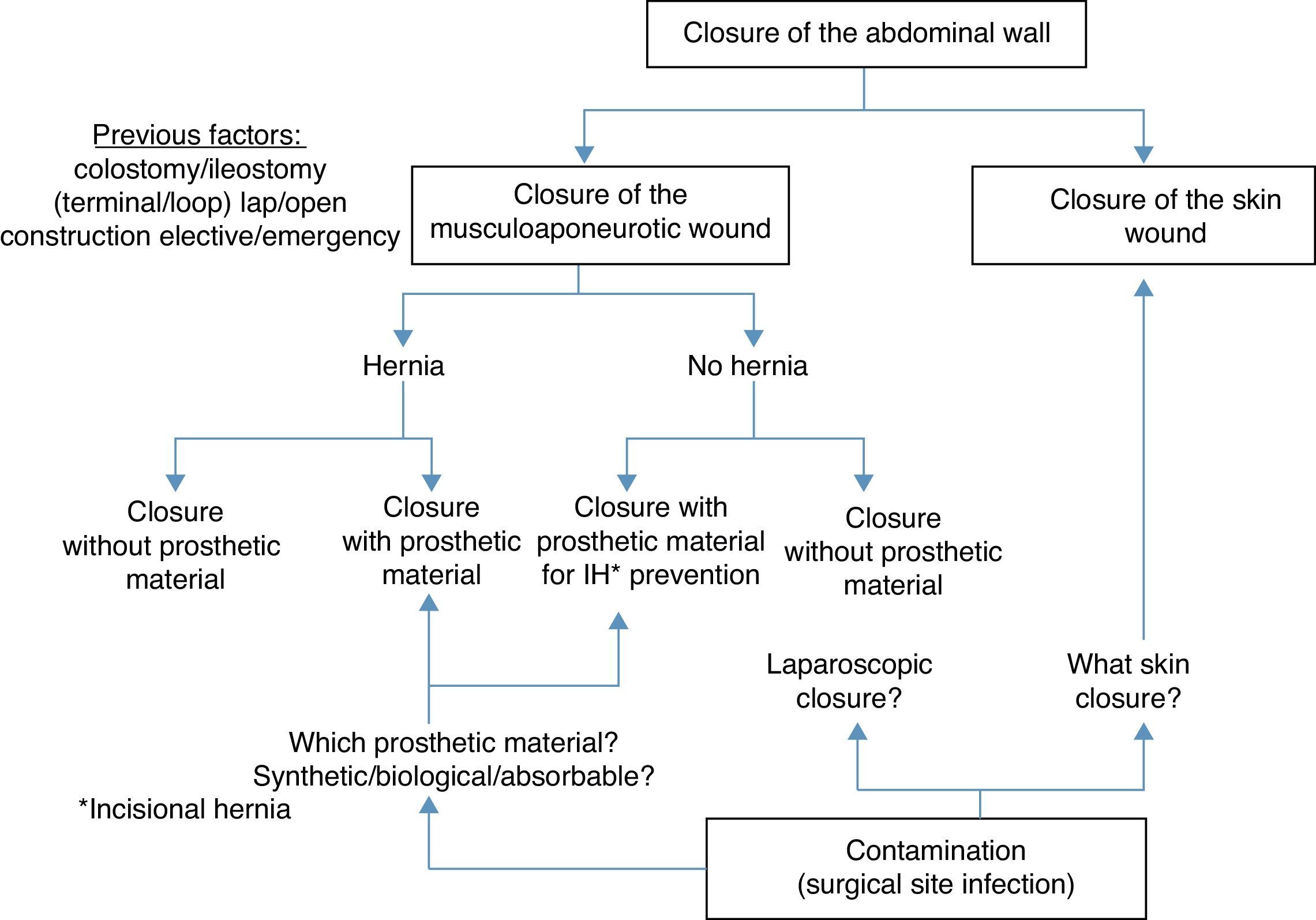
Points for AnalysisThe abdominal wall is made up of the skin, aponeurosis, muscle and peritoneum.8 For this reason, when closing a stoma it is necessary to treat a skin wound and a musculoaponeurotic wound. The musculoaponeurotic wound can present a concomitant parastomal hernia or be the origin of a later incisional hernia. Thus, prosthetic material may be used during the closure of the wound (either to treat or prevent a hernia). In addition, closure of the abdominal wall of a temporary ostomy is associated with bacterial contamination because the intestine is open and there is therefore a greater risk of surgical site infection (SSI) (Fig. 1).
In this context and in our opinion, 5 points should be considered:
- 1.
SSI in the closure of a temporary stoma
- 2.
The presence of a hernia at the time of stoma closure: how to close the musculoaponeurotic wound?
- 3.
The absence of a hernia at the time of stoma closure: should we prevent the appearance of a later incisional hernia?
- 4.
The advantages of laparoscopic closure of the stoma
- 5.
Closure of the skin at the stoma site
SSI is reported as being the most frequent complication after the closure of a temporary stoma9 with an incidence that ranges between 2% and 40%.10–12 This variability in incidence may be related with under-reported percentages, the analysis of different types of temporary ostomies (different wound management protocols) or the use of data collection designs that are not homogenous enough to detect such events. One of the largest and most recent patient series published9 shows an SSI incidence after temporary stoma reversal of 20%–30%, with the following associated risk factors: (1) morbid obesity (thickness of subcutaneous fat greater than 25mm in the region of the navel); (2) the temporary stoma is a colostomy (SSI 5 times more frequent than in the case of ileostomy); or (3) the temporary stoma was created as an emergency procedure (persistence of “sleeping” bacteria at the surgical site). In addition, this same study9 shows that the gram-positive microorganisms (basically enterococci and methicillin-resistant Staphylococcus aureus) can play a determinant role in SSI after the closure of a temporary stoma, representing 70% of the bacteria isolated on culture. According to these authors, abdominal wall closure after temporary stoma reversal can be an inherently different procedure from colon and rectal surgery since the colonization of the skin and intestine can be completely different.
Presence of a Hernia at the Time of a Stoma Closure: How to Close the Musculofascial Wound?Incisional hernias are more frequently reported in association with colostomies (63%)13 than with ileostomies (20%–30%).14,15 It is interesting to observe how, in one of the largest published series about SSI and temporary stoma closure, the presence of a concomitant hernia was indicated as a risk factor for SSI.9 Basically, this was seen in patients who were treated with the placement of synthetic mesh. The authors explained that it is a procedure that has additional dissection and entails longer surgical times. This increased risk of SSI related with the use of prosthetic material has also been reported by other authors.16 Thus, these groups9,16 recommend not reinforcing the hernia repair with synthetic material when closing a temporary stoma.
On the other hand, the use of synthetic prostheses for the treatment of a hernia in contaminated and potentially contaminated areas is currently under debate.17,18 Some studies justify their use in these situations.19–24 These studies defend and argue in favor of hernia repair with synthetic mesh during the closure of a temporary ostomy. An alternative for avoiding the uncertainty of using synthetic material could be the use of biological prostheses; however, more evidence of the functional and long-term results are needed to determine in which situations and patients these expensive materials could be justified.25,26 In our opinion, more data are required about repairing associated hernias with mesh during temporary ostomy reversal. In this context of limited available evidence, the surgical technique to be used for the abdominal wall closure will depend on individual clinical experience27 and factors such as surgeon preference or the clinical scenario in particular (type of patient, associated risk factors for SSI, etc.).
Absence of a Hernia at the Time of the Stoma Closure: Should Measures be Taken to Prevent the Appearance of an Incisional Hernia?The literature suggests that the incidence of incisional hernias at the closure site of a temporary stoma can be high.16,28–32 In a recent systematic review and meta-analysis on this subject,33 a percentage of 35% was observed when clinical and radiological evaluations were combined. For this reason, it has been suggested16,28–33 that the closure of the musculoaponeurotic defect after the closure of a temporary ostomy should be reinforced by adding a prosthetic material. Nonetheless, the utility of reinforcement in these situations has not been sufficiently studied (probably due to the risk of associated SSI), which poses problems similar to those mentioned in the previous section. It could be argued in these cases that absorbable synthetic prosthetic material could be used,34 but unfortunately there are no supporting clinical data. At the writing of this paper, we have found only two related studies. The first, which is currently in the development stage and whose final objective is a randomized study (Reinforcement of Closure of Stoma Site [ROCSS]),35,36 will evaluate a biological prosthetic material (dermis porcina) in the prevention of incisional hernias at the closure site of temporary ostomies. The second is a retrospective study which concludes that the placement of synthetic prosthetic material reduces the later appearance of incisional hernias at the stoma site.37 Once again, and until more evidence appears, the implementation of preventive prosthetic material will depend on the surgeon's better judgment and the characteristics of the clinical scenario.
Advantages of Laparoscopic Stoma ClosureIn the era of minimally invasive surgery, some authors have associated advantages with the use of the laparoscopic approach for closure of temporary stomas38: faster postoperative recovery, shorter hospital stay, vision of the entire abdominal cavity, avoiding the re-opening of previous laparotomies, lower rate of reoperations due to intestinal obstruction or a reduction in SSI rate.
The mentioned advantages have been confirmed both for the closure of temporary ileostomies39–41 as well as the closure of temporary colostomies (i.e. Hartmann's procedure).42–45 Unfortunately, the majority of these published studies are characterized by two factors: (a) they mostly analyze the aspects related with the surgical technique for re-establishing intestinal continuity; and (b) practically no consideration is given to the aspects of abdominal wall closure and the problems that may arise. Only one author46 makes an anecdotal mention that the laparoscopic approach is able to: (a) allow for exact dissection along the line joining the abdominal wall and intestinal loop; (b) avoid excessive dissection and resection of musculoaponeurotic tissue; and (c) minimize the damage caused by the use of electrocautery. The result of all these advantages would be the existence of less tension in the wall closure, with no vascular compromise along the edges of the musculoaponeurotic wound.46 In this previous context, it is tempting to speculate that some general beneficial aspects, especially the reduction in SSI rate, may favor different wall closure strategies (placement of synthetic prosthetic material). However, it seems evident that more studies are needed to clarify the actual impact of the laparoscopic approach in the closure of the abdominal wall at the stoma site.
Closure of the Skin at the Stoma SiteSeveral options have been described for skin closure in these circumstances. Some authors propose leaving it open, allowing the skin wound to heal by secondary intention (granulation) and thus diminishing the risk for SSI.47,48 On the other hand, primary closure has also been proposed, describing different variations (“air-tight” primary closure, “loose” primary closure or “delayed” primary closure), which provides for rapid healing but can be associated at the same time with a greater incidence of SSI.48 Last of all, a hybrid closure combining the two previously mentioned options can be carried out by closing the skin with a “purse-string” suture.49
Comparisons have been made among the different options (especially the last 2),50 and the purse-string suture has been shown to be a good alternative to primary closure in terms of lower rate of SSI. In a recent systematic review and meta-analysis,51 the authors conclude that the approximation technique with a purse-string suture was associated with a reduction of 80% in SSI, with no negative impact on hospital stay or long-term cosmetic results.
SummaryThe closure of a temporary stoma is sometimes perceived as minor surgery.46 In our opinion, it is not a minor procedure at all. The surgical technique for the closure of a temporary stoma raises 2 concerns that are different although closely related. On the one hand is the reconstruction of the intestinal transit with its potential problems.1 On the other is the closure of the abdominal wall with certain particularities that may give rise to complex therapeutic situations (both for decision-making as well as in the immediate and long-term results of those decisions).
Minimizing the risk of SSI is a key aspect in the closure of the abdominal wall at the site of a temporary ostomy. It is therefore important to analyze the previous surgical characteristics (type of temporary stoma, emergency or not). In addition, it may be of interest to implement a weight loss program prior to stoma reversal and to even consider avoiding closure in morbidly obese patients. As closing the wall can be a procedure that is inherently different from colon and rectal surgery, using antibiotics that cover gram-positive bacteria in the preoperative prophylaxis can be beneficial.
When an associated hernia appears at the site of the temporary stoma, it may be logical to think that the best solution is standard hernia treatment (application of prosthetic material). However, the evidence in this regard is not solid and more data are needed. The incidence rates of associated hernias (63% for colostomies and 20%–30% for ileostomies) merit urgent attention in clinical research to determine the best possible treatment.
Furthermore, the incidence of incisional hernias at the site of a previous temporary stoma can reach 35%. Likewise, one-third of patients who undergo stoma reversal could require later abdominal wall surgery. Currently, there is an important lack of data and attention given to the complexity of potential “future” hernias and what they may mean in terms of morbidity and mortality. Studies are necessary (preferably randomized) to define the efficacy of prophylactic prosthetic materials and to determine which type of material is best. The same reasoning could be applied to the influence of the laparoscopic approach in wall closures at temporary stoma sites. The closure of the skin in these patients seems better when using an approximation with a “purse-string” suture.
Finally, answering the many specific questions regarding abdominal wall closure at a temporary stoma site combines aspects from different highly specialized areas. We therefore believe that cooperation is essential amongst the surgeons involved in the creation and reconstruction of the stoma (mostly surgeons specialized in colon and rectal surgery) and surgeons specialized in abdominal wall surgery.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: López-Cano M, Pereira JA, Villanueva B, Vallribera F, Espin E, Armengol Carrasco M, et al. Cierre de la pared abdominal después del cierre de un estoma temporal. Cir Esp. 2014;92(6):387–392.