Traditionally, full sternotomy (FS) has been the gold standard for cardiac myxoma resection, however, in the last decade, minimally invasive surgery has become an attractive surgical alternative. The objective of this study is to compare the postoperative results of cardiac myxoma resection by minithoracotomy (MT) versus standard FS in a national referral center.
MethodsFrom January 2010 to December 2023, 85 patients with diagnosis of cardiac myxoma underwent surgery by FS or MT in our hospital. We compared perioperative and follow-up mortality and major complications, and other clinical variables.
ResultsWe compared 65 patients who underwent FS versus 20 who underwent MT for cardiac myxoma excision, all cases with histopathological confirmation. Mortality at 30 days was 1/65 (1.5%) for FS versus 0/20 (0%) for MT (p:0.58). The cardiopulmonary bypass (CPB) time (73min IQR: 53–86 vs 65.5 IQR: 59–72, p: 0.18) were similar, but aortic cross clamp (ACC) time (51min IQR: 26–67 vs 30.5 IQR: 24–35.5, p: 0.02) was shorter in MT. Patients underwent MT had less intraoperative (420ml IQR: 360–500 vs 275 IQR: 200–475, p<0.01) and postoperative bleeding (400ml IQR: 350–460 vs 220 IQR: 185–275, p<0.01) than those who underwent FS. The intensive care unit (ICU) stay was significantly shorter in MT group (3 days, IQR: 2–3 versus 2 days IQR: 1–2, p<0.01).
ConclusionsMT for cardiac myxoma excision is a safe procedure and it has less intraoperative and postoperative bleeding compared to FS, as well as fewer days of ICU stay.
Tradicionalmente, la esternotomía media ha sido el estándar de oro para la resección de mixoma cardíaco; sin embargo, en la última década, la cirugía mínimamente invasiva se ha convertido en una alternativa quirúrgica atractiva. El objetivo de este estudio es comparar los resultados postoperatorios de la resección de mixoma cardíaco mediante minitoracotomía (MT) frente a la esternotomía (ET) en un centro de referencia nacional.
MétodosDe enero de 2010 a diciembre de 2023, 85 pacientes con diagnóstico de mixoma cardíaco fueron sometidos a cirugía mediante ET o MT en nuestro hospital. Se compararon la mortalidad perioperatoria y el seguimiento, así como las complicaciones mayores y otras variables clínicas.
ResultadosSe compararon 65 pacientes sometidos a ET frente a 20 sometidos a MT para la escisión de mixoma cardíaco. Todos los casos fueron confirmados con histopatología. La mortalidad a los 30 días fue de 1/65 (1,5%) para ET frente a 0/20 (0%) para MT (p: 0,58). El tiempo de circulación extracorpórea (73min RIC: 53-86 frente a 65,5min RIC: 59-72; p: 0,18) fue similar, pero el tiempo de pinzamiento aórtico (51min RIC: 26-67 frente a 30,5min RIC: 24-35,5; p: 0,02) fue menor en la MT. Los pacientes sometidos a MT presentaron menor sangrado intraoperatorio (420ml RIC: 360-500 frente a 275 RIC: 200-475; p<0,01) y postoperatorio (400ml RIC: 350-460 frente a 220 RIC: 185-275; p<0,01) que los sometidos a ET. La estancia en la unidad de cuidados intensivos fue significativamente menor en el grupo de MT (3 días, RIC: 2-3 frente a 2 días RIC: 1-2; p<0,01).
ConclusionesLa MT para la escisión de mixoma cardíaco es un procedimiento seguro, y presenta menor sangrado intraoperatorio y postoperatorio en comparación con la ET, así como menos días de estancia en la UCI.
Cardiac myxoma is the most common primary cardiac tumor (estimated incidence of 0.03% in general population), it is generally located in the left atrium, it is more common in women, and tumor excision usually offers a cure.1,2 Traditionally, full sternotomy (FS) has been the standard approach; however, in recent decades, minimally invasive approaches to surgically access cardiac pathology have had constant growth and surgery for myxoma excision has been no exception. Minimal access offers faster recovery, less pain and better esthetic acceptance.3–7
Latin America has some of the most persistent health inequalities in the world.8 Peru has a fragmented and often inefficient health system; in this context, the development of new surgical techniques that involve the use of advanced technology is not always possible.9,10 However, our hospital is a national reference center in cardiovascular pathology for social security patients, and for more than a decade we have implemented a mini-invasive cardiac surgery program.11 In this context, this paper presents the postoperative results of patients underwent minimally invasive surgery for the excision of cardiac myxoma.
MethodsStudy design and populationWe carried out a retrospective study between January 2010 to December 2023 in patients underwent cardiac tumors excision in the National Cardiovascular Institute, EsSalud, Lima, Peru. Patients with histological confirmation of myxoma after surgery were included and others were excluded. All cases included in our series demonstrated calretinin expression in tumor cells (immunohistochemistry).
Surgical techniqueAll surgeries were performed during cardioplegic arrest on CPB and underwent intraoperative transesophageal echocardiography in addition to standard monitoring for cardiac surgery.
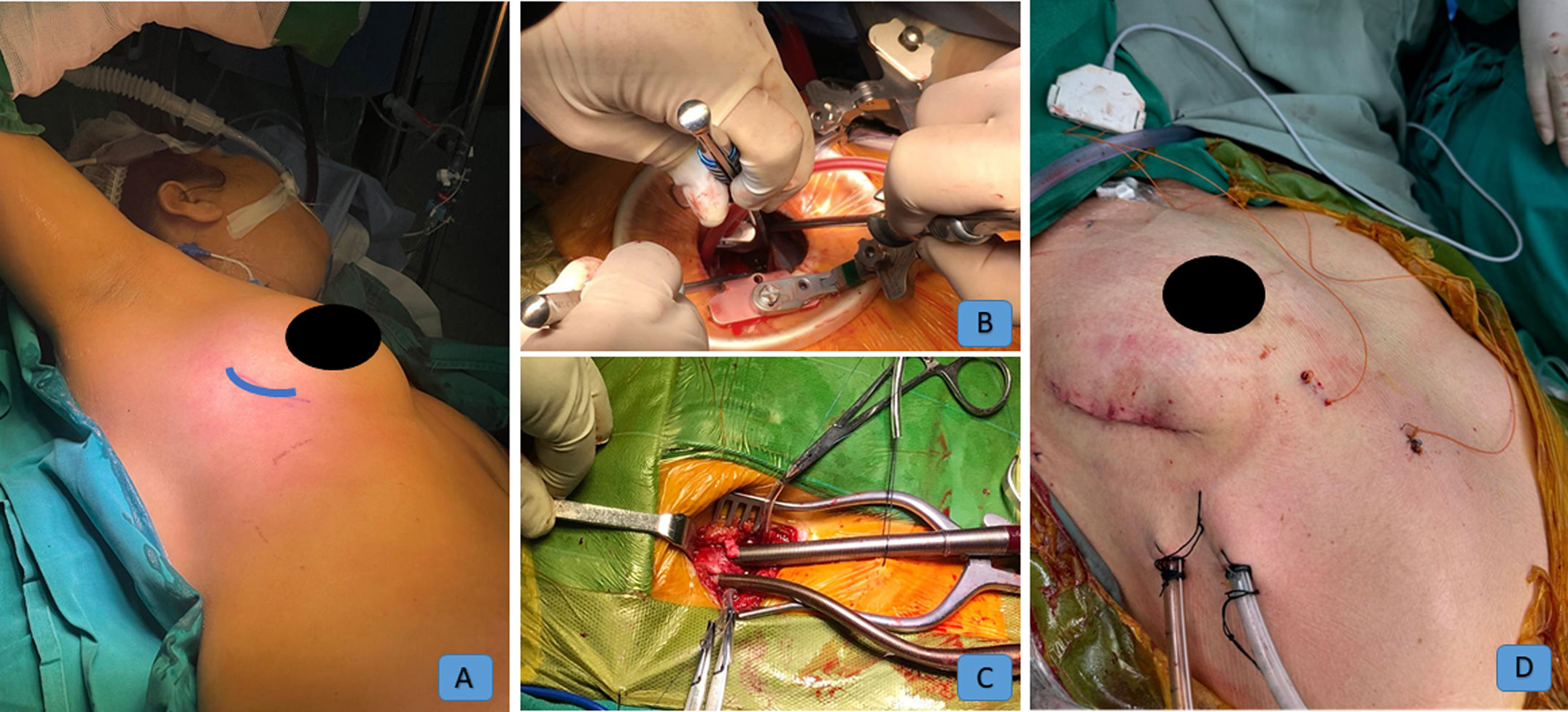
MT. We included two approaches, anterior and axillar minithoracotomy. The first 12 cases of MT were performed via anterior access and recently we have used the axillary approach. In both accesses through a 6–8cm incision we opened the four or five intercostal space and for CPB right femoral artery and vein were cannulated (in our hospital we do not have percutaneous closure devices, so direct cannulation was performed), and when it was necessary to open the right atrium, jugular percutaneous cannulation or direct cannulation of the superior vena cava was used (Fig. 1). For ACC, the transcutaneous Chitwood clamp was used, placed in the second intercostal space and anterior axillary line. Endotracheal intubation in our first cases was with a double-lumen tube, but in the last 15 cases with a single-lumen tube. In 5 patients we used video-assistance (video-assisted MT). The drain was removed when output was <100ml in 12h.
FS. In this approach, we opened the sternum from the fork to the xiphoidal appendix, the cannulation strategy was the classic one, ascending aorta for arterial perfusion and atrio-caval or bicaval for venous drainage.
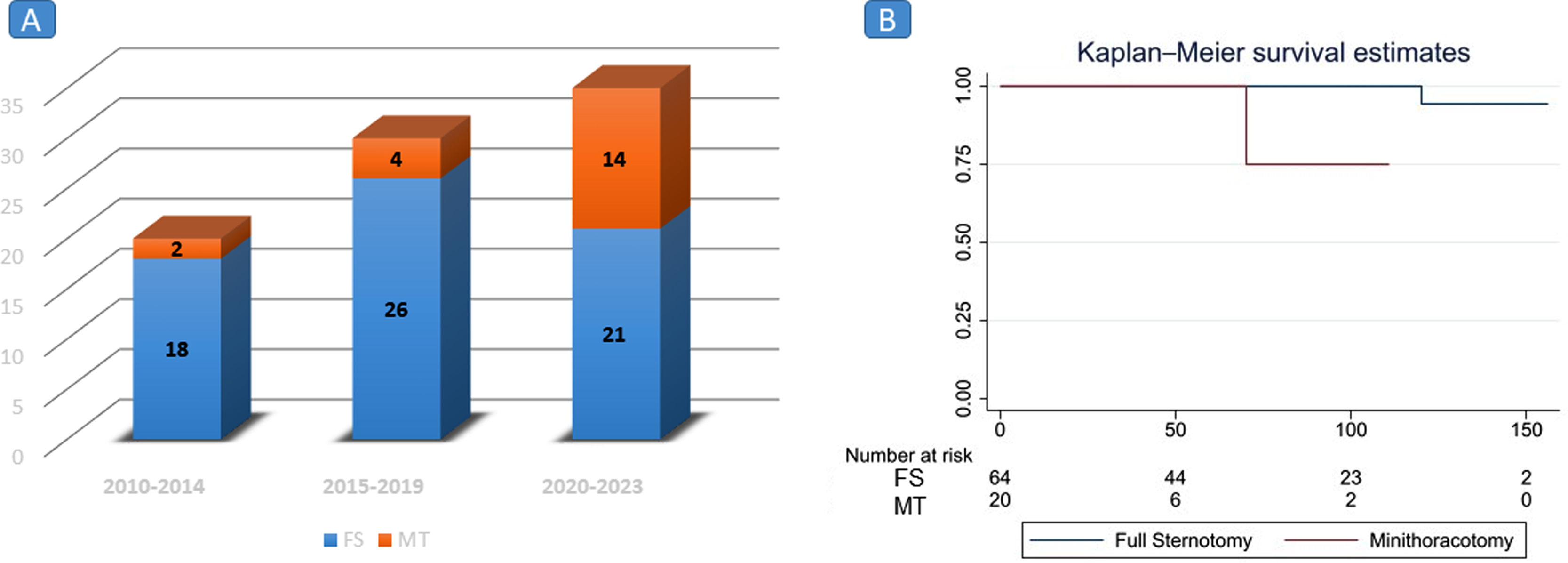
The minimally invasive surgery program began at our hospital in 2010, mitral valve and atrial septal defect surgeries were our first procedures; however, aortic valve, ascending aorta, and atrial tumor surgeries have subsequently been performed. As can be seen in Fig. 2A, the frequency of atrial myxoma resection has been performed mainly in the last five years. Only three surgeons perform minimally invasive cardiac surgeries in our hospital; however, atrial tumor surgeries are performed by the entire surgical staff (10 in total). The surgical approach (FS o MT) was chosen by the surgeon assigned to the surgery.
Clinical endpointsWe define three time periods. Baseline: from hospital admission to before the surgical procedure. Perioperative period: until first 30 postoperative days. Extended follow-up: after 30 postoperative days until a median follow-up of 80 months for FS and 68 months for MT.
The primary clinical endpoints were safety measured through major complications (mortality, perioperative myocardial infarction, stroke and permanent atrioventricular block (ABV)). The secondary clinical outcomes were intra and postoperative bleeding, ICU stay, new onset atrial fibrillation (AF), redo for bleeding, mediastinitis, superficial surgical site infection and tumor recurrence.
Statistical analysisDescriptive analysisWe explored the distribution of variables using analytical and graphical methods and reported numerical data as mean and standard deviation or as median and interquartile ranges (IQR). The categorical variables were presented as absolute and relative frequencies. For complications we estimate the cumulative incidence.
Comparative analysisWe performed the comparative analysis between MT and FS in perioperative period and follow. For numerical data we used t-test or Mann–Whitney depending on normality and x2-test for categorical variables. We used Kaplan–Meier method for survival estimates. Statistical non-significance in some hypothesis tests (e.g. in associated procedures) could be due to a small sample size which may suppose a low statistical power and random error, this can lead to errors of interpretation.
EthicsThe Institutional Research and Ethics Committee approved the protocol of this study. All patients signed informant consent according to health care hospital regulations.
ResultsBaseline characteristicsIn Table 1 we present baseline characteristics. 65 patients underwent FS and 20 MT. The age of the patients was similar in both groups (FS: 55.42±15.3 and MT: 57.9±14.5 years), the majority of patients were women (72% and 60%, respectively). Dyspnea was the principal clinical manifestation (75%) in both groups, followed by stroke and syncope. The left atrium was the most frequent location of the myxoma. (FS: 76.9%, MT: 75%).
Baseline characteristics.
| Full sternotomy(n=65) | Mini-thoracotomy(n=20) | p value | |
|---|---|---|---|
| Age (years) mean (SD) | 55.42 (15.3) | 57.9 (14.5) | 0.52a |
| Women n(%) | 47 (72) | 12 (60) | 0.2b |
| Risk factors n(%) | |||
| Hypertension | 16 (24.6) | 5 (25) | 0.97b |
| Diabetes | 6 (9.2) | 0 (0) | 0.16b |
| Clinical presentation n(%) | |||
| Asymptomatic | 5 (7.7) | 2 (10) | 0.74b |
| Dyspnea NYHA II | 21 (32.3) | 9 (45) | 0.29b |
| Dyspnea NYHA III | 27 (41.5) | 5 (25) | 0.18b |
| Dyspnea NYHA IV | 1 (1.5) | 1 (5) | 0.37b |
| Atrial Fibrillation | 6 (9.2) | 3 (15) | 0.46b |
| Angina | 8 (12.3) | 3 (15) | 0.75b |
| Stroke | 12 (18.5) | 5 (25) | 0.52b |
| Syncope | 7 (10.8) | 5 (25) | 0.11b |
| Echocardiography | |||
| LVEF(%) mean (SD) | 59.58 (7.57) | 61.6 (7.53) | 0.30c |
| RVLFS mean (SD) | 47.65 (6.66) | 49.2 (7.19) | 0.37c |
| SMR n (%) | 5 (7.7) | 0 (0) | 0.2b |
| STR n (%) | 5 (7.7) | 1 (5) | 0.68b |
| Localization n (%) | |||
| Left atrium | 50 (76.9) | 15 (75) | 0.86b |
| Right atrium | 8 (12.3) | 2 (10) | 0.78b |
| Both atrium | 2 (3.1) | 0 (0) | 0.43b |
| Left ventricle | 2 (3.1) | 1 (5) | 0.68b |
| Right ventricle | 3 (4.6) | 2 (10) | 0.37b |
| STS score median (IQR) | 0.89 (0.77–1.37) | 0.915 (0.70–1.2) | 0.47c |
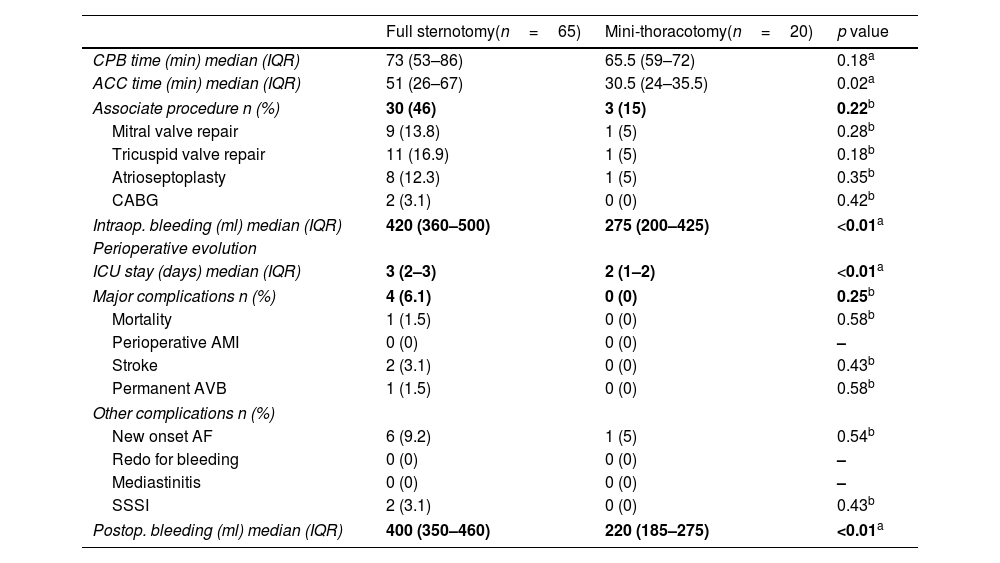
Table 2 shows the results in perioperative period. There was not difference in CPB for both group, but ACC (FS: 51min IQR: 26–66, MT: 30.5min IQR: 24–35.5, p: 0.02). However, in the FS group we performed more associated procedures (46% compared to 15%), despite the fact that the statistical difference was not significant (due to the size of the sample), more associated procedures were performed through FS and this explains the longest CPB and ACC times in this approach. The most common associate procedure was mitral or tricuspid repair. The STS score was similar in both MT and FS.
Perioperative period.
| Full sternotomy(n=65) | Mini-thoracotomy(n=20) | p value | |
|---|---|---|---|
| CPB time (min) median (IQR) | 73 (53–86) | 65.5 (59–72) | 0.18a |
| ACC time (min) median (IQR) | 51 (26–67) | 30.5 (24–35.5) | 0.02a |
| Associate procedure n (%) | 30 (46) | 3 (15) | 0.22b |
| Mitral valve repair | 9 (13.8) | 1 (5) | 0.28b |
| Tricuspid valve repair | 11 (16.9) | 1 (5) | 0.18b |
| Atrioseptoplasty | 8 (12.3) | 1 (5) | 0.35b |
| CABG | 2 (3.1) | 0 (0) | 0.42b |
| Intraop. bleeding (ml) median (IQR) | 420 (360–500) | 275 (200–425) | <0.01a |
| Perioperative evolution | |||
| ICU stay (days) median (IQR) | 3 (2–3) | 2 (1–2) | <0.01a |
| Major complications n (%) | 4 (6.1) | 0 (0) | 0.25b |
| Mortality | 1 (1.5) | 0 (0) | 0.58b |
| Perioperative AMI | 0 (0) | 0 (0) | – |
| Stroke | 2 (3.1) | 0 (0) | 0.43b |
| Permanent AVB | 1 (1.5) | 0 (0) | 0.58b |
| Other complications n (%) | |||
| New onset AF | 6 (9.2) | 1 (5) | 0.54b |
| Redo for bleeding | 0 (0) | 0 (0) | – |
| Mediastinitis | 0 (0) | 0 (0) | – |
| SSSI | 2 (3.1) | 0 (0) | 0.43b |
| Postop. bleeding (ml) median (IQR) | 400 (350–460) | 220 (185–275) | <0.01a |
Intraoperative bleeding was significantly lower in MT group (FS: 420ml IQR: 360–500, MT: 275ml IQR: 200–425, p<0.01). Similar results were observed in postoperative bleeding (FS: 400ml IQR: 350–46, MT: 275ml IQR: 185–275, p: <0.01).
The ICU stay was shorter in MT group (FS: 3days IQR: 2–3, MT: 2 days IQR: 1–2, p<0.01).
There was no difference in major complications at 30 days; however, one patient in the FS group died on the first postoperative day due to cardiogenic shock.
No redo for bleeding or mediastinitis was observed in both groups. 6 patients (9.2%) presented postoperative new onset AF in FS, but 1 (5%) in MT (p: 0.54).
Follow-upFollow-up was not uniform (Table 3). For FS was 80 months (IQR: 30–120) and for MT was 68 months (IQR 25–109), this difference can be explained because in the period 2010–2014 our mini-invasive surgery program had barely begun, and recently (2020–2023) more patients underwent MT (Fig. 2A).
Follow-up.
| Full sternotomy(n=65) | Mini-thoracotomy(n=20) | p value | |
|---|---|---|---|
| Follow up (months) median (IQR) | 80 (30–120) | 68 (25–109) | <0.01a |
| Major complications n(%) | 9 (13.8) | 1 (5) | 0.28b |
| All mortality | 2 (3.1) | 1 (5) | 0.68b |
| Stroke | 2 (3.1) | 0 (0) | 0.427b |
| Myocardial Infarction | 0 (0) | 0 (0) | – |
| Permanent Pacemaker | 1 (1.5) | 0 (0) | 0.58b |
| Recurrence | 4 (6.2) | 0 (0) | 0.25b |
One patient in FS group died for a hemorrhagic stroke 10 years after surgery, in addition to the patient who died in perioperative period (total mortality: 2/65, 3.1%). In MT group one patient died due to Covid-19 infection (total mortality 1/20, 5%). Kaplan–Meier survival estimates are shown in Fig. 2B.
In FS group, 4 (6.2%) patients developed recurrence that required re-operation (01 patient in the context of Carney syndrome), but none in MT group. The second operation to excise the recurrent myxoma was success performed through redo-sternotomy removing the entire interatrial septum (the site of recurrence) and replacing it with a bovine pericardial patch.
DiscussionIn our data, myxoma resection surgery was more frequent in women, both for FS and MT. Dyspnea was the main clinical manifestation and the left atrium was the preferred location. MT had shorter aortic cross time, but FS more associate procedures. Intraoperative/postoperative bleeding and ICU stay were significantly lower in MT group. There was no difference in mortality or major complications in both groups.
Ko et al. reported the first removal of myxoma through a right MT.5 Later, some studies of a few cases have been published comparing MT versus FS for myxoma surgery, this is because despite being the most common cardiac tumor, myxoma is a rare disease.6,7,12–14
In a recent publication, Shin et al. reported 64 patients underwent MT for myxoma excision without operative mortality.12 Ellouze et al. in a retrospective study to compare the clinical outcomes of 20 patients undergoing MT and 23 undergoing FS reported no mortality in both groups.6 Lee et al. compared 83 patients treated using FS and 63 patients treated using right MT, no early mortalities were recorded in either group. Similar results were reported for other authors.7,14,15 In our study no operative mortality was observed in MT group, but 01/65 (1.5%) in FS. The deceased patient underwent emergency surgery for refractory shock due to mitral valve obstruction, and died a few hours after surgery.
One of the risks of myxoma surgery is the possibility of embolism due to tumor mobilization. Regarding to this, we observed 2/65 (3.1%) post-operative stroke in FS group, but none in MT. Iribarne et al. reported postoperative stroke rates of up to 13% for FS approach and none for MT (p:0.044), others authors found similar stroke ratios between MT and FS.7,14
It has been established that minimally invasive cardiac surgery has lower bleeding rates, short hospital stays and rapid recovery of patients.3,4,16 In our data, the ICU stay was 1 day shorter in MT group (FS: 3days IQR: 2–3, MT: 2 days IQR: 1–2, p<0.01). Lee et al. found no significant differences in hospital stay, postoperative intubation time, or ICU stay; however, Iribarne et al. reported that the hospital stay was shorter in the MT group by 2.2 days (p 0.044), and Pineda et al. observed that the mean ICU and hospital stays were 27h (IQR 24–47) versus 60h (IQR 48–79; p<0.01) and 5 days (IQR 4–6) versus 7 days (IQR 6–8; p 0.03) for the MT and the FS group.7,13,14
In our research; although it is true, no patient required redo surgery for bleeding in both groups, patients underwent MT had less intraoperative (420ml IQR: 360–500 vs 275 IQR: 200–475, p<0.01) and postoperative bleeding (400ml IQR: 350–460 vs 220 IQR: 185–275, p<0.01) than those who underwent FS. Regarding to this, Ellouze et al. reported that operative blood loss (106ml±95 vs 338ml±270) was significantly less in the MT group, and Lee et al. found that 51% of patients underwent FS required blood transfusion versus 17% of patients underwent MT (p: 0.04).6,13
In our data CPB times were similar in both groups, but ACC time were shorter in the MT group. This difference in ACC time would be due to the fact that patients underwent FS had a higher frequency of procedures associated with myxoma resection; on the other hand, the technical level of the surgeons is not comparable, probably, the surgeons who performed the mini approach had more experience, which could act as a confounding factor. Other authors found that the CPB and ACC were significantly longer in patients undergoing myxoma resection by MT.7,13
We did not have recurrence in the patients in the MT group in a median of 68 months of follow-up. Although we present the experience of 20 cases of myxoma resection using minithoracotomy, we have demonstrated that the resection of benign cardiac tumors can be performed entirely using minimally invasive surgery. This is one of the highlights of our work. We also believe that the incorporation of video facilitates visualization of the implantation site. Results from other authors support this finding.7,13,14 In the FS group, 6.4% (04 patients) had recurrence, which is comparable to the series by Shah et al. (150 patients, rate of recurrence 5.6%).17 One of our patients had Carney syndrome and other patient had ventricular myxoma, some authors suggest these factors as a risk of recurrence.17 It is well established that complete endocardial resection from the free wall of the atrium or atrial septum (myxoma implantation base) is the recommended technique to avoid recurrence; this can be facilitated with the use of video in minimally invasive techniques.15,17
Although it is true that there are several published studies that show that minimally invasive surgery for the removal of cardiac myxoma is safe; it is nevertheless interesting in that it communicates how, in areas with disparities in access to resources and limited availability, a surgical program/technique can be implemented safely and even with outcomes comparable to other published series. This is one of the first studies in a middle-income country to describe successful outcomes of cardiac myxoma excision using minimally invasive techniques. In our country there are not always resources available for surgical innovation, and implementing a minimally invasive surgery program was a challenge.
ConclusionIn terms of mortality and major complications, both MT and FS are safe approaches for cardiac myxoma excision; However, MT has less intraoperative and postoperative bleeding and a shorter ICU stay. MT is a feasible approach for surgeries like myxoma resection and does not increase adverse outcomes compared to FS and without the risk of tumor recurrence.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Authors contribution statementJCRO: Conceptualization, Research, Data Collection, Writing, JSR: Conceptualization, Research, Data Collection. ZDC: Validation, Supervision. DEA: Conceptualization, Research, Data Collection. CAC: Conceptualization, Research, Data Collection. YPV: Conceptualization, Research. JMC: Conceptualization, Validation, Supervision.
FundingThis work was supported by self-financing.
Conflict of interestNone declared.
Data availability statementAuthors declare the availability of data.