Comprehensive care of the cardiosurgical patient is essential to optimize clinical results. In this context, preoperative strategies play a key role, with accelerated recovery programs (ERAS) being a promising alternative.
ObjectiveTo evaluate the psychological and metabolic effects of prolonged fasting (>8h) in patients undergoing elective cardiac surgery, comparing them with a group receiving carbohydrate supplementation.
MethodologyQuasi-experimental, prospective and randomized study. Patients were assigned to two groups: (1) Carbohydrate supplementation and (2) Prolonged fasting. Clinical variables, capillary blood glucose, anxiety (Hamilton Scale), feeling of hunger and thirst, perceived satisfaction and postoperative complications were measured.
Results58 patients were included. The intervention group presented a lower sensation of hunger and thirst (p<0.001), as well as a significant reduction in pre-surgical anxiety (p=0.003) compared to the control group. Perceived satisfaction was also higher in the intervention group (p=0.047). No significant differences were detected in capillary blood glucose levels between the groups. Neither was a greater need for insulin administration observed in either group. Regarding postoperative complications, no significant differences were observed, nor were there any cases of mortality attributable to the procedure.
ConclusionsPreoperative supplementation with carbohydrate-rich fluids improves the patient experience in terms of anxiety and comfort, without compromising metabolic stability or increasing the incidence of postoperative complications. The findings found throughout the research support the incorporation of this strategy into cardiac surgery protocols, with the potential to optimize patient experience and outcomes.
La atención integral del paciente cardioquirúrgico es fundamental para optimizar los resultados clínicos. En este contexto, las estrategias preoperatorias desempeñan un papel clave, siendo los programas de recuperación acelerada (ERAS) una alternativa prometedora.
ObjetivoEvaluar los efectos psicológicos y metabólicos del ayuno prolongado (>8 horas) en pacientes sometidos a cirugía cardíaca programada, comparándolos con un grupo que recibe suplementación con hidratos de carbono.
MetodologíaEstudio cuasiexperimental, prospectivo y aleatorizado. Los pacientes fueron asignados a dos grupos: 1) Suplementación con carbohidratos y 2) Ayuno prolongado. Se midieron variables clínicas, glucemia, ansiedad (Escala de Hamilton) y satisfacción percibida.
ResultadosSe incluyeron 58 pacientes. El grupo de intervención presentó menor sensación de hambre y sed (p<0.001), así como una reducción significativa de la ansiedad prequirúrgica (p=0.003) en comparación con el grupo control. La satisfacción percibida también fue mayor en el grupo de intervención (p=0,047). No se observaron diferencias significativas en las complicaciones postoperatorias.
ConclusionesLos hallazgos encontrados a lo largo de la investigación respaldan la incorporación de esta estrategia en los protocolos de cirugía cardíaca, con el potencial de optimizar la experiencia y los resultados del paciente.
Comprehensive and multidisciplinary patient-centered care is essential to prioritize the safety, well-being and clinical prognosis of cardiac surgery patients. In this context, the implementation of appropriate preoperative strategies plays a key role in optimizing the quality of care and reducing surgical complications. These strategies should focus on both the patient and their family environment, promoting an effective, efficient and safe care process.
Since the 1990s, Enhanced Recovery After Surgery (ERAS) programs in cardiovascular surgery have evolved significantly, encompassing all phases of the surgical process. Recent research1 highlights the benefits of comprehensive interventions during the perioperative period, such as patient education, optimization of nutritional status, and reduction of fasting time through the use of carbohydrate-rich solutions up to two hours before surgery.2 These are part of the ERAS protocols, which aim to mitigate surgical stress, accelerate postoperative recovery and improve clinical outcomes.3
ERAS protocols have been successfully implemented in a variety of surgical procedures, such as colorectal surgery, bariatric surgery and cardiac surgery.4 Studies have shown that the application of these protocols is associated with a significant reduction in hospital stay, postoperative complications and healthcare costs, without compromising patient safety.5 As evidence continues to support the benefits of ERAS protocols, their adoption has become increasingly widespread in the field of surgery.6
Prolonged preoperative fasting, a traditional practice in surgery, generates multiple adverse effects: catabolic stress, insulin resistance, metabolic alterations, muscle mass loss and immune deficiencies.7 These factors not only complicate recovery, but also increase the risk of postoperative complications. In contrast, strategies such as preoperative carbohydrate-rich fluid loading have demonstrated significant benefits, such as reduced insulin resistance, preservation of lean mass, and decreased symptoms of thirst, hunger and anxiety.8
The hypothesis is that supplementation with carbohydrate-rich fluids, compared to traditional prolonged fasting, significantly improves metabolic control, reduces anxiety, and optimizes the preoperative experience of the patient.
Overall objectiveTo evaluate the psychological and metabolic effects of prolonged fasting (>8h) in patients undergoing scheduled cardiac surgery, comparing these effects with those of a group of patients who receive a carbohydrate supplement.
Materials and methodsThis is a quasi-experimental, prospective and randomized study designed to evaluate the psychological effects of prolonged fasting in patients undergoing scheduled cardiac surgery. 68 adult patients were included in the tertiary care center, HUVA, in Murcia, Spain. Six patients scheduled for afternoon surgery were excluded from the study due to emergency surgery, two patients withdrew informed consent before the first nutritional intervention, one patient left the study due to postoperative acute confusional state, and one patient due to perioperative myocardial infarction, leaving a final 58 patients who completed the study.
Patients were randomly assigned to two groups: Intervention Group and Control Group. The Intervention Group received a supplementation with 400ml of a fast-absorbing carbohydrate-rich liquid solution (Sugarmix), administered in two moments: the night before surgery at 23:00 and on the day of surgery 3h before the procedure, at 12:00. The Control Group followed the traditional protocol of prolonged fasting (>8h) without receiving the supplementation.
The inclusion criteria were: patients over 18 years of age diagnosed with cardiac pathology (valve replacement or myocardial revascularization) scheduled for cardiac surgery in the afternoon shift. The exclusion criteria included: known intolerance to carbohydrates, hemodynamic instability due to urgent surgery, pregnant women, preoperative active infection, comorbidities affecting gastric emptying, morbid obesity, poorly controlled diabetes, and eating disorders.9
Measurements were performed at three key time points: Visit 1 (preoperative, the day before surgery), Visit 2 (day of surgery, before and after supplement administration) and Visit 3 (24h post-surgery, in the intensive care unit). At each visit, clinical variables, capillary glucose, anxiety using the Hamilton Anxiety Scale (HAM-A), and perceived satisfaction were evaluated.
The data were analyzed using the SPSS statistical software. Descriptive analysis was used to characterize the sample, and tests such as Student's t-test and Chi-square were applied to compare variables between the groups, establishing a statistical significance level of p<0.05 and calculating 95% confidence intervals.
Ethical considerationsTo carry out the study, informed consent was obtained from de patients in order to publish the results.
The study will only begin after obtaining written authorization from the Clinical Research Ethics Committee of our center.
This study was conducted in accordance with the Good Clinical Practice guidelines and there regulations and recommendations contained in the Declaration of Good Clinical Practice. Clinical Practices and there regulations and recommendations contained in the Declaration of Helsinki Declaration of Helsinki and which are included in the current legislation on the practice of clinical studies, as well as the Laws and Regulations in force in Europe and specifically in Spain.
The rules fort head equate protection of personal data, according to the European Directive 1995/46/EC on the protection of Personal Data. The processing, communication and transfer of personal data of all participating subjects will comply with the provisions of Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Personal Data, other applicable regulations and as established between the parties, if applicable.
Archiving of all relevant documents in relation to the study has been performed according to there requirements of the ICH-GCP, the Commission Directive 2005/28/EC of April 8, 2005, and according to the relevant national laws.
The data have been included in a data base that complies with Spanish legislation in this regard taking into account Regulation 679/2016, of April 27, General Data Protection Regulation and Organic Law 3/2018, of December 5, on the Protection of Personal Data and guarantee of digital rights. Likewise, the transmission of said data has been carried out with the appropriate security measures in compliance with said regulation. During documentation and analysis, patient shave been only identified by their individual patient code, while all the names of the subjects were kept secret by the investigator. For this reason, the confidentiality of personal data is guaranteed in this study, which is carried out with anonymized data.
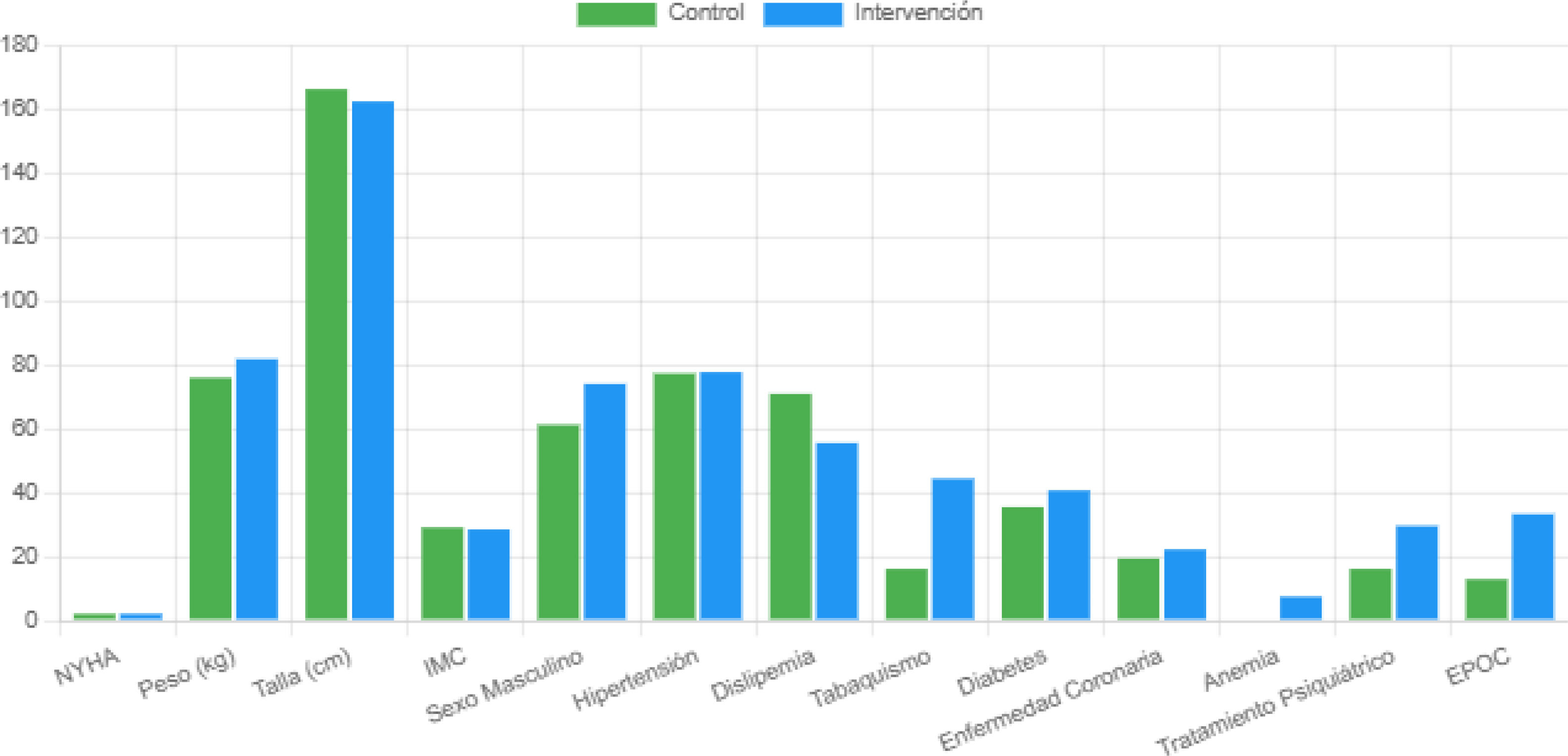
ResultsA total of 58 patients were included in the final study, after excluding 10 patients who did not complete the process. Of these 58 patients, 27 were assigned to the Intervention group and 31 to the Control group. The baseline characteristics of the patients, including demographic and clinical variables, are shown in Table 1 and Fig. 1. No statistically significant differences were found between the groups in most variables, except for the NYHA functional classification values and body weight. Patients in the Intervention group had higher NYHA scores (p=0.013) and higher body weight (p=0.054) compared to the Control group.
Baseline characteristics of the patients.
| Variable | Control (n=31) | Intervention (n=27) | Value |
|---|---|---|---|
| New York Heart Association functional classification (NYHA) | 2 (1–2) | 2 (2–3) | 0.013 |
| Weight (kg) | 76.05±10.28 | 81.91±15.37 | 0.054 |
| Size (cm) | 166.5±9.56 | 162.65±33.34 | 0.188 |
| Body mass index (BMI) | 29.1±6.12 | 28.48±5.37 | 0.055 |
| Male sex, n (%) | 19 (61.3%) | 20 (74.1%) | 0.512 |
| Hypertension, n (%) | 24 (77.4%) | 21 (77.8%) | 0.648 |
| Dyslipidemia, n (%) | 22 (71.0%) | 15 (55.6%) | 0.118 |
| Smoking, n (%) | 5 (16.1%) | 12 (44.4%) | 0.082 |
| Diabetes, n (%) | 11 (35.5%) | 11 (40.7%) | 0.837 |
| Coronary heart disease, n (%) | 6 (19.4%) | 6 (22.2%) | 0.893 |
| Anemia, n (%) | 0 (0%) | 2 (7.4%) | 0.229 |
| Psychiatric treatment, n (%) | 5 (16.1%) | 8 (29.6%) | 0.277 |
| EPOC, n (%) | 4 (12.9%) | 9 (33.3%) | 0.086 |
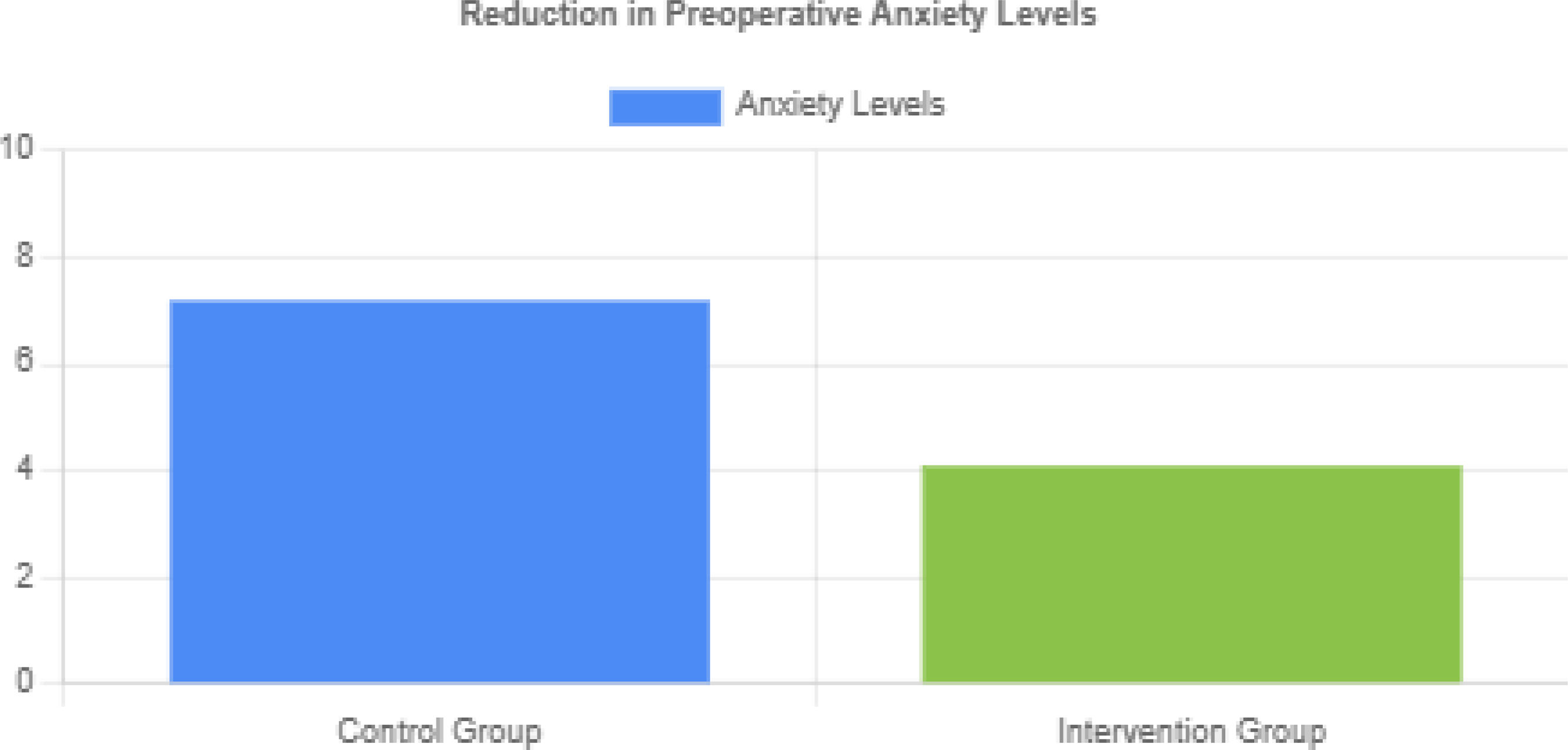
Fig. 2 shows the reduction in preoperative anxiety levels in the intervention group compared to the control group.
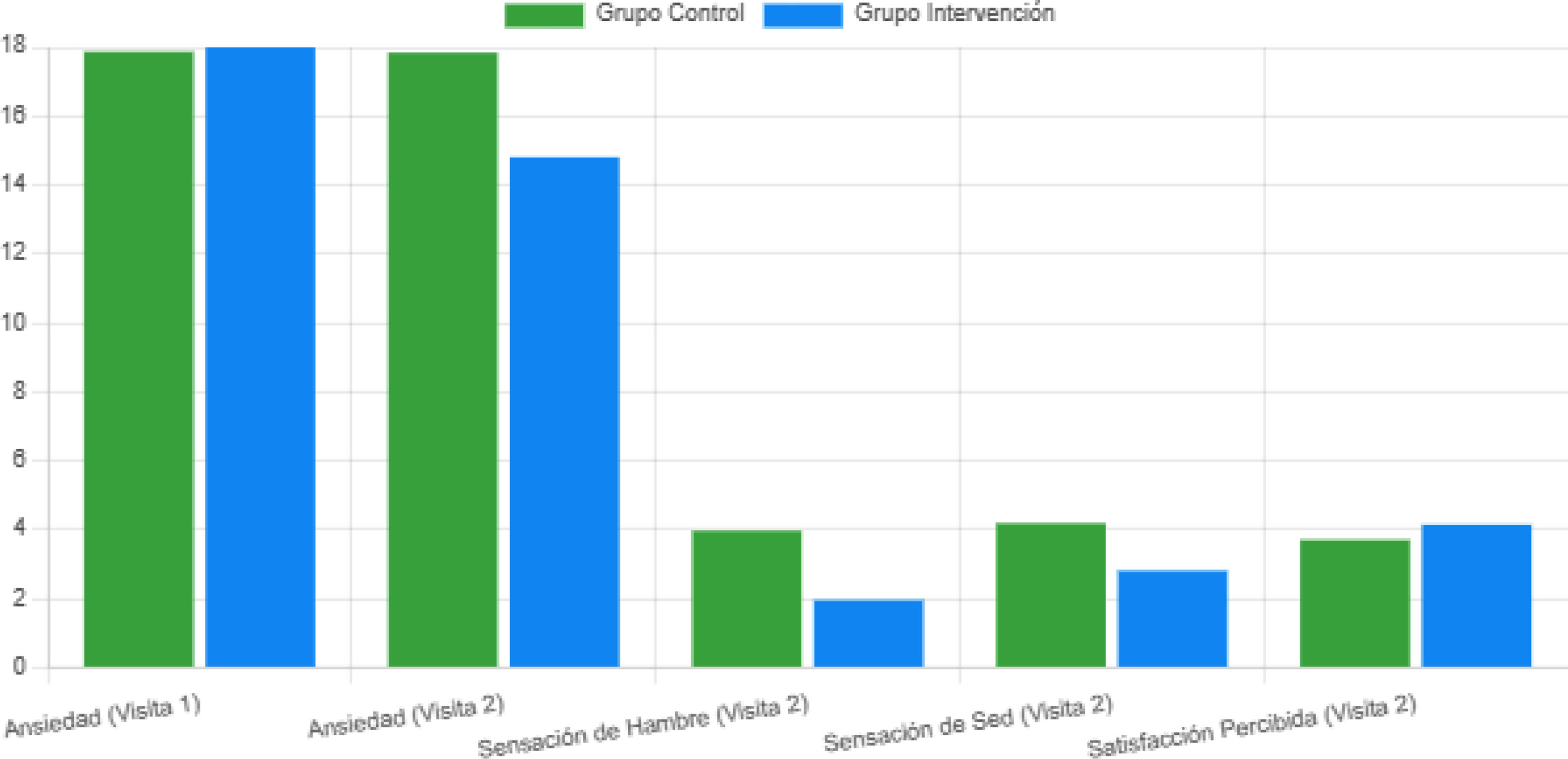
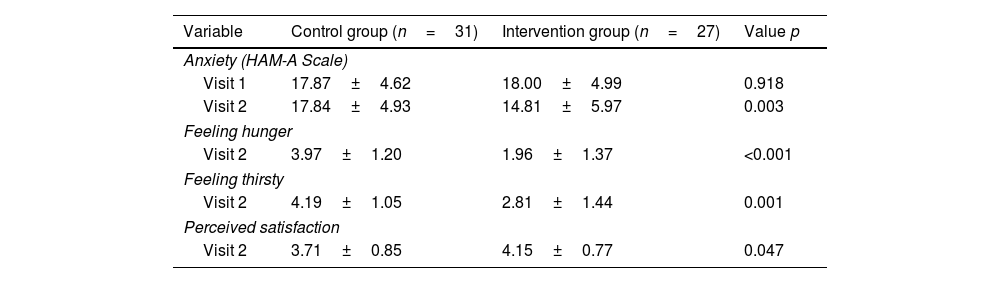
Patients in the Intervention group showed a significant reduction in preoperative anxiety levels between Visit 1 and Visit 2, according to the Hamilton Anxiety Scale (p=0.003). In addition, they presented a significant decrease in the sensation of hunger and thirst in Visit 2 compared to the Control group (p<0.001 and p=0.001, respectively). On the other hand, patients in the Intervention group reported greater perceived satisfaction during Visit 2 compared to the Control group (p=0.047).
The results of the clinical and psychological parameters evaluated throughout the study are shown in detail in Table 2 and Fig. 3. Regarding the psychological findings, patients in the Intervention group who received carbohydrate supplementation showed a significant reduction in preoperative anxiety levels between Visit 1 (preoperative) and Visit 2 (day of surgery), according to the scores obtained on the Hamilton Anxiety Scale (p=0.003).10
Evolution of anxiety, hunger, thirst and perceived satisfaction parameters in patients undergoing cardiac surgery, with and without carbohydrate supplementation.
| Variable | Control group (n=31) | Intervention group (n=27) | Value p |
|---|---|---|---|
| Anxiety (HAM-A Scale) | |||
| Visit 1 | 17.87±4.62 | 18.00±4.99 | 0.918 |
| Visit 2 | 17.84±4.93 | 14.81±5.97 | 0.003 |
| Feeling hunger | |||
| Visit 2 | 3.97±1.20 | 1.96±1.37 | <0.001 |
| Feeling thirsty | |||
| Visit 2 | 4.19±1.05 | 2.81±1.44 | 0.001 |
| Perceived satisfaction | |||
| Visit 2 | 3.71±0.85 | 4.15±0.77 | 0.047 |
This beneficial effect on preoperative anxiety is a relevant finding, given that anxiety is a common experience in patients undergoing cardiac surgery and can negatively impact their recovery.11
Additionally, the Intervention group presented a significant decrease in the subjective sensation of hunger and thirst during Visit 2, compared to the Control group that followed the traditional protocol of prolonged fasting (p<0.001 and p=0.001, respectively). These discomfort symptoms related to prolonged fasting can generate greater stress and discomfort in patients in the preoperative stage, so their mitigation through carbohydrate supplementation is a clinically relevant finding.9
Furthermore, patients in the Intervention group also reported greater perceived satisfaction during Visit 2 compared to the Control group (p=0.047). This greater patient satisfaction with their preoperative experience is an important indicator of the acceptability and clinical relevance of the carbohydrate supplementation strategy.12
The results observed in relation to the clinical and psychological parameters evaluated throughout the study demonstrate that carbohydrate supplementation had a positive impact on the preoperative experience of patients undergoing cardiac surgery. Specifically, this strategy was able to significantly reduce preoperative anxiety levels, decrease the sensation of hunger and thirst, and improve the perceived satisfaction of patients compared to the group that followed the traditional protocol of prolonged fasting.13
These findings are particularly relevant, as anxiety, discomfort, and patient dissatisfaction in the preoperative period can be associated with poorer clinical outcomes and a more prolonged recovery.14 Therefore, the incorporation of carbohydrate supplementation into the Enhanced Recovery After Cardiac Surgery (ERAS) protocols could represent an effective strategy to optimize the patient's experience and, ultimately, improve surgical outcomes.
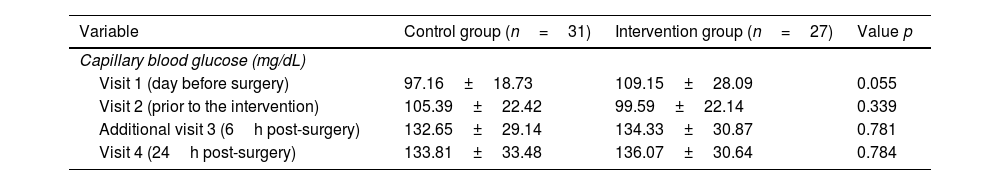
Regarding capillary glucose values, no statistically significant differences were observed between the groups at any of the evaluation time points, as shown in Table 3. Capillary blood glucose measurements were performed at four key time points: Visit 1 (the day before surgery), Visit 2 (the day of surgery, before the surgical intervention), an additional Visit 3 (6h postoperatively) to detect possible variations related to the carbohydrate load administered preoperatively, which could induce hyperglycemia during the first hours after the intervention, and Visit 4 (24h postoperatively).
Capillary blood glucose values in patients in the control group and the intervention group at the different visits.
| Variable | Control group (n=31) | Intervention group (n=27) | Value p |
|---|---|---|---|
| Capillary blood glucose (mg/dL) | |||
| Visit 1 (day before surgery) | 97.16±18.73 | 109.15±28.09 | 0.055 |
| Visit 2 (prior to the intervention) | 105.39±22.42 | 99.59±22.14 | 0.339 |
| Additional visit 3 (6h post-surgery) | 132.65±29.14 | 134.33±30.87 | 0.781 |
| Visit 4 (24h post-surgery) | 133.81±33.48 | 136.07±30.64 | 0.784 |
This analysis allows for a more precise assessment of the potential immediate metabolic effects of preoperative nutritional intervention and its relationship to postoperative glycemic fluctuations. Furthermore, since variations in postoperative blood glucose levels could be associated with the need for insulin administration, an analysis of insulin use to correct elevated glucose levels in both groups was included. However, no patients in either group were observed to require significant doses of insulin to control their glycemia. Importantly, although blood glucose measurements were presented in isolation, evaluation of administered insulin doses did not reveal significant differences between groups in the need for pharmacological interventions. This additional analysis reinforces the lack of differences between groups in postoperative glucose control. This result suggests that carbohydrate supplementation did not generate relevant metabolic alterations in the patients in the Intervention group.15
Postoperative complications and mortality were carefully assessed in both groups during the 24-h postoperative follow-up period. During follow-up, one case of acute postoperative confusion was observed in the intervention group, which was adequately treated and did not present any further complications. In the control group, one case of death due to perioperative myocardial infarction was reported, an adverse event that occurred outside the scope of the nutritional intervention protocol. However, both cases were isolated, and no statistically significant differences were found between the intervention and control groups in terms of the incidence of serious complications or mortality (p>0.05).
It is important to note that, given the quasi-experimental design and limited sample size (58 patients), the lack of statistical power may have influenced the inability to detect significant differences in these aspects. Despite the presence of some adverse events, the results suggest that carbohydrate supplementation was no associated with an increased risk of serious postoperative complications or mortality, highlighting the safety of this intervention in the context of the ERAS protocol for cardiac surgery.
Collectively, these findings strongly support the incorporation of carbohydrate supplementation as an integral part of the enhanced recovery protocols in cardiac surgery.16 This strategy has been shown to be effective in optimizing the patient's preoperative experience, significantly reducing anxiety, discomfort, and improving perceived satisfaction, without compromising safety or clinical outcomes. These positive results suggest that the implementation of this nutritional intervention in the ERAS programs for cardiac surgery could have a favorable impact on the quality of care and patient well-being.10
Discussion of resultsThe findings of this quasi-experimental, prospective, and randomized study demonstrate that carbohydrate supplementation in the preoperative period of patients undergoing scheduled cardiac surgery generates significant psychological and metabolic benefits, compared to the traditional protocol of prolonged fasting.
A key aspect evidenced by the results is the significant reduction in preoperative anxiety levels in the intervention group that received carbohydrate supplementation. Anxiety is a common experience in patients undergoing surgical procedures, especially in the field of cardiac surgery, and can have a considerable negative impact on recovery and clinical outcomes.3 Therefore, this finding is of great clinical relevance, as it suggests that the incorporation of carbohydrate supplementation into the enhanced recovery protocols before cardiac surgery (ERAS) could represent an effective strategy to mitigate preoperative anxiety levels and, ultimately, optimize the patient's experience.
The reduction in preoperative anxiety observed in the intervention group is complemented by other psychological benefits demonstrated in the study, such as the significant decrease in the sensation of hunger and thirst experienced by these patients. Prolonged fasting, a traditional practice in the perioperative period, is often associated with discomfort, inconvenience, and stress for patients.7 In this sense, carbohydrate supplementation proved to be an effective strategy to mitigate these symptoms, which also contributes to improving the preoperative experience and well-being of the patient.
Additionally, patients in the group receiving carbohydrate supplementation reported greater perceived satisfaction compared to the control group.17 This finding is of great relevance, as patient satisfaction is a key indicator of the quality of care and the acceptability of the implemented interventions.5 The improvement in perceived satisfaction suggests that the carbohydrate supplementation strategy is well-received by patients and contributes to optimizing their preoperative experience.11
It is important to note that the psychological benefits observed in the intervention group were not achieved at the expense of a deterioration in metabolic parameters. The results showed that carbohydrate supplementation did not generate significant alterations in capillary glucose levels at any of the evaluated time points, compared to the control group.9 In fact, none of the patients in either group required significant doses of insulin for glucose control in the immediate postoperative period. This finding is important because it confirms that the implementation of this proposed nutritional strategy did not compromise the patients’ metabolic stability, even in a clinical context as demanding as cardiac surgery, which is a fundamental aspect to ensure the safety and feasibility of its incorporation into clinical practice.12
The findings of this study are aligned with the scientific evidence supporting the benefits of enhanced recovery after surgery (ERAS) programs in the field of cardiac surgery.6 Several studies have shown that the implementation of ERAS strategies, which include nutritional interventions such as carbohydrate supplementation, is associated with better clinical outcomes, such as a reduction in hospital stay, postoperative complications, and healthcare costs.2
From a physiological perspective, carbohydrate supplementation in the preoperative period has been shown to be effective in mitigating the catabolic response to surgical stress, preserving muscle mass, and improving insulin sensitivity.13 These favorable metabolic effects could indirectly contribute to faster recovery and better clinical prognosis of patients undergoing cardiac surgery.14
Furthermore, the recommendations of the American Society of Anesthesiologists (ASA) on preoperative fasting support the strategy of carbohydrate supplementation, suggesting that patients can consume clear liquids up to 2h before surgery, as long as there are no conditions that may affect gastric emptying.15 This contextual evidence further strengthens the justification for the implementation of carbohydrate supplementation in cardiac surgery protocols.
On the other hand, it is important to consider some limitations of this study. First, the relatively small sample size (n=58) may limit the generalizability of the results. However, the quasi-experimental, prospective, and randomized design of the study, as well as the rigorous control of variables and the application of appropriate statistical tests, contribute to the internal validity of the findings. Additionally, the fact that the results align with the previous scientific evidence in the field of ERAS surgery supports the robustness and clinical relevance of the conclusions.
Another potential limitation is the absence of long-term measurements, as the study focused on the preoperative period and the first 24h after surgery. It would be valuable to evaluate whether the benefits observed in the patient's preoperative experience translate into faster postoperative recovery and better medium and long-term clinical outcomes. Future research could address this question, by expanding the patient follow-up and evaluating variables such as length of hospital stay, postoperative complications, and quality of life.
Furthermore, while no significant differences in postoperative complications were observed between the groups, the study did not have sufficient statistical power to clearly detect these differences. It would be recommended to conduct studies with larger samples that allow for a more robust evaluation of the impact of carbohydrate supplementation on postoperative clinical outcomes.
Despite these limitations, the findings of this study provide solid evidence on the benefits of carbohydrate supplementation in the preoperative period of patients undergoing cardiac surgery. The positive effects observed in the reduction of anxiety, the decrease in the sensation of hunger and thirst, and the improvement in the perceived satisfaction of patients, without compromising metabolic control, strongly support the incorporation of this nutritional strategy into the enhanced recovery protocols before cardiac surgery (ERAS).
The implementation of this type of nutritional interventions in ERAS programs could have relevant clinical implications. By improving the patient's preoperative experience and mitigating surgical stress, carbohydrate supplementation can contribute to faster recovery, lower incidence of complications, and ultimately, better quality of life and long-term outcomes for patients undergoing cardiac surgery.18
From a broader perspective, these findings support the importance of adopting a comprehensive and multidisciplinary approach in the care of the cardiac surgery patient, where nutritional and psychological interventions play a fundamental role in optimizing the safety, well-being, and prognosis of patients.1
In conclusion, the results of this study demonstrate that carbohydrate supplementation in the preoperative period of patients undergoing scheduled cardiac surgery generates significant psychological benefits, by reducing preoperative anxiety, decreasing the sensation of hunger and thirst, and improving the perceived satisfaction of patients, without compromising metabolic control. These findings strongly support the incorporation of this nutritional strategy into the enhanced recovery protocols before cardiac surgery (ERAS), with the potential to optimize the patient's experience and outcomes.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
FundingHCUVA Pharmacy Service.
Conflict of interestNo.