Several factors have caused the operating room to no longer be the ideal place for early surgical training, forcing the search for more effective options for simulation-based surgical learning. The objective of our study was to design and build a home-made proposal for a vascular anastomosis simulator for surgical training.
MethodsDescriptive, preliminary, observational, analytical, and prospective study. The study was divided into two phases, the simulator construction with low-cost common materials (9.75$), and its operative evaluation with the Objective Structured Assessment of Technical Skills (OSATS-Modified). The study subject was a cardiothoracic surgery junior resident (postgraduate year two, PGY-2) who used the simulator and was evaluated through recorded sessions in 2 consecutive 3-month periods (first period, FP vs. second period, SP) by a senior surgeon. The acquisition of operative skills in the creation of end-to-side (E-T-S), side-to-side (S-T-S), end-to-end (E-T-E) vascular anastomoses were evaluated.
ResultsThere were 273 sessions with a total of 4904min of simulation training between the three anastomosis modalities. A significant improvement was identified in the final OSATS-Modified scores (FP vs. SP) in the use of the Castroviejo needle holder, needle angles, and needle transfer in the E-T-S anastomosis (p<.05); graft orientation, appropriate spacing, use of Castroviejo needle holder, and the needle angles in the S-T-S (p<.05), and in the use of the Castroviejo needle holder, and needle transfer in the E-T-E (p<.05). Significant improvement was reported in E-T-S anastomosis time and S-T-S (p<.05).
ConclusionsOur home-made portable prototype has proven to be very efficient in improving operational skills on a smaller scale; however, our findings need to be extrapolated to a larger population of surgical residents. Current evidence suggests that skills acquired through simulation-based training are transferred and positively impact the surgical environment.
Diversos factores han provocado que el quirófano deje de ser el lugar idóneo para la formación quirúrgica temprana, obligando a la búsqueda de más opciones efectivas para el aprendizaje quirúrgico basado en simulación. El objetivo de nuestro estudio fue diseñar y construir una propuesta casera de un simulador de anastomosis vascular que permita el entrenamiento quirúrgico.
MétodosEstudio descriptivo, preliminar, observacional, analítico y prospectivo. Se dividió en 2 fases: la construcción del simulador con materiales comunes de bajo costo (9,75$) y su evaluación operativa con la Evaluación Objetiva Estructurada de Habilidades Técnicas (EOEHT-Modificada. El sujeto de estudio fue un residente junior de Cirugía Cardiotorácica (posgrado año dos, PA-2), quien utilizó el simulador y fue evaluado a través de sesiones grabadas en 2 períodos consecutivos de 3 meses (primer período, PP vs. segundo período, SP) por un cirujano sénior. Se evaluó la adquisición de habilidades operativas en la creación de anastomosis vasculares término-lateral (TL), látero-lateral (L-L) y término-terminal (T-T).
ResultadosFueron 273 sesiones con un total de 4.904min de entrenamiento de simulación entre las 3 modalidades de anastomosis. Se identificó una mejora significativa en las puntuaciones finales modificadas por EOEHT (PP vs. SP) en el uso del portaagujas de Castroviejo, los ángulos de la aguja y la transferencia de la aguja en la anastomosis T-L (p<0,05); la orientación del injerto, el espaciamiento adecuado, el uso del portaagujas de Castroviejo y los ángulos de la aguja en la L-L (p<0,05), y en el uso del portaagujas de Castroviejo y la transferencia de la aguja en la T-T (p<0,05). Se reporta una mejora significativa en el tiempo de anastomosis T-L y L-L (p<0,05).
ConclusionesNuestro prototipo portátil hecho en casa ha demostrado ser muy eficiente para mejorar las habilidades operativas a menor escala; sin embargo, nuestros hallazgos deben extrapolarse a una población mayor de residentes quirúrgicos. La evidencia actual demuestra que las habilidades adquiridas a través del entrenamiento basado en simulación se transfieren y tienen un impacto positivo en el entorno quirúrgico.
The surgical training of Cardiothoracic Surgery residents is basically based on three pillars of learning, the theoretical component, the strengthening of operative skills, and the practical component.1 These learning milestones have endured for many years; however, recently the latter have undergone a series of changes in response to problems associated with patient safety, financial pressures, ethical and medico-legal conflicts, work hours, COVID-19 pandemic and among others, causing that the operating room is no longer the ideal place for early surgical training of Cardiothoracic Surgery residents.2–6 This has forced surgical mentors to search for more effective options and methods for teaching, and acquiring operative skills based on surgical simulation.
The objective of this brief study was to design and build a home-made proposal for a low-cost, and portable vascular anastomosis simulator, which allows the operative training of Cardiothoracic Surgery residents from the comfort of their home and under the supervision of a tutor surgical.
MethodsDesign and sample sizeA preliminary, descriptive, observational, analytical, and prospective study was carried out. The study was divided into two phases, the first was related to the construction of the vascular anastomosis simulator and the second to the evaluation of training and acquisition of surgical skills with its use. The study subject was a junior resident of Cardiothoracic Surgery (Postgraduate Year two, PGY-2) belonging to the Thoracic and Cardiovascular Surgery program granted by the Universidad Nacional Mayor de San Marcos at the Edgardo Rebagliati Martins National Hospital (Total PGY-5). This hospital institution belongs to the Social Health Insurance, and is located in Lima, capital of Peru; the number of patients currently affiliated with this hospital is close to 10% of the national population (approximately 2,013,452 inhabitants).7 After the construction of the simulator, the acquisition of operational skills in the study subject was evaluated periodically and continuously (Interday) during its use for a period of six months (June–November 2020). All training sessions were recorded by a video camera, timed, and evaluated in a second moment by a surgical mentor (Senior Surgeon). The sessions consisted of the creation of End-to-Side (E-T-S), Side-to-Side (S-T-S), and End-to-End (E-T-E) vascular anastomoses, and finally, sessions that were not properly documented and evaluated during training were totally excluded from the study.
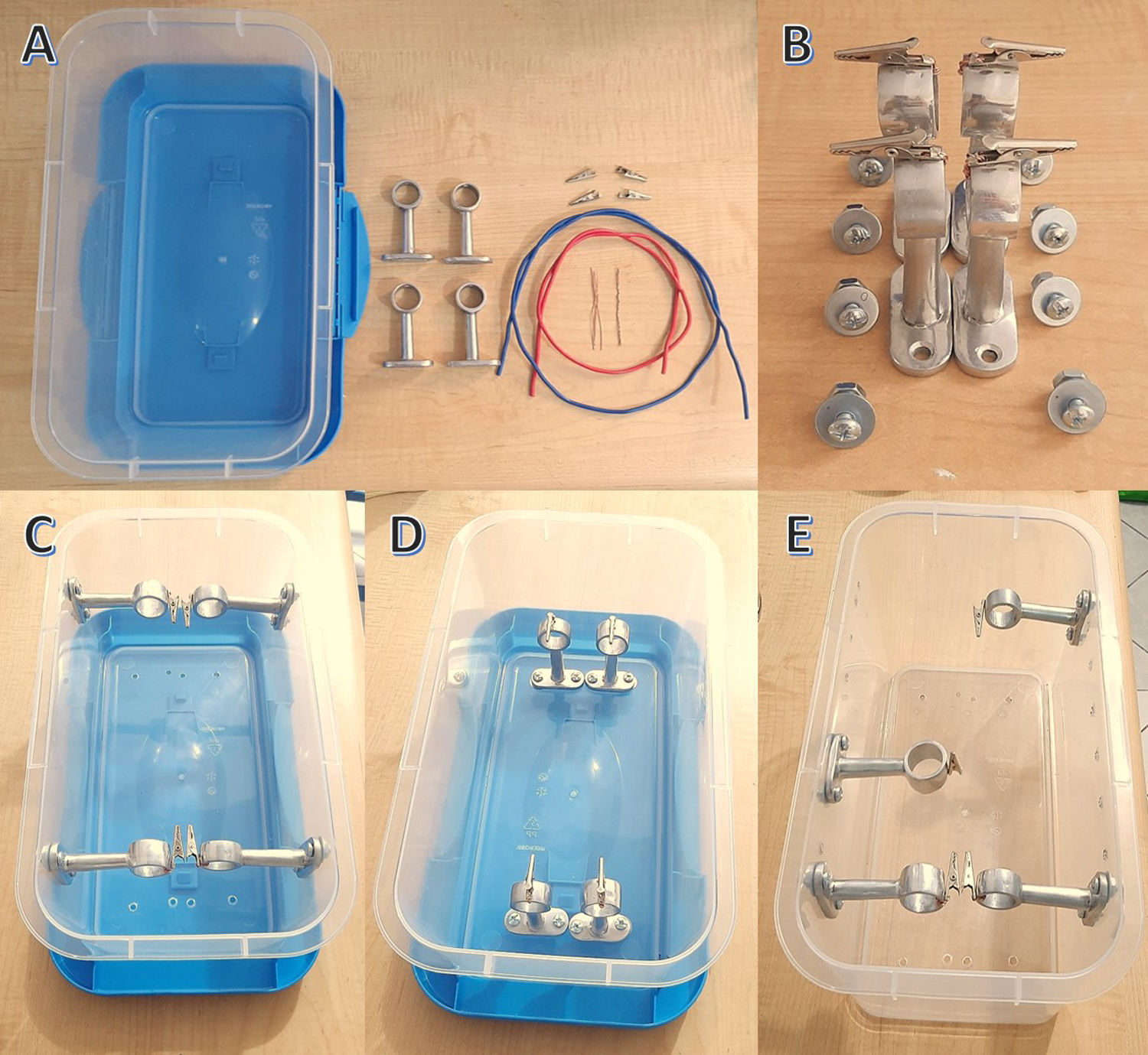
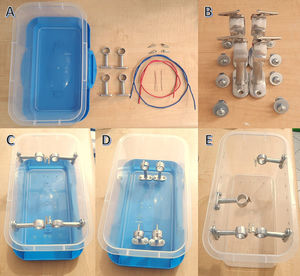
Design, construction, and use of the vascular anastomosis simulatorThe main principles that governed the construction of the vascular anastomosis simulator were portability, ease of use, and high reproducibility. The materials used were inexpensive and easy to acquire, which included 01 plastic container with a lid (30×15×10cm; 2.5$), 04 small crocodile-type hooks (2$), galvanized fine wire (20cm, 0.25$), 04 chrome brackets for installation of curtains (3$), 08 anchor bolts with nut (5mm, 2$) and tools such as pliers and screwdriver (Fig. 1). With the materials described, the 04 small crocodile-type hooks were joined with each of the 04 upper segments of the chrome-plated supports with the fine galvanized wire. Subsequently, these 04 fitted parts were coupled with the anchor bolts with nut according to the arrangement and the type of anastomosis to be performed; that is, placed in parallel in S-T-S anastomoses or perpendicular in E-T-E, and E-T-S (Fig. 1).
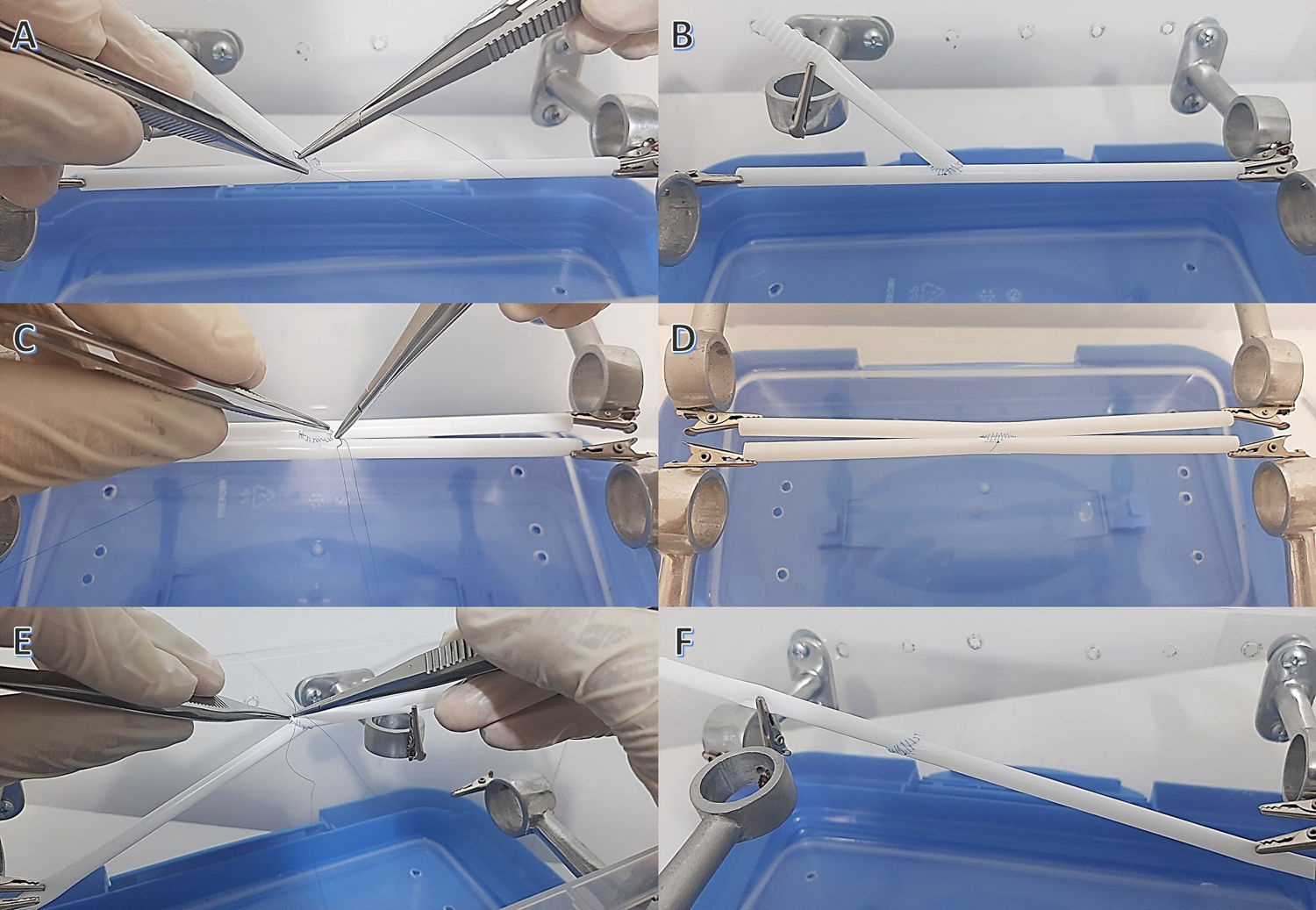
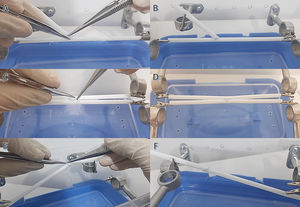
To use the vascular anastomosis simulator, materials were required that mimic the arrangement and size of vascular grafts, such as thin plastic tubes 15cm long and 2–3mm in lumen (for example, straws); and also, vascular surgical instruments (Castroviejo, vascular dissection forceps, scissors, and scalpel) and 6 and 7–0 polypropylene sutures. The thin plastic tubes were arranged in a parallel way and held by the 04 small crocodile-type hooks for the S-T-S anastomosis and perpendicularly for the E-T-E, and E-T-S anastomoses. To perform the E-T-S anastomosis, it was required to place a thin tube between 2 small hooks and the next tube held in its proximal segment by a hook and with its distal end oriented perpendicular to the first tube. To perform the E-T-E anastomosis, it was necessary to place a thin tube held by a hook in its proximal portion and oriented towards another tube with the same arrangement, in such a way that there is a close distance for performing the anastomosis (Fig. 2).
Data collection and study variablesThe primary source of information derived directly from the observation of the recorded sessions and data collection related to the subject's training during the period established by the study. The information collected was selected and arranged chronologically according to its development; finally, in a second instance, the data was collected with double-typing mechanisms and review through a checklist.
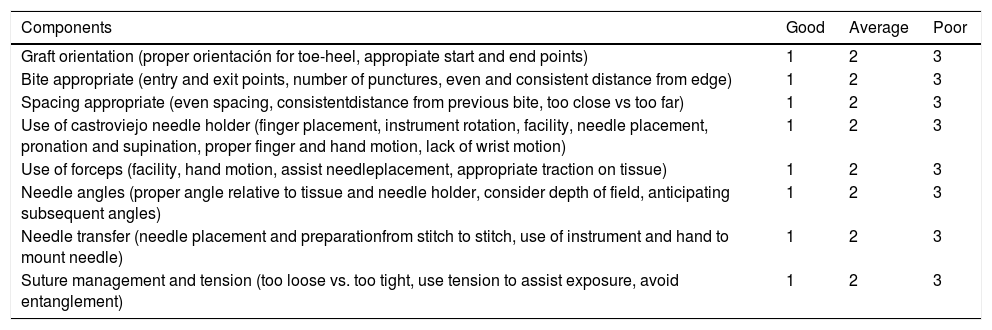
The variables evaluated during the training were taken according to the Objective Structured Assessment of Technical Skills (OSATS-Modified), this score was proposed by the University of Toronto in 1990 to evaluate the acquisition of operative skills during the surgical simulation.3 Components of this rating score included graft orientation, bites, spacing, use of needle holder, use of forceps, needle angles, needle transfer, suture management, and tension, and were individually scored 1 (Good), 2 (Average), or 3 (Poor) as observed by the surgical tutor (Table 1). Likewise, the other variable evaluated was the time of the creation of the vascular anastomosis, whose value was considered in minutes (Chronometry). The scores of all the previously described variables were grouped into three groups according to the type of vascular anastomosis performed: E-T-S, E-T-E, and S-T-S; and they were evaluated in two time periods: First Period (FP): June–July–August, and Second Period (SP): September–October–November.
Components of performance rating scores (OSATS).
| Components | Good | Average | Poor |
|---|---|---|---|
| Graft orientation (proper orientación for toe-heel, appropiate start and end points) | 1 | 2 | 3 |
| Bite appropriate (entry and exit points, number of punctures, even and consistent distance from edge) | 1 | 2 | 3 |
| Spacing appropriate (even spacing, consistentdistance from previous bite, too close vs too far) | 1 | 2 | 3 |
| Use of castroviejo needle holder (finger placement, instrument rotation, facility, needle placement, pronation and supination, proper finger and hand motion, lack of wrist motion) | 1 | 2 | 3 |
| Use of forceps (facility, hand motion, assist needleplacement, appropriate traction on tissue) | 1 | 2 | 3 |
| Needle angles (proper angle relative to tissue and needle holder, consider depth of field, anticipating subsequent angles) | 1 | 2 | 3 |
| Needle transfer (needle placement and preparationfrom stitch to stitch, use of instrument and hand to mount needle) | 1 | 2 | 3 |
| Suture management and tension (too loose vs. too tight, use tension to assist exposure, avoid entanglement) | 1 | 2 | 3 |
Good: able to accomplish goal without hesitation, showing excellent progress and flow; Average: able to accomplish goal with hesitation, discontinuous progress and flow; Poor: able to partially accomplish goal with hesitation. Adapted from Objective Structured Assessment of Technical Skill (OSATS).3
Continuous data were expressed as mean±Standard Deviation (SD) as appropriate. The data were analyzed with paired t-tests to compare the scores obtained during the FP versus SP in the three types of anastomosis. It was not necessary to assess inter-rater reliability at the time of scoring the anastomosis sessions, as he was only one rater. The differences were considered significant with a value of p<0.05. In all cases, the data analysis was performed using the statistical program STATA MP v16 for the Windows 10 version.
Ethical aspectsThe evaluation and ethical feasibility of this work were in charge of the Postgraduate Area of the National University of San Marcos and the Edgardo Rebagliati Martins National Hospital (RCEI-7), Lima, Peru; who reviewed and approved the protocol of this study. The confidentiality of the information and the principles of bioethics outlined in the Declaration of Helsinki were respected.
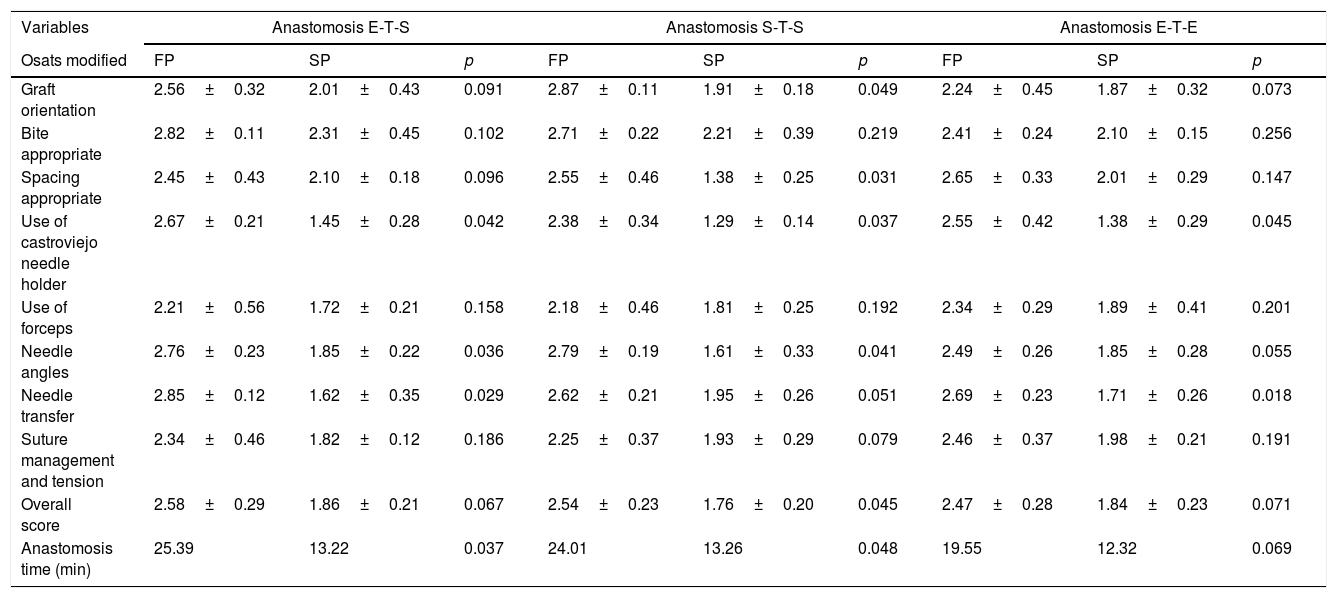
ResultsTechnical skills assessmentDuring the period proposed by the study, 91 surgical training sessions were carried out for each of the E-T-S, S-T-S, and E-T-E anastomosis types, adding a total of 273 sessions performed by our study subject. An improvement was obtained in the scores in the SP of all the items evaluated; However, for the E-T-S anastomosis, a significant reduction in the score was identified of Use of Castroviejo needle holder (2.67±0.21 vs. 1.45±0.28; p=0.042), Needle angles (2.76±0.23 vs. 1.85±0.22; p=0.036) and the Needle transfer (2.85±0.12 vs. 1.62±0.35; p=0.042). In the S-T-S anastomosis, the statistically significant items were the Graft orientation (2.87±0.11 vs. 1.91±0.18; p=0.049), Spacing appropriate (2.55±0.46 vs. 1.38±0.25; p=0.031), Use of Castroviejo needle holder (2.38±0.34 vs. 1.29±0.14; p=0.037), and the Needle angles (2.79±0.19 vs. 1.61±0.33; p=0.041); Likewise, an improvement in the general score in relation to the others was evidenced in this type of anastomosis (Overall score; 2.54±0.23 vs. 1.76±0.20; p=0.045). Finally, in the E-T-E anastomosis, only two items showed significant results, and they were the Use of Castroviejo needle holder (2.55±0.42 vs. 1.38±0.29; p=0.045) and the Needle transfer (2.69±0.23 vs. 1.71±0.26; p=0.018). It should be noted that there were items that did not show statistically significant variation between the three types of anastomosis, and they were the Bite appropriate (p=0.102 vs. 0.219 vs. 0.256), Use of forceps (p=0.158 vs. 0.192 vs. 0.201), and Suture management and tension (p=0.186 vs. 0.079 vs. 0.191) (Table 2).
Mean scores obtained according to the type of anastomosis and OSATS.
| Variables | Anastomosis E-T-S | Anastomosis S-T-S | Anastomosis E-T-E | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Osats modified | FP | SP | p | FP | SP | p | FP | SP | p |
| Graft orientation | 2.56±0.32 | 2.01±0.43 | 0.091 | 2.87±0.11 | 1.91±0.18 | 0.049 | 2.24±0.45 | 1.87±0.32 | 0.073 |
| Bite appropriate | 2.82±0.11 | 2.31±0.45 | 0.102 | 2.71±0.22 | 2.21±0.39 | 0.219 | 2.41±0.24 | 2.10±0.15 | 0.256 |
| Spacing appropriate | 2.45±0.43 | 2.10±0.18 | 0.096 | 2.55±0.46 | 1.38±0.25 | 0.031 | 2.65±0.33 | 2.01±0.29 | 0.147 |
| Use of castroviejo needle holder | 2.67±0.21 | 1.45±0.28 | 0.042 | 2.38±0.34 | 1.29±0.14 | 0.037 | 2.55±0.42 | 1.38±0.29 | 0.045 |
| Use of forceps | 2.21±0.56 | 1.72±0.21 | 0.158 | 2.18±0.46 | 1.81±0.25 | 0.192 | 2.34±0.29 | 1.89±0.41 | 0.201 |
| Needle angles | 2.76±0.23 | 1.85±0.22 | 0.036 | 2.79±0.19 | 1.61±0.33 | 0.041 | 2.49±0.26 | 1.85±0.28 | 0.055 |
| Needle transfer | 2.85±0.12 | 1.62±0.35 | 0.029 | 2.62±0.21 | 1.95±0.26 | 0.051 | 2.69±0.23 | 1.71±0.26 | 0.018 |
| Suture management and tension | 2.34±0.46 | 1.82±0.12 | 0.186 | 2.25±0.37 | 1.93±0.29 | 0.079 | 2.46±0.37 | 1.98±0.21 | 0.191 |
| Overall score | 2.58±0.29 | 1.86±0.21 | 0.067 | 2.54±0.23 | 1.76±0.20 | 0.045 | 2.47±0.28 | 1.84±0.23 | 0.071 |
| Anastomosis time (min) | 25.39 | 13.22 | 0.037 | 24.01 | 13.26 | 0.048 | 19.55 | 12.32 | 0.069 |
End-to-Side (E-T-S), Side-to-Side (S-T-S), End-to-End (E-T-E). First Period (FP), Second Period (SP).
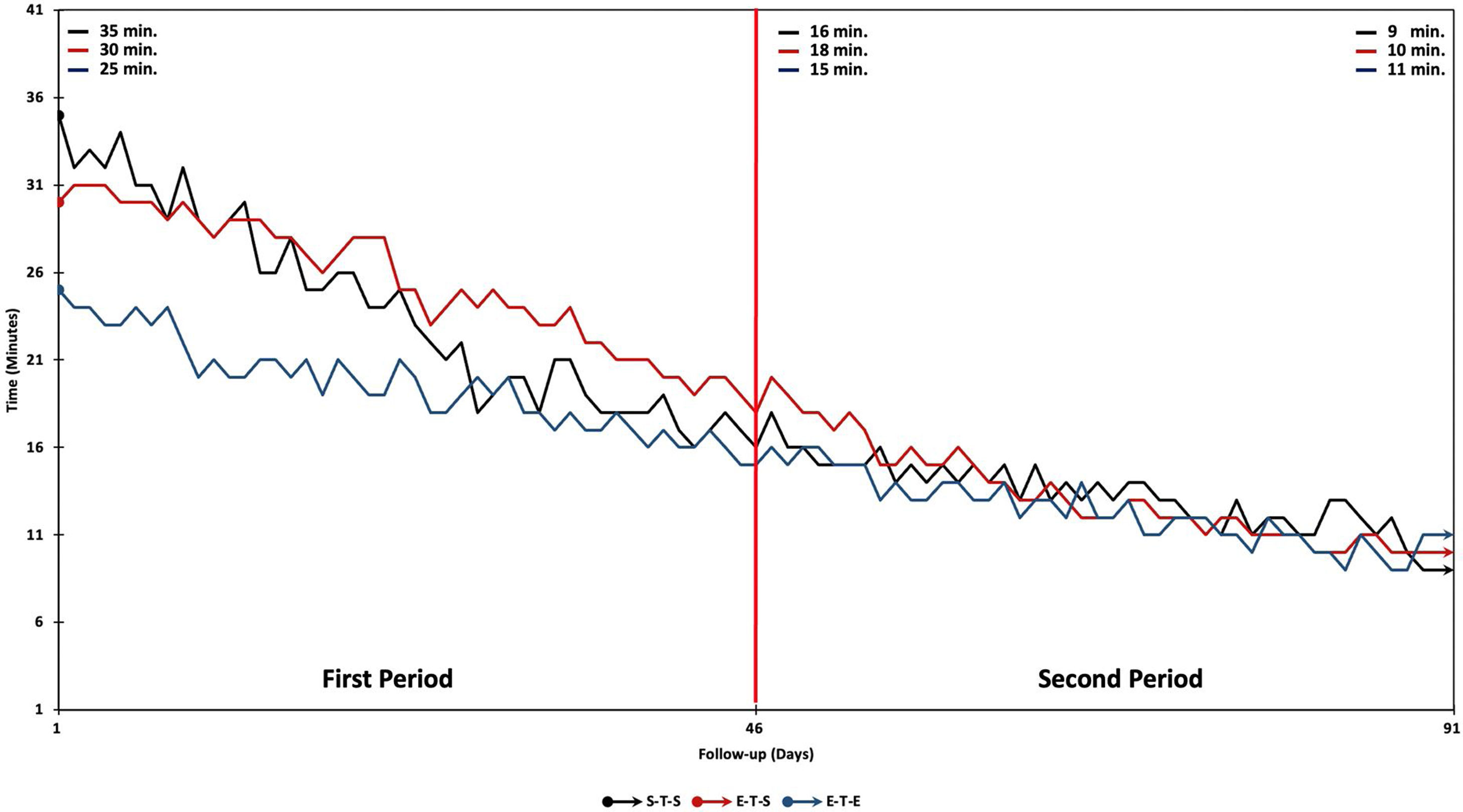
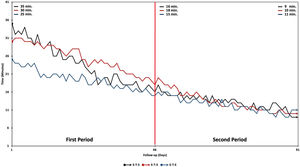
A total of 4904minutes (Min) of simulation training was performed between the three types of anastomosis for six months (E-T-S, 1762 Min; S-T-S, 1690 Min; E-T-E, 1452 Min); Likewise, an average was shown in the FP of 25.39, 24.01, 19.55 Min and in the SP of 13.22, 13.26, 12.32 Min respectively. During days 01, 46, and 91 of the training sessions, the results that ranged from 35, 30, 25min vs. 16, 18, 15min vs. 9, 10, 11min; and also, a statistically significant reduction in anastomosis time was evidenced only in the E-T-S (p=0.037) and S-T-S (p=0.048) anastomoses (Fig. 3).
DiscussionMore than a century ago, Halsted proposed a surgical graduation model to his Johns Hopkins University students, based on high-volume, constant-exposure surgical teaching. This proposal conditioned residents long hours of work in the operating room (more than 110h a week) with exposure to surgical errors on patients, the impossibility to marry and start a family and stay full time in the hospital.6 With the passing of the years and the advent of new advances in surgical knowledge, it has demanded greater professional, ethical and deontological transparency during patient care, added to the surgeon's operational expertise.8
The latter has been working from residency programs, where medical education in surgical residents, especially those in Cardiothoracic Surgery, has recently been greatly affected due to factors associated with restriction of working hours, zero tolerance for medical errors, pandemic due to COVID-19, ethical and medical-legal conflicts.1,9 Due to this, the classic strategy of teaching in the operating room under the premise of “First see, then do and finally teach“, is being displaced by the paradigm of simulation-based surgical learning. In many surgical specialty training centers around the world, simulation laboratories and operating rooms have been progressively implemented; generating a great opportunity for training and acquisition of operational skills without risk to the patient.10,11,5 In our country, few training institutions have this new operational simulation model; however, there are still notable learning gaps that have forced many surgical students and residents to design and build low-cost, portable, and fully reproducible home-made simulators.
Our work presents the proposal of a vascular anastomosis simulator, which is the first of its kind in our country, being a friendly prototype and easy to use from the comfort of home; however, it is not the first time that something similar has been designed. Fann et al. designed a coronary vascular anastomosis training station on pig hearts and a portable simulator, using the OSATS they obtained scores that ranged from 1.29±0.45 to 1.58±0.50 (Needle holder use, needle transfer and suture management and tension; p<0.001) during the 6 months of training.3 Similar findings were obtained in the S-T-S anastomosis simulation during the SP in the items Spacing appropriate (1.38±0.25, p=0.031) and Use of Castroviejo needle holder (1.29±0.14, p=0.037).
On the other hand, Price et al. described that residents who underwent training with vascular anastomosis simulators guided obtained significantly higher scores than those who received training on without mentorship simulators (OSATS; 23.7±4.7 vs 18.5±3.9, p=0.003), and also performed vascular anastomoses with faster (777″ vs 977″, p=0.04).4 These latter findings were also described by Fann et al. that showed an improvement of 15% in the construction times of the anastomosis in the simulator during the first week of use (426±115″ to 362±94″, p=0.04).2 Regarding the speed of construction of the anastomoses during the simulation, we reported a gradual improvement pattern that initially ranged with a mean of 30min, 16.3min during session 46 (P50), and finally 10min at the end of the study period. This improvement in the time-curve reflects what has been previously described in the studies and highlights the importance of continuity of training on the acquisition of operational skills based on the phenomenon of repetition.
The latter, together with the phenomenon of “Plateau” and “Ceiling”, have been infrequently described and many times underestimated during the subtotal statistical analysis of the results described in some works, because despite the evident improvement in manual skills in most of the participants after using the surgical simulators, there would be a small group of participants who would not achieve significant improvement despite their continued use. Such is the case of the findings described by Fann et al., who observed that 25% of the residents did not manage to improve significantly with the anastomosis simulators, and also in this subgroup it was identified that the majority were apprentices with a higher degree of expertise and experience on the rest of the study participants, causing surprise and attention in the authors about these phenomena of operational learning.2
The “Plateau” phenomenon is based on the resident's ability to improve in the short term; however, it is necessary to define whether the trainee has reached a plateau in his technical ability for one type of anastomosis during the simulation and whether continuous training could improve the participant's abilities and skills to the next operational level. On the other hand, the “Ceiling” phenomenon described in many anastomosis simulators is based on the fact that a training station is not capable of distinguishing the operative level between a junior or expert apprentice, causing an outstanding learning curve in the former. and the second shows a “Ceiling” effect due to the great baseline operational expertise that would not generate a greater technical curve.
Taking into consideration what has been described and about the findings of our study, we could infer that the improvement in the operative learning curve of our study subject would be strongly related to his low baseline level of surgical expertise and that, with training deliberately, he was able to obtain optimal scores on the OSATS-Modified and an improvement in the time it took to create the anastomosis. Likewise, we highlight the importance of both phenomena of operative learning (“Plateau and Ceiling”), since it would help us to identify our target population according to the type of surgical simulator, to achieve greater operative skills according to the baseline degree of experience and expertise of the trainee at the time of starting their training.
Even though in our work we are based on a small vessel vascular anastomosis simulation system, there are reports of larger caliber vessel simulators with results similar to those described. Such is the case of Sigounas et al. who developed a vascular anastomosis simulator for femoro-popliteal bypass, carotid endarterectomy and repair of abdominal aortic aneurysm; Likewise, they described statistically significant findings in OSATS scores before and after training (2.6 vs 3.1, p=0.01), highlighting the vital importance of simulation-guided surgical training.6
There is no doubt that the cognitive and operational learning of apprentices in the operating room provides limited opportunities for training, reflection and feedback on surgical skills; so much so, that simulation learning emerges as a proposal for training and necessary practice outside the operating room.12,13 Recently, surgical simulators have been grouped into organic and inorganic, the former consisting of live animal models and fresh human cadavers, is considered to some extent very high fidelity; However, this modality conditions a series of economic and merely ethical–legal details. Due to this, the use of simulators with real organs has been proposed with the help of synthetic grafts and tissues monitored in vivo, simulating an operating room.14–16 This last operational proposal has generated greater trust and adherence on the part of the participants, allowing a more realistic appearance that would help to identify technical and learning deficiencies at the time of their interaction.4 Despite all the novel advantages described, there would still be a series of drawbacks related to greater logistics for the acquisition and preparation of materials, the need for an environment that simulates a real operating room, the non-portability of the training station, and more. This has forced the search for other alternatives oriented towards simulation with inorganic materials, with the aim of acquiring operational skills in a simulator that offers safety, zero risk to the patient, low cost, and portability for continuous training outside the operating room like the one proposed in our study.
Simulation training has been widely studied and is currently governed by a series of models and theories such as that proposed by Ericsson et al., Who argue that simulation provides the opportunity for the learner to deliberately perform and practice technical skills without concern for consequences or repercussions on the patient.17 Likewise, they suggest that previous experience with the anastomosis training model may not be associated with improved technical skills if the exposure is not repetitive or periodic, a fact that would condition the need for many hours of deliberate practice to achieve high levels of operational performance. By referring to the term “deliberate practice”, it would imply focusing on a defined and repetitive activity that, together with adequate mentoring and feedback on performance, could achieve the desired degree of expertise.17,18
On the other hand, several principles associated with simulation learning have been described, such as massive learning vs. interleaved learning, the first one would be based on the evaluation of the performance of an anastomosis session without rest periods and at the end of them (Acquisition performance), observing some inconsistencies on the performance and acquisition of retention skills.19,20 While interspersed learning added to factors such as the type of vascular anastomosis (Simple vs. complex), the amount of time between practice sessions according to the complexity of the sessions (Short vs. long), and the motivation of the learner would add to the obtaining of results encouraging and satisfying at the end of each vascular training session.3,20
Nowadays, when speaking of surgical learning by operative simulation, we are not referring to utopias or futuristic visions, this educational modality is universally feasible and has gained great expectation among the training institutions of surgical residents worldwide. Such is the case, that organizations such as The American College of Surgeons (ACS), The Society of Thoracic Surgeons (STS), The Thoracic Surgery Residents Association (TSRA) and among others, have been promoting and developing a great diversity of training programs and surgical accreditation based on operative simulation aimed at surgeons and surgical residents.3,21–23
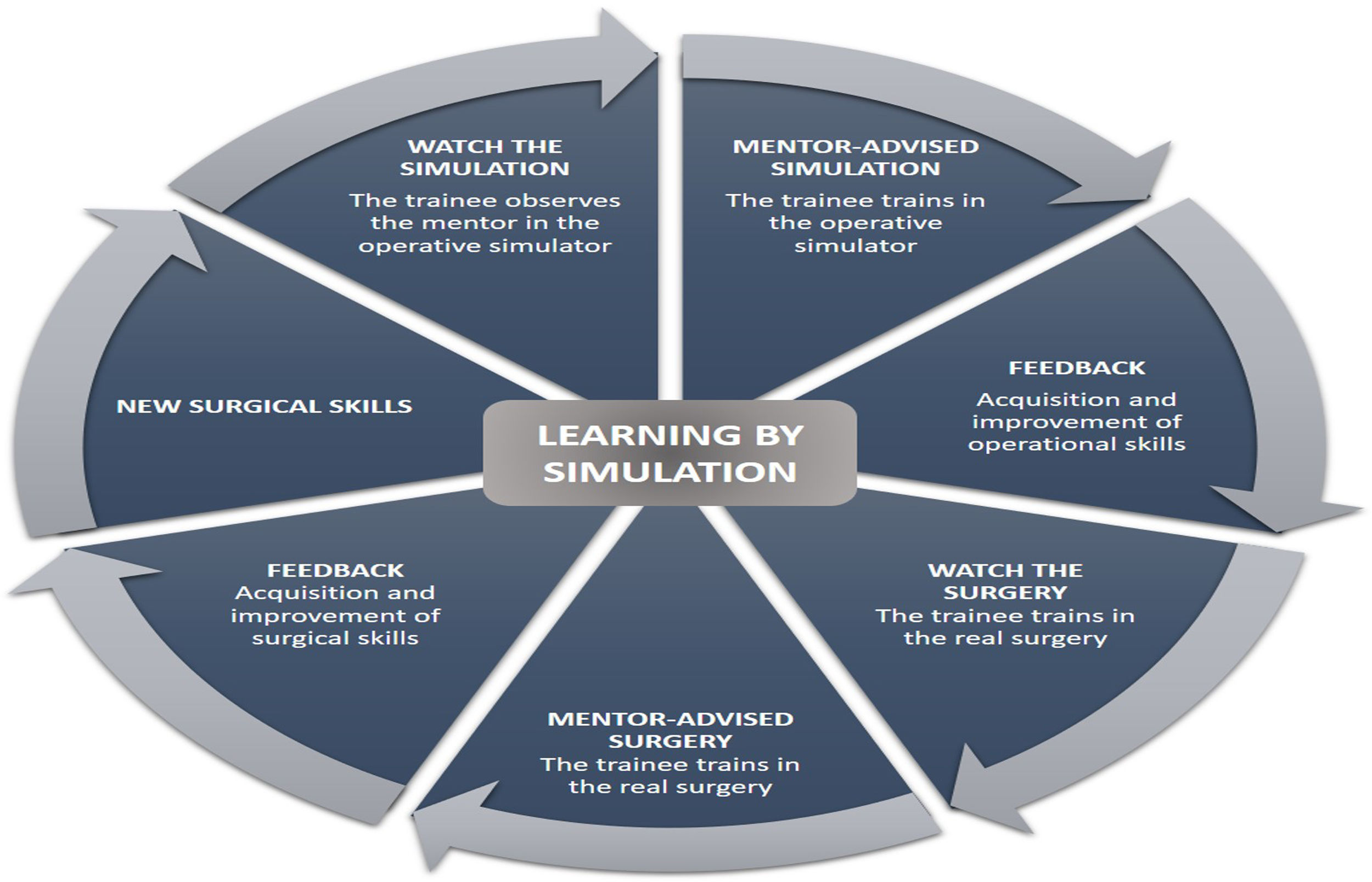
Current evidence suggests that skills acquired by simulation transfer and positively impact the surgical environment; however, we are aware that the greatest challenge for the future revolves around understanding the value of this novel learning proposal and developing an educational plan that incorporates surgical simulators as a fundamental part of surgical training (Fig. 4). Our country has recently been implementing this novel educational proposal in resident training institutions, requiring further research with various and new prototypes such as the one described in our work. Despite the preliminary and encouraging results of the simulator with our study subject, it should be extrapolated to a larger population of participants, taking into account the various conditioning factors of simulation learning during the analysis of its effectiveness in acquiring operational skills in the surgical resident.
Conflict of interestsThe author declares no conflict of interest.