Tuberculosis (TB) is a chronic granulomatous disease caused by Mycobacterium tuberculosis, with extrapulmonary manifestations occurring in approximately 1% of cases. Among these, central nervous system involvement, including intracranial tuberculomas, is rare. We present the case of a 13-year-old female from Borama, Somalia, admitted with abnormal lip movements and a complex medical history, including weight loss, recurrent urinary tract infections, and a familial predisposition to TB. Neurological examination revealed left-sided facial deviation and hyperreflexia, prompting investigations that confirmed left temporal epilepsy and a right-sided tuberculoma. Treatment with levetiracetam and anti-TB medication led to significant improvement. This case underscores the importance of considering tuberculomas in the differential diagnosis of neurological presentations, even in non-HIV patients, especially in resource-limited settings like Africa.
La tuberculosis (TB) es una enfermedad granulomatosa crónica causada por Mycobacterium tuberculosis, con manifestaciones extrapulmonares en aproximadamente el 1% de los casos. Entre éstas, la afectación del sistema nervioso central (SNC), incluidos los tuberculomas intracraneales, es poco frecuente. Presentamos el caso de una niña de 13 años de Borama, Somalia, que ingresó con movimientos labiales anormales y una historia clínica compleja, que incluía pérdida de peso, infecciones urinarias recurrentes y una predisposición familiar a la tuberculosis. La exploración neurológica reveló desviación facial izquierda e hiperreflexia, por lo que se realizaron pruebas que confirmaron epilepsia temporal izquierda y un tuberculoma derecho. El tratamiento con levetiracetam y medicación antituberculosa condujo a una mejoría significativa. Este caso subraya la importancia de considerar los tuberculomas en el diagnóstico diferencial de las presentaciones neurológicas, incluso en pacientes sin VIH, especialmente en entornos con recursos limitados como África.
Tuberculosis (TB), caused by Mycobacterium tuberculosis (MTB), is recognized as a chronic granulomatous disease primarily affecting the pulmonary system, yet its potential to manifest in various extrapulmonary sites is acknowledged.1,2 Extrapulmonary TB occurrences are relatively rare, estimated at around 1%, with central nervous system (CNS) involvement constituting approximately 15% of these cases.1,2 Within the spectrum of CNS TB manifestations, intracranial tuberculomas represent a notably uncommon subset, with their prevalence markedly lower compared to other CNS pathologies associated with TB.2 The clinical presentation of intracranial tuberculomas is frequently non-specific, posing challenges in diagnosis, and often leading to delays in appropriate management.3 Moreover, literature regarding tuberculomas is notably scarce in Eastern Africa, including Somalia, which is characterized by limited publication output. Therefore, the dissemination of this case report from Somalia serves to contribute valuable insights into an underreported aspect of TB presentation within this region.
Moreover, the significance of this case report lies in its relevance to resource-limited settings, particularly in Africa. While the prevalence of TB is higher in these regions, cases with neurological presentations, including tuberculomas, often go undiagnosed or misdiagnosed due to limited resources and expertise. By documenting this case, we aim to raise awareness among healthcare professionals working in similar environments, emphasizing the need for considering tuberculomas in the differential diagnosis of neurological manifestations, even in non-HIV patients.
Case presentationA 13-year-old female from Borama, residing in the capital city of the Awdal region, Somalia/Somaliland was admitted to Alaalleh Hospital presenting with abnormal lip movements persisting for 3 days. The patient's chief complaint included involuntary movements of the lips, she had a notable history of weight loss, recurrent urinary tract infections, and periodic febrile episodes. The sudden onset of abnormal lip movements was accompanied by tongue biting and left facial deviation, although the patient remained conscious and aware. There were no reported fever, headache, neck stiffness, or weakness in the lower limbs.
Further exploration of the patient's medical background revealed a familial predisposition to TB, with her sister previously diagnosed with TB lymphoadenitis treated with anti-TB medication earlier in the year. Additionally, her recent academic performance had declined, despite her previous reputation as an excellent student. Socially, she was a seventh-grade student, typically characterized by energetic behavior, although recent observations noted a decline in her usual vigor.
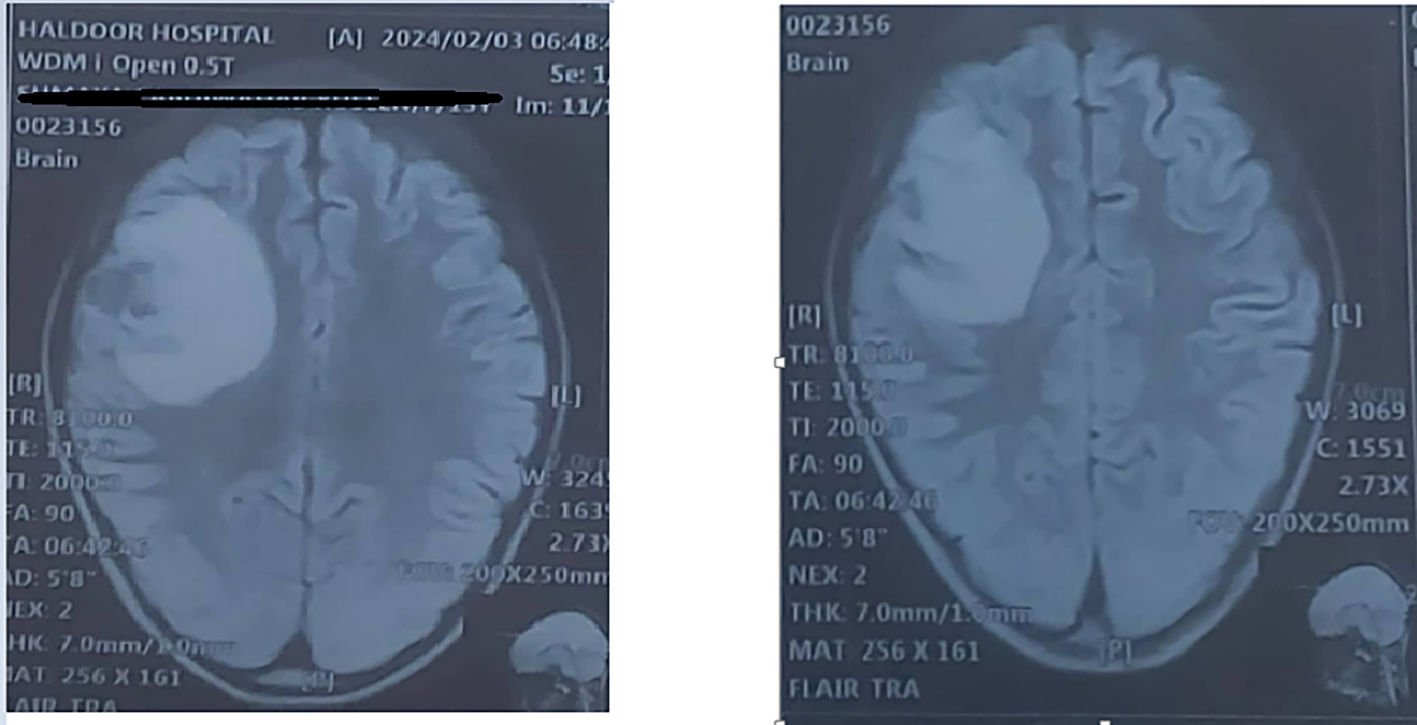
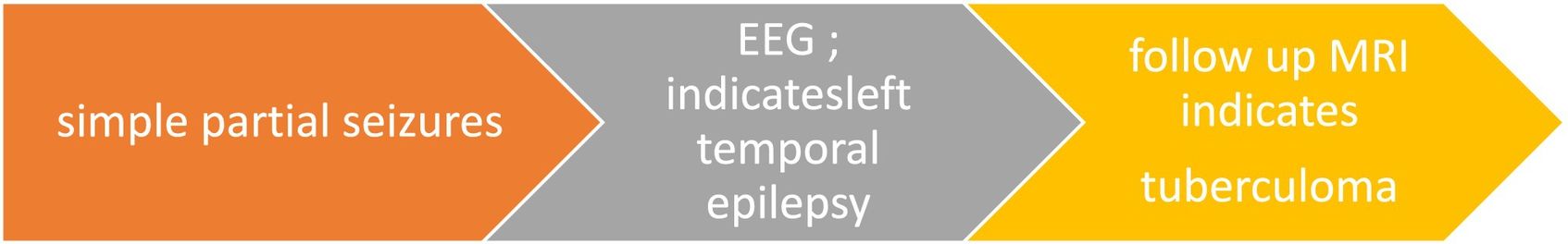
Upon physical examination, the patient demonstrated orientation to time, place, and person. Notably, there was evident left-sided facial deviation accompanied by jerky movements towards that side. Neurological examination revealed hyperreflexia and normal power, while tone remained unremarkable. Evaluation of cardiovascular, respiratory, and abdominal systems yielded no significant findings. Electroencephalography demonstrated intermittent high-amplitude sharp waves localized over the left temporal region, consistent with left temporal epilepsy. Magnetic resonance imaging revealed an impressive finding of a right-sided anterior parietal cortical and subcortical brain parenchymal intra-axial lesion, initially isodense but marginally enhancing, indicative of a tuberculoma as shown in Fig. 1.
Treatment and management were promptly initiated following the diagnosis. The patient started treatment with levetiracetam 250 mg twice daily to manage seizure activity effectively. Simultaneously, first-line anti-TB medication was initiated to address the underlying tuberculous infection. Following the initiation of therapy, the patient reported improvement, highlighting the efficacy of the treatment regimen in addressing both the neurological and infectious components of her presentation.
TimelineDiscussionTB remains a formidable global health challenge, necessitating effective management strategies to combat its high mortality rate. Tuberculomas, as rare manifestations of CNS TB, often manifest with diverse clinical symptoms, including epilepsy. Managing epilepsy, particularly in resource-limited regions like Africa, presents significant challenges compounded by TB-related complications. The co-occurrence of TB, tuberculomas, and epilepsy underscores the critical need for a comprehensive understanding and effective management strategies for neurological disorders in these contexts.4
Understanding the relationship between temporal lobe epilepsy (TLE) and TB in sub-Saharan Africa requires a multifaceted approach. While the direct link between TLE and TB may not be explicitly outlined in existing literature, related studies shed light on the broader context of infectious diseases, comorbidities, and healthcare challenges. For instance, a systematic review and meta-analysis on epilepsy comorbidities in low and middle-income countries have highlighted a significant prevalence of infections and their association with epilepsy, emphasizing the importance of comprehensive management strategies in such settings.5
Intracranial tuberculomas represent a rare complication of TB, often observed in immunocompromised individuals, particularly those infected with HIV. The incidence of intracranial tuberculomas in non-HIV-infected patients remains largely unknown, with diagnostic delays often occurring due to frequent oversight. Research has shown that cerebral tuberculomas are diagnosed in approximately 4 weeks for HIV-positive patients but may take up to 16 weeks for HIV-negative patients. A case reported by Zavasck and colleagues at The Hospital São Lucas da Pontifícia Universidade in Brazil underscores the importance of clinical suspicion, as TB was not considered until histopathological findings were available.6
The radiographical features of tuberculomas often mimic those of various infectious and non-infectious conditions, posing challenges in diagnosis. Definitive diagnosis requires intracranial biopsy followed by histopathological examination. However, the invasive nature of this diagnostic procedure limits its feasibility, especially in clinical settings.2 In our case, the combination of clinical symptoms, familial history of TB, and positive response to medication serves as strong indicators of TB presence.
Adolescence represents a period of heightened susceptibility to TB, with increased prevalence of M. tuberculosis infection and disease incidence. However, intrathoracic TB is more common in adolescents, while CNS involvement is less prevalent. Research from the USA indicates a prevalence of CNS TB of 4.1% in this specific demographic group.7
Our patient initially presented with a simple partial seizure, emphasizing the importance of considering this presentation as a marker of tuberculoma in the list of differential diagnoses (DDx) to prompt earlier treatment. Moreover, regardless of HIV status, incorporating tuberculoma into the DDx ensures comprehensive evaluation and timely intervention, ultimately optimizing patient care and outcomes.
ConclusionIn resource-limited settings like Africa, managing TB and its complications such as tuberculomas poses significant challenges. Recognizing the potential for tuberculoma, even in non-HIV patients, and including it in the list of DDx is crucial for prompt treatment. This approach ensures a comprehensive evaluation and timely intervention, optimizing patient care and outcomes in TB-endemic regions.
Ethical considerationsThe study protocol, case investigation, and consent form were thoroughly examined by the institutional review board of the College of Health Sciences at Amoud University. They granted approval for the study, along with the Ministry of Health and Borama Regional Hospital in Awdal Region, Somaliland (BRH-28/2024). Prior to participation, written informed consent was obtained from every individual involved.
FundingThe study did not receive funding.