To study if the consultation's problems classification of a fictitious case by General and Family Medicine doctors, showed the characteristics of being a mechanistic or a systemic approach. Exploratory cross-sectional observational study in a convenience sample of the General Practice/Family Medicine population, internees included, in April 2020, applying a modified real world clinical case. Central Portugal and the Autonomous Region of Azores. General Practice/Family Medicine specialists and internees. Electronic Doctors invitation to participate, anonymously, in specific doctor's social networks. A self-fulfilling questionnaire was used to verify the classification of a clinical case in Subjective, Assessment and Plan (from the SOAP methodology) with the response options of the International Classification of Primary Health Care (ICPC2) in chapters P (Psychological) and Z (Social) possible for this case. “Technicists” doctors, only classifying “P” codes and “Systemics” classifying “P+Z” or only “Z” ICPC2 codes were defined. Differences between genders, work place, being an internee or specialist and being a tutor in specialized formation were studied. A sample of 227 30% (n=68) males, specialists represented 66% (n=149), of whom 49% (n=73) were internee's tutors and 34% (n=78) were internees, was studied. In the Subjective chapter of the SOAP methodology, 44.1% (n=100) were “technicists”, for Assessment n=93 (40.8%) were “technicists” and for P chapter classification 56.8% were “technicists”. For S, A and P chapters classification there was no significant difference between the considered variables. In this sample General Practice/Family Medicine Portuguese doctors were more “systemic” for the S and A chapters of the SOAP model, And “technicists” in the P chapter.
El enfoque de la medicina centrada en el paciente (MCP) es cada vez más importante debido a su asociación de efectos positivos sobre el médico y el paciente. El presente estudio tuvo como objetivo conocer si el abordaje de un caso clínico, a través de la clasificación de problemas de consulta de un caso ficticio por médicos de Medicina General y de Familia, presenta características de abordaje mecanicista o sistémico. Estudio observacional transversal en una muestra de conveniencia de la población de Medicina General/Medicina Familiar, incluidos los internos, en abril del 2020, aplicando un caso clínico del mundo real modificado de Portugal y los especialistas en Medicina General/Medicina Familiar de Azores y de Portugal central. Especialistas en Medicina General/Medicina Familiar e internados. Los médicos fueron invitados a participar, de forma anónima, mediante invitación electrónica, ya sea en la red oficial de pasantías o en la red social de un médico específico, la red MGFamiliar. Se utilizó un cuestionario autocumplimentable para verificar la clasificación de un caso clínico en subjetivo, evaluación y planificación (de la metodología SOAP) con las opciones de respuesta de la Clasificación Internacional de Atención Primaria de Salud (CIPC2) en los capítulos P (Psicológico) y Z (Social) posible para este caso. Se definieron médicos «técnicos» solo clasificando con códigos «P» y «sistémicos» clasificando «P+Z»’ o solo con códigos ICPC2 «Z». Se estudiaron las diferencias entre géneros, lugar de trabajo, ser interno o especialista, ser tutor en formación especializada. En una muestra de 227 sujetos, 30% (n=68) varones, los especialistas representaron el 66% (n=149), de los cuales el 49% (n=73) fueron tutores internos y el 34% (n=78), internos. Para la clasificación en el capítulo subjetivo de la metodología SOAP, el 44,1% (n=100) eran «técnicos», para la evaluación n=93 (40,8%) eran «técnicos» y para la clasificación del capítulo P el 56,8% eran «técnicos». Para la clasificación de los capítulos S, A y P no hubo diferencia significativa entre las variables consideradas. En esta muestra, los médicos portugueses fueron más «sistémicos» para los capítulos S y A del modelo SOAP, es decir, tomar en consideración simultáneamente los problemas psicológicos y sociales del paciente, por lo que son holísticos. La terapéutica en el capítulo P fue técnicamente orientada.
The concept of “Health care humanization” has been discussed since the 20th century.1 It is about the potentiation of the humanitarian values between health professionals and those who seek them and is about altruism, duty performance, integrity, compassion, respect for the other and ultimately by the principle of “primum non nocere”.2,3 It also implies that the one who seeks for doctor attention is a subject with rights and autonomy and that the fair Health Professional is the one with skills to perform a humanized care.1,4
Patient Centred Medicine (PCM) is one of the ways to achieve “Health care humanization”.5 PCM is a concept and an evolving model of practicing medicine. It is based on the recognition of the Patient in its integrity, valuing its beliefs, ideas and worries, and empowering him/her, meaning the patient becomes part of the solution for his problems and not only the doctor.6 PCM implies the performance of effective communication and active listening allowing the development of a more efficient and empathic doctor-patient relationship which is also based on narrative medicine (NBM).7,8
This kind of Patient approach has advantages for the doctor and the patient with a described significant increase in physical and mental well-being, a more adequate prescription of laboratory tests, and a better Patient referral.9 More efficient symptoms resolution, better physiologic and pain control, better patient treatment acceptance, have been described.10,11 For the Doctor a sounder emotional growth is acquired once he is able to accept and deal with emotions resulting from the frequent contact with sufferance.7 This process of emotion regulation should be started as early as possible in pre-graduate teaching and continue to the life time.7
Although PCM and NBM are advocated, some studies sustain that in general a reduction on the performance of PCM exists as pre-graduate studies evolve due to lack of role models. In the immediate post-graduate, at the end of the first year, a more marked reduction in male doctors has been found.12–14
General Practice/Family Medicine (GP/FM) is the first contact of patients with the health care system.15 It is a medical speciality in Portugal with a 4 years specialization program. GP/FM specialists are well aware of the EURACT/WONCA definition for their speciality.15 And so they perceive daily cases of worried Patients for social problems, resulting in sickness16 or illness problems,17 cases that cause sufferance especially in theses pandemic times.18,19 These cases can easily be transformed by doctors in physical or mental diseases to be treated with medicines without a sound prior PCM or NBM, allowing a thorough understanding.20
This study aimed to ascertain how GP/FM specialists and internees in Central Portugal and the Autonomous Region of the Azores, Portugal, would respond to questions about a clinical case. Portuguese GP/FM in the National Health Service in mainland can work in different organizational contexts like the Personalised Care Health Unit (UCSP) and the Family Health Unit (USF) model A or B depending on the administrative and functional organizational autonomy. In the autonomous Region of the Azores they work in the Regional Health Service in Health Centres (HC). The main difference between UCSP/HC and USF is that in the USF model doctors, nurses and administrative staff get together and engage in a contract with health authorities to accomplish an health assistential contract to a specific population. Model A and B differ in team growth and payment model with a coordinator but without Top/Bottom structure. UCSP and HC have a traditional Top/Bottom structure.21,22 In mainland Portugal, there are 5 Health Administrative regions.
ICPC2 is a classification system, created by WONCA and recognized by the WHO, that allows classification of reason for encounter, medical diagnostics and procedures in a bi-axial structure, letters referring to organ, with chapters (systems) and components, seven for each chapter classifying symptoms, diagnostics and procedures.23,24
The pertinence and importance of this study are linked to the need of obtaining knowledge about how doctors reflect, using their knowledge and practice about PCM and NBM in their usual work when making e.registrations and e.classifications using ICPC223,24 on the SOAP methodology25 for consultation. In the ICPC2, chapters P reflects psychological and psychiatric problems and Z chapters deals with the classification of social problems that patients can present and that can act as a trigger for sufferance.23,24 ICPC2 is the most used classification system in the Portuguese General Practice/Family Medicine setting official e.registrations program in the Portuguese National Health System, the “SClinico”. This study intended to know whether GP/FM tended to have a technicist approach (more reasoning in disease) or a systemic one (simultaneously reasoning the patient and the cause of his problems). Medicines can have little efficiency and tend to lead to addiction with later difficulty to deprescribe them.26–28
It was hypothesized that tutor specialists, older non-tutor specialists and 3rd and 4th year internees were more systemic, choosing simultaneous ICPC2 classifications in the Z (Social) and P (Psychologic) chapters.
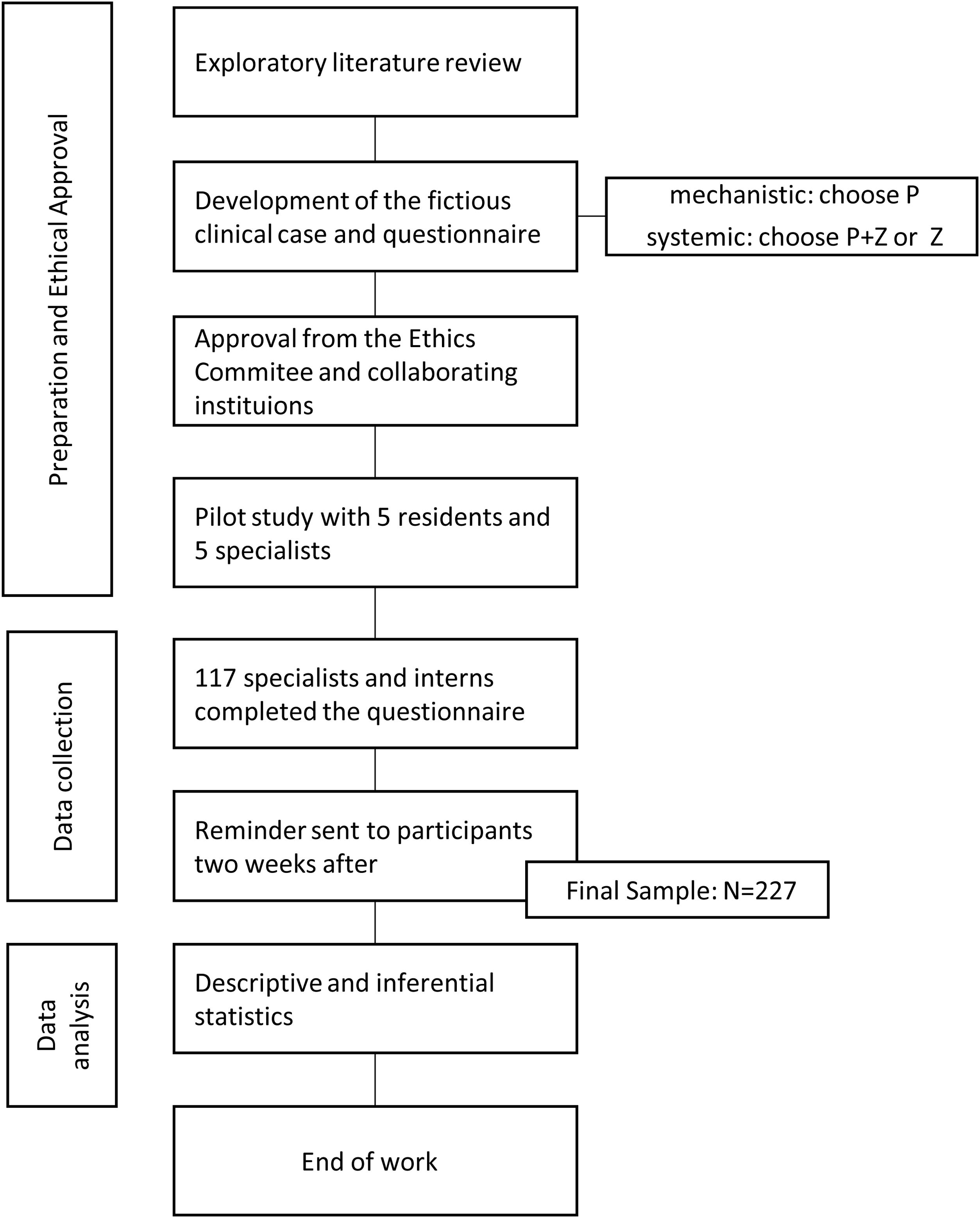
MethodsAn exploratory, cross-sectional observational study was performed in a convenience sample of the population of GP/FM specialists and internees of the Central Region of Portugal and of the Autonomous Region of Azores in April 2020, after Ethic Committee approval and with no financial fundings.
A fictional clinical case was made by the authors and adapted to the objectives to be analyzed. (Fig. 1)
The questionnaire intended to collect information about how doctors made e.ICPC2 classifications in Subjective, Assessment and Plan (“S”, “A” and “P” of the SOAP method), P and Z chapters classifications being listed and allowing other classifications if intended necessary by the responder in blank lines.23,25
We defined two kinds of doctors: The “technicists” only classifying with P codes in S, A and P of ICPC2 and “systemics” classifying “P+Z” or only Z.
After a small introductory text a written consent for participation was presented. The questionnaire included knowledge about sociodemography: years of medicine practice, gender, kind of primary health care practice, being a specialist or an internee, a tutor in internship and for internees the attended year.
Through specific and dedicated professional networks the invitation was made sending the link of the on-line questionnaire. Two reminders were made two weeks apart.
Sample size was calculated for an error margin of 5% and interval confidence of 95%, for a population of n=2200 using an online calculator. [https://comentto.com/calculadora-amostral/]
The Statistical Package for the Social Sciences (SPSS®) version 25.0 for Windows was used to perform descriptive and inferential statistics. Nonparametric tests Mann–Whitney U and Kruskall–Wallis were used for numeric non-normal distributed variables and for ordinal variables. A p value of <0.001 was defined for significance.
A printed pre-test was made with 5 GP/FM specialist and 5 GP/FM internees out of the population to be studied, to know acceptability, content understanding and time to fill-in.
ResultsCalculated sample size was of n=222 and a sample of n=227 was collected. The pilot study showed good acceptability, content understanding and a mean time of 7min to fill-in the questionnaire.
In this sample 30% (n=68) were males, 15% (n=33) worked in a UCSP, 18% (n=41) in a Health Centre in Azores, 34% (n=77) in Family Health Unit model A (USFA) and 33% (n=76) in a Family Health Unit model B (USFB). Specialists represented 66% (n=149), of whom 49% (n=73) were tutors for internees, and 34% (n=78) were internees. A proportion of 24% (n=19) of the internees was attending the 1st year of GP/FM residence, 18% (n=14) was attending the 2nd year, 28% (n=22) the 3rd and 30% (n=23) the 4th.
Years of Clinical Practice were of 37% (n=83) for ≤ 5 years, 27% (n=62) between 6 and 10 years, 14% (n=33) between 11 and 15 years, 7% (n=15) between 16 a 25 years and 15% (n=34) ≥26 years.
No significant differences by gender were found for Years of Clinical Practice (p=0.063), Type of Health Unit of work (p=0.944), being a specialist or an internee (p=0.184) and year of internship (p=0.976), and being a tutor (p=0.191).
For the classification in the Subjective chapter of the SOAP methodology, 44.1% (n=100) was only P Chapter classification. The P+Z and the only Z classification were the remainder 55.8%, indicating a systemic prevalence prevailing.
For the suggested ICPC2 classifications, 443 were made in chapter P and 148 in the Z chapter, more than one classification being possible.
Table 1 refers the specific chosen classifications. The most chosen ones were P27 (Fear of mental disorder) with 30.3% and P04 (Feeling/behaving irritable/angry) with 27.0%. For the Z chapter the more frequent chosen was Z05 (Work problem) with 43.2%, followed by Z06 (Unemployment problem) and Z27 (Fear of social problem) both with 28.4% of frequency.
ICPC2 P and Z classifications in the S chapter of the SOAP methodology.
| ICPC2 Chapter | ICPC2 option | n | % |
|---|---|---|---|
| P | P01 | 72 | 16.6 |
| P02 | 46 | 10.6 | |
| P03 | 67 | 15.5 | |
| P04 | 117 | 27.0 | |
| P27 | 131 | 30.3 | |
| Total | 433 | 100 | |
| Z | Z05 | 64 | 43.2 |
| Z06 | 42 | 28.4 | |
| Z27 | 42 | 28.4 | |
| Total | 148 | 100 |
Note: P01: Feeling anxious/nervous/Tense; P02: Acute Stress reaction; P03: Feeling depressed; P04: Feeling/Behaving instable/Angry; P27: Fear of mental disorder; Z05: Rork problem; Z06: Unemployment problem; Z27: Fear of social problem.
Using nonparametric statistics no significant differences were found for gender (p=0.532), type of health care unit (p=0.274), years of practice (p=0.022), year of internship (p=0.090), being internee or a specialist (p=0.039) and being a tutor (p=0.583).
For the subjects that only chosen P ICPC2 classifications, P01 had a frequency of 40.0%, P02 of 9.0%, P03 of 13.0%, P04 of 18.0% and P27 of 20.0%. In the cases that had chosen P+Z classification the P chapter ICPC2 classifications frequencies were of 19.0%, 13.0%, 13.0%, 26.0% and 29%, respectively, Table 2.
ICPC2 classification in S of the Soap model according to only P chapter or P+Z chapter classifications.
| ICPC2 classification | Signs and symptoms | |||||
|---|---|---|---|---|---|---|
| P01 | P02 | P03 | P04 | P27 | Total | |
| P chapter only | ||||||
| n | 97 | 21 | 33 | 44 | 50 | 245 |
| % | 40.0 | 9.0 | 13.0 | 18.0 | 20.0 | |
| P+Z simultaneously | ||||||
| n | 50 | 34 | 34 | 67 | 76 | 261 |
| % | 19.0 | 13.0 | 13.0 | 26.0 | 29.0 | |
Note: P01: Feeling anxious/nervous/Tense; P02: Acute Stress reaction; P03: Feeling depressed; P04: Feeling/Behaving instable/Angry; P27: Fear of mental disorder.
For SOAP Assessment suggested classifications in “Assessment” 226 doctors responded (99.6%). For n=93 (40.8%) a single option in ICPC2 chapter P was marked, for n=2 (0.9%) a single one in the Z ICPC2 chapter was marked and for n=131 (57.5%) there was simultaneous P and Z ICPC2 Chapters classification, meaning a technicist approach by 40.8%
According to Table 3, for 226 doctors, and for the suggested Classifications, n=372 classifications were made in ICPC2 P Chapter and n=162 were made in the Z one. For the P Chapter classifications, the most chosen ones were P02 (30.6%) (Acute stress reaction), and P27 (25.3%) (Fear of mental disorder). For Z chapter was Z05 (43.2) (Work problem). Classifications Z06 and Z27 represent an aggregate of 52.4% of the Z answering options.
ICPC2 P and Z suggested classifications in the A chapter of the SOAP methodology.
| ICPC2 chapter | ICPC2 option | Absolute frequency | Relative frequency |
|---|---|---|---|
| P | P01 | 24 | 6.5 |
| P02 | 114 | 30.6 | |
| P03 | 26 | 7.0 | |
| P04 | 25 | 6.7 | |
| P27 | 94 | 25.3 | |
| P74 | 32 | 8.6 | |
| P76 | 50 | 13.4 | |
| P99 | 7 | 1.9 | |
| Total | 372 | 100 | |
| Z | Z05 | 70 | 43.2 |
| Z06 | 43 | 26.5 | |
| Z27 | 42 | 25.9 | |
| Total | 162 | 100 |
Note: P01: Feeling anxious/nervous/Tense; P02: Acute Stress reaction; P03: Feeling depressed; P04: Feeling/Behaving instable/Angry; P27: Fear of mental disorder; P74: Anxiety disorder/anxiety state; P74: Depressive disorder; P99: Psychological disorders/other. Z05: Work problem; Z06: Unemployment problem; Z27: Fear of social problem.
Using nonparametric tests no differences were found in the classification by gender (p=0.751), type of health care unit (p=0.101), years of practice (0.769), year of internship (0.741), being internee or a specialist (p=0.006) and being a tutor (p=0.495).
In the specific classification of diagnosis (Table 4), for the subjects that only chosen P ICPC2 classifications P27, P74 and P76 had a frequency of 32.0%, contrasting to a frequency of 18.0% when P+Z were classified.
ICPC2 classification in A of the Soap model according to only P chapter or P+Z chapter classifications and for the specific chapters of signs and symptoms and diagnostic.
| ICPC2 classification | Signs and symptoms | Diagnostics and diseases | ||||||
|---|---|---|---|---|---|---|---|---|
| P01 | P02 | P03 | P04 | P27 | P74 | P76 | Total | |
| P chapter only | ||||||||
| n | 8 | 40 | 10 | 10 | 37 | 14 | 35 | 154 |
| % | 5.0 | 26.0 | 6.0 | 6.0 | 24.0 | 9.0 | 23.0 | |
| P+Z simultaneously | ||||||||
| n | 21 | 71 | 19 | 17 | 68 | 23 | 18 | 237 |
| % | 9.0 | 30.0 | 8.0 | 7.0 | 29.0 | 10.0 | 8.0 | |
Note: P01: Feeling anxious/nervous/Tense; P02: Acute Stress reaction; P03: Feeling depressed; P04: Feeling/Behaving instable/Angry; P27: Fear of mental disorder; P74: Anxiety disorder/anxiety state; P74: Depressive disorder.
For the ICPC2 classifications in the SOAP Plan chapter, for 56.8% of the doctors there were only P chapter classifications, for 1.3% there were only Z chapter classifications and for 40.5% there were simultaneous P and Z chapter Classifications. A technicist approach was verified for 56.8%.
According to Table 5 a total of 423 classifications were made in ICPC2 P chapter and 139 in the Z one. As for its distribution and for the P ICPC2 chapter, the most chosen options were P58 (36.9%) (Therapeutic counselling/therapeutic listening) and P45 (28.9%) (Observation/health education/counselling/diet). For the Z chapter Z45 was the most frequent (36.0%) (Observation/health education/counselling/diet) and Z58 (33.1%) (Therapeutic counselling/therapeutic listening), the second one most frequent. Drugs prescription (Z50) was classified by 1.4% of the respondents.
ICPC2 P and Z suggested classifications in the P chapter of the SOAP methodology.
| ICPC2 chapter | ICPC2 Classification | N | % |
|---|---|---|---|
| P | P45 | 122 | 28.9 |
| P48 | 93 | 22.0 | |
| P50 | 52 | 12.3 | |
| P58 | 156 | 36.9 | |
| Total | 423 | 100 | |
| Z | Z45 | 50 | 36.0 |
| Z48 | 41 | 29.5 | |
| Z50 | 2 | 1.4 | |
| Z58 | 46 | 33.1 | |
| Total | 139 | 100 |
Note: P45: Observation/Health education/Counselling/ Diet; P48: Clarification/reason for encounter/Discussion; P50: Prescribing/Prescription/injection; P58: Therapeutic counselling/Therapeutic listening. Z45: Observation/Health education/Counselling/Diet; Z48: Clarification/reason for encounter/Discussion; Z50: Prescribing/Prescription/injection; Z58: Therapeutic counselling/Therapeutic listening.
Using nonparametric tests no differences were fund for gender (p=0.248), type of health care unit (p=0.698), years of practice (0.260), year of internship (0.339), being an internee or a specialist (p=0.392) and being a tutor (p=0.184).
For the subjects that only chosen P ICPC2 classifications in the Plan chapter, P58 “Therapeutic counselling/therapeutic listening” had a frequency of 32.5%, and “Observation/Health Education/Counselling/diet” a 28.5% of frequency. In the case of P+Z classification, frequencies were of 41.3% for “Therapeutic counselling/therapeutic listening” and 25.6% for “Observation/Health Education/Counselling/diet” (Table 6).
ICPC2 classification in A of the Soap model according to only P chapter or P+Z chapter classifications and for the specific chapters of signs and symptoms and diagnostic.
| ICPC2 classification | Plan | ||||
|---|---|---|---|---|---|
| P45 | P48 | P50 | P58 | Total | |
| P chapter only | |||||
| n | 70 | 68 | 28 | 80 | 246 |
| % | 28.5 | 27.6 | 11.4 | 32.5 | |
| P+Z simultaneously | |||||
| n | 44 | 40 | 17 | 71 | 172 |
| % | 25.6 | 23.3 | 9.9 | 41.3 | |
Note: P45: Observation/Health education/Counselling/Diet; P48: Clarification/reason for encounter/Discussion; P50: Prescribing/Prescription/injection; P58: Therapeutic counselling/Therapeutic listening. Z45: Observation/Health education/Counselling/Diet.
As ICPC2 added classifications we found 3 (1.3%) in the Plan and Procedures SOAP chapter, and none in the remaining SOAP chapters.
DiscussionThis study aimed to understand how GP/FM doctors both internees or specialists, would classify a clinic case according to the ICPC2 in the SOAP model. The issue was not about the righteousness of the chosen classifications, but rather about the ambience for the choice of classifications. It was pre-defined that those who would choose only to classify P ICPC2 chapter would be classified as “technicists” as they would be more disease and doctor matters centered. Such would not be mandatorily wrong and could reflect several aspects of pre-graduation, initial internship study or experience and continuous medical education and continuous medical development, and even the work ambience like the one of the type of Primary Care Unit. The “systemic” ones would tend to simultaneously classify P and Z or only Z and they tend to reflect on the case and its causes.
GP/FM has an “umbrella” core of knowledge and specific ways of dealing, caring and solving problems.5,7,8,15,16,20,23,25
This clinical case presented someone with complains of not feeling well, knowing the cause of his sufferance, being afraid of developing dementia like his mother, not wishing to develop anxiety or depression and with no intension of being medicated although he thought the doctor should know better what to do. Several ICPC2 P and Z chapter classifications were suggested, and subjects could choose “other classification” as a free one if they needed, for each of the SOAP consultation model chapters, gathering information for the best management.29,30
With no other known articles discussing features as these, the results of the present study reveal different pictures for each of the SOAP model chapters with possible ICPC2 classification.
In the S SOAP chapter, 44.1% of this convenience sample was “technicist” and the ICPC2 more frequent classification was “Fear of mental disorder” followed by “Feeling depressed”. If the P ICPC2 chapter was the only one classified than “Feeling anxious/nervous/tens” would be the most chosen one. If the choice would be of simultaneously classifying P+Z, then the most frequent chosen answer was “Fear of mental disorder”. This is an interesting change in classification meaning different approaches to the classification of reason for encounter, even though no significant differences were found comparing for the considered variables.
For the SOAP A chapter, 40.8% of the respondents made classifications choice as “technicist” doctors, a somehow lower frequency than the one found for the S SOAP chapter. The specific ICPC2 P chapter classifications for diseases represented 23.9%, meaning that many doctors did not feel at ease with making an immediate diagnosis. And if the P ICPC2 chapter was the only one classified, the specific classifications in diagnosis (P27, P74 and P76) frequency would be of 32.0%, being of 18.0% if a P+Z classification was made. This analysis distinctly shows the difference between the two types of doctors, with the “systemic” ones not making as much “Depressive disorder” classifications as “technicist” doctors. Even though there are no difference between the two types of doctors for “Anxiety disorder/anxiety state” classifications.
“Systemic” doctors tend to keep their ICPC2 Classifications in the S and A SOAP chapters, on the contrary of the “technicist” ones.
For the SOAP Plan chapter, a “technicist” approach was verified for 56.8% of the respondents although the classification “50, prescription” was the least one used. The more “systemic” doctors tended to use more the “P58” “Therapeutic counselling/Therapeutic listening” than the “technicists” ones.
Overall these results mean that General Practice/Family Medicine doctors have a tendency to be “systemic” in S and A but not in P of the SOAP model. This can indicate that the therapeutics is still somehow technically oriented. For S and A the differences in ICPC2 P chapter classification between “technicist”/“systemic” clearly deserve attention, and the reason why even “systemic” doctors tend to be “technicists” in the Plan chapter of the SOAP Model is a question to be further studied. Therefore the WONCA-Europe Definition of General Practice.31
Even though there seems to be room for Continuous Medical Education and, especially Continuous Medical Development.32
This “exploratory” study has some limitations like the convenience sample obtained in professional social net-works, but the will to have a larger number of respondents in short time and getting answers from doctors responding at their own time and place took us to this way of performing the study. Another limitation is that we do not know what any one of the respondents knew about ICPC2 classification. And the last limitation is about the convenient technicist/systemic definition we have explained earlier. Psychiatrists also deal with this kind of problems but the lack of this speciality to deal with ICPC2 made it difficult to make comparisons.
The quality of ICPC2 classifications not being at stake must be considered as a systematic error.
So it can be concluded that in this sample of GP/FM Portuguese doctors, both internees and specialist, a more “systemic” classification for the S and A chapters of the SOAP consultation model was found, meaning simultaneously taking in consideration Psychological and Social patient's problems. For the P SOAP a generalized “technicist” approach was verified.
Conflict of interestAll authors disclose any financial and personal relationships with other people or organizations that could inappropriately influence (bias) their work.
This research was not granted and was interely suported by the authors who made it in their own non-working time.