To analyze the evolution of the stages of CKD and the progression of the estimation of glomerular filtration rate (eGFR) in patients with newly diagnosed hypertension.
DesignRetrospective cohort.
SiteFamily Medicine Unit No. 31, Mexican Social Security Institute, Mexico City.
ParticipantsPatients with hypertension who have been diagnosed in primary care and have developed chronic kidney disease.
Main measurementsThe eGFR was calculated with the CKD Epi formula in three moments, the first measurement was at the time of diagnosis of hypertension, the second measurement was made when it arrived a change in CKD stage and the last one at the end of the study, with which the evolution time from one stage to another was obtained, as well as the drop in eGFR.
ResultsThe sample consisted of 207 electronic health records of patients, with an average follow-up of 10.2 years from the moment of diagnosis of hypertension until the end of the study. The average time to go from one baseline stage of CKD to another was 7 years (average decline in eGFR of 5.8ml/min/year) and to have a second stage change was 3.2 years (average decline in eGFR of 6.8ml/min/year), with a statistically significant repeated measures ANOVA (p<0.001).
ConclusionsPatients with newly diagnosed hypertension remain longer in the initial stages of CKD, to later evolve and change more quickly.
Analizar la evolución de los estadios de la enfermedad renal crónica (ERC) y la progresión de la estimación de la tasa de filtración glomerular (eTFG) en pacientes con hipertensión arterial de nuevo diagnóstico.
DiseñoCohorte retrospectiva.
EmplazamientoUnidad de Medicina Familiar N.° 31, Instituto Mexicano del Seguro Social, Ciudad de México.
ParticipantesPacientes hipertensos que hayan sido diagnosticados en atención primaria y hayan desarrollado ERC.
Mediciones principalesLa eTFG se calculó con la fórmula CKD Epi en 3 momentos. La primera medición fue al momento del diagnóstico de hipertensión arterial, la segunda medición se realizó cuando se presentó un cambio de estadio de la ERC y la última, al final del estudio, con el que se obtuvo el tiempo de evolución de un estadio a otro, así como el descenso de la eTFG.
ResultadosLa muestra estuvo constituida por 207 historias clínicas electrónicas de pacientes, con un seguimiento promedio de 10,2 años desde el momento del diagnóstico de hipertensión arterial hasta el final del estudio. El tiempo promedio para pasar de una etapa inicial de la ERC a otra fue de 7 años (disminución promedio de la eTFG de 5,8ml/min/año) y para tener un cambio de segunda etapa fue de 3,2 años (disminución promedio de la eTFG de 6,8ml/min/año), con un ANOVA de medidas repetidas estadísticamente significativo (p < 0,001).
ConclusionesLos pacientes con hipertensión arterial de nuevo diagnóstico permanecen más tiempo en los estadios iniciales de la ERC, para luego evolucionar y cambiar más rápidamente.
Worldwide, there is an exponential rise in the incidence and prevalence of Chronic Kidney Disease (CKD), to such an extent that it is considered a public health problem1; there is a close bidirectional relationship between CKD and arterial hypertension, therefore that adequate control of hypertension can prevent or delay its evolution.2
In high- and middle-income countries, the main causes of CKD are diabetes and high blood pressure; According to the World Health Organization, it estimated that in 2012 it was the cause of death between 1 and 5% worldwide and according to projections of the Global Health Observatory it will be the cause of 14 of 100,000 deaths by the year 2030.3 The information from the prevalence and incidence of CKD is not very exact, since it varies globally; the greatest difficulties in knowing the prevalence, incidence, and progression of CKD are due to the heterogeneous populations; despite this, there are data in high-income countries where the prevalence is around 11% and varies around the world around 8–16% in the general population, being those over 65 years the group with the highest prevalence with data ranging from 23.4 to 35.8%.4,5
At the time of detection of CKD, 90% of the cases are in early stages 1–3 according to the KDOQI (Kidney Disease Outcomes Quality Initiative) classification, which are asymptomatic.6 Therefore, the study of the causes and evolution of CKD with concomitant and causative diseases, such as arterial hypertension. The progression of CKD with hypertension is associated with poor blood pressure control7; there are examples where a decrease in glomerular filtration rates (GFR) was reported as there was less control of systolic blood pressure (SBP)8–10; therefore, the control of arterial hypertension plays an important role in the follow-up of newly diagnosed patients.
The progression of CKD and the increase in creatinine levels in patients with arterial hypertension do not become consistent over time.11 At the clinical level, few studies have investigated the evolution of CKD by stages in patients with arterial hypertension; there are some reports where patients with CKD with stages 3a and 3b progress to stages 4 or 5 in an average of 10 years, without taking into account the underlying diseases, with variable results.12,13 The prevalence or progression in CKD in patients with hypertension is greater than those without the disease,14 according to the Annual Report of the US Renal Data System (2013) attributed up to 25% of CKD cases to arterial hypertension.15 The main objective of this study was to analyze the evolution of the CKD stage and the progression of eTFG in patients with newly diagnosed arterial hypertension.
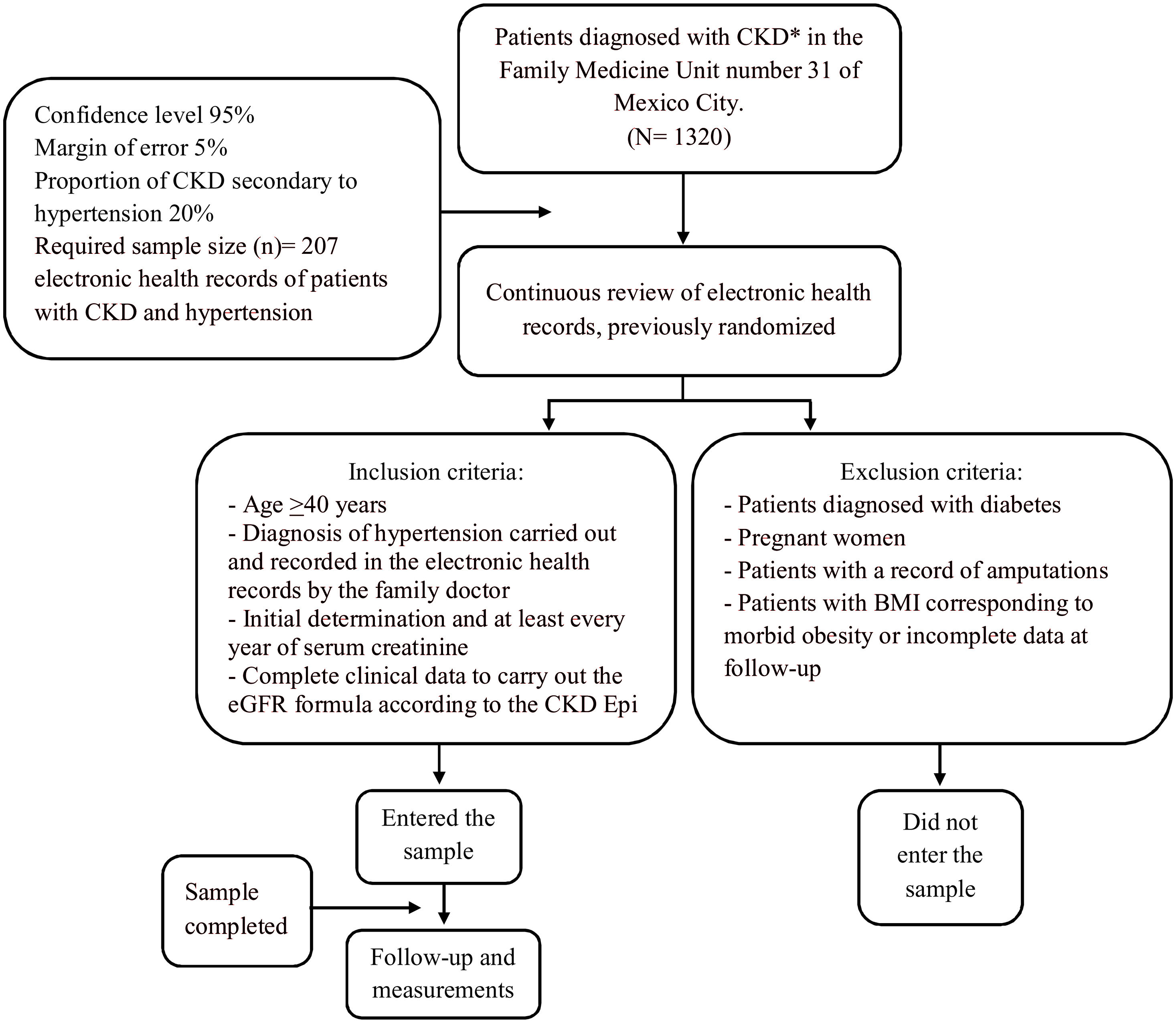
MethodsStudy design and participantsAt the time of the study, in the Primary Care Unit there was a census of 1320 patients with a diagnosis of CKD (N), the sample was calculated using the formula of proportions, taking into account that 20% of patients with CKD it is secondary to hypertension, leaving the sample in 207 patients (n); of the census of patients with CKD, a simple randomization of the population was carried out, applying the selection criteria, they were chosen consecutively until the sample was completed. This is a retrospective cohort of patients with hypertension from the moment of diagnosis of the disease, in a Family Medicine Unit of Mexico City of the Mexican Institute of Social Security in 2019, the selection criteria were: age >40 years, having been diagnosed for the first time with arterial hypertension (the diagnosis was made by the family medicine specialist and recorded in the clinical file), initial determination and at least every year of serum creatinine and complete clinical data to carry out the eGFR formula according to the CKD Epi; patients diagnosed with diabetes, pregnant women, with amputations, morbid obesity or incomplete data at follow-up, were excluded (Fig. 1).
VariablesThe variables taken into account were age (over 40 years), sex. To calculate the eGFR, the formula proposed by CKD Epi was used, taking into account the height, weight and calculation of body mass index (BMI) and serum creatinine levels (the laboratory tests for the determination of serum creatinine were performed in the Family Medicine Unit) for the classification by stages of CKD.
The aforementioned variables were followed over time from the diagnosis of arterial hypertension; three measurements were recorded in each patient. To know the time difference (years) between one and the other, the age of the patients was taken into account. The first measurement was made at the time of diagnosis of arterial hypertension (baseline measurement). The second measurement was carried out when a change in CKD stage was detected with respect to the baseline measurement (intermediate measurement). The last measurement was carried out with the last data recorded in the clinical record at the time of the study (final measurement or last measurement). In this way, the record of measurements was determined by the progression from one stage to another.
Statistical methodsThe descriptive statistical analysis for the quantitative variables was carried out with the determination of means and their respective standard deviation, while the qualitative variables, frequencies and percentages with a 95% CI were used. We calculate the eGFR with the equation proposed by the CKD Epi for its subsequent classification into stages. Once having the means in the 3 measurements, a repeated measures ANOVA test was performed to find out if the difference in means was statistically significant, with a partial squared Eta calculation and Mauchly's sphericity test to determine if the assumption of sphericity of variance was fulfilled, when seeing that this assumption was not fulfilled, the correction was chosen with the Huynh–Felt test. The Bonferroni post hoc test was performed to check the statistical significance in the interaction between all groups. Statistical significance was determined at 0.05%.
ResultsThe study included 207 patient files, with an average follow-up of 10.2 (±4.5) years from the diagnosis of arterial hypertension. The sample consisted of 132 male and 75 female patients (63.8%, 57.2, 70.3 95% CI and 36.2%, 29.7, 42.8 95% CI, respectively), at the beginning of the study, the patients had a mean age of 62.6 years (±9.3) and at the end of 72.9 (±9.3) years and more than half were male. The mean difference from the baseline to the intermediate measurement was 7 years and from the intermediate measurement to the last, it was 3.2 years. Regarding the body mass index (BMI), the group with the highest prevalence was the overweight at the time of the three measurements. The decrease in eGFR by CKD Epi at the three moments of the calculation were noticeable; from the first calculation to the second, the decrease was 28.3ml/min/1.73m2 and from the second estimate to the third it was 14.6ml/min/1.73m2 (Table 1).
Characteristics of the patients at different times of the eGFR (n=207).
| Clinical features | Baseline measurement | Intermediate measurement | Last measurement |
|---|---|---|---|
| Age, mean (SDa), years | 62.6 (± 9.3) | 69.6 (± 9.3) | 72.7 (± 9.2) |
| BMI (SDa) | 27.2 (± 3.3) | 27.1 (± 3.3) | 27.1 (± 3.3) |
| Normal | 54 (26.1%) | 54 (26.1%) | 54 (26.1%) |
| Overweight | 115 (55.6%) | 116 (56%) | 116 (56%) |
| Obesity | 38 (18.4%) | 37 (17.9%) | 37 (17.9%) |
| eGFR CKD Epi | 80.9 (± 17) | 52.6 (± 18.8) | 38 (± 18.3) |
| Stage 1 | 63 (30.4%) | 2 (1%) | 0 |
| Stage 2 | 123 (59.4%) | 75 (36.2%) | 20 (9.7%) |
| Stage 3a | 12 (5.8%) | 66 (31.9%) | 60 (29%) |
| Stage 3b | 6 (2.9%) | 37 (17.9%) | 67 (32.4%) |
| Stage 4 | 3 (1.4%) | 15 (7.2%) | 28 (13.5%) |
| Stage 5 | 0 | 12 (5.8%) | 32 (15.5%) |
At the time of diagnosis of arterial hypertension (baseline measurement), the patients who were found in stage 1 (n=63), took 7.8 years on average to progress to other stages (intermediate measurement), while those who started with a stage 2 (n=123) took 6.9 years on average and patients who were at baseline in stages 3a, 3b and 4 (n=24) together, took 4 years to progress to other stages. The average time from initial to intermediate measurement is shorter in patients with more advanced stages. It is worth mentioning that 34 patients (16.4%) had no change in stage from the intermediate to the last measurement (Table 1).
The mean annual decrease in eGFR by CKD Epi from the initial to the intermediate measurement was 5.8ml/min/year, while, from the intermediate to the final measurement, it was 6.8ml/min/year, that is, it was slower at first; This pattern was repeated in the case of males, unlike females, where the initial measurement was faster than the subsequent one.
The patients at the time of diagnosis of hypertension (baseline measurement) who were found in stage 1 (n=63) progressed to the intermediate measurement to stage 2 in 60.3% and in 22% to 3a and when the last eGFR was obtained more than 50% were found in stages 3a and 3b. The patients who started with stage 2 (n=123), in the intermediate measurement 30% remained in 2, 50% progressed to stage 3 and for the last measurement 36% were found in 3b, 11% in stage 4 and 16% to stage 5. The patients who were in stage 3a in the initial measurement (n=12), 66% advanced to a 3b, for the last calculation, 50% remained in 3b and 33% changed to stage 4. To check whether the differences in the eGFR values by CKD Epi at the 3 moments (initial, intermediate and last) were statistically significant, the repeated measures ANOVA test was used, in which a difference in the variances was statistically found. significant, with a p<0.001 (Table 2).
Follow-up, comparison and distribution of patients by initial stage of CKD.*
| Stage in baseline measurement | Distribution of patients in the intermediate measurement | Distribution of patients in the last measurement |
|---|---|---|
| Frequency (%) | Frequency (%) | |
| Stage 1 patients (n=63) | ||
| 1 | 2 (3.2) | 0 |
| 2 | 38 (60.3) | 14 (22.2) |
| 3a | 14 (22.2) | 22 (34.9) |
| 3b | 6 (9.5) | 16 (25.4) |
| 4 | 2 (3.2) | 6 (9.5) |
| 5 | 1 (1.6) | 5 (7.9) |
| Total | 63 (100) | 63 (100) |
| Stage 2 patients (n=123) | ||
| 2 | 37 (30.1) | 6 (4.9) |
| 3a | 50 (40.7) | 38 (30.9) |
| 3b | 21 (17.1) | 45 (36.6) |
| 4 | 8 (6.5) | 14 (11.4) |
| 5 | 7 (6.5) | 20 (16.3) |
| Total | 123 (100) | 123 (100) |
| Stage 3a patients (n=12) | ||
| 3a | 2 (16.7) | 0 |
| 3b | 8 (66.7) | 6 (50) |
| 4 | 1 (8.3) | 4 (33.3) |
| 5 | 1 (8.3) | 2 (16.7) |
| Total | 12 (100) | 12 (100) |
| Stage 3b patients (n=6) | ||
| 3b | 2 (33.3) | 0 |
| 4 | 3 (50) | 4 (66.7) |
| 5 | 1 (16.7) | 2 (33.3) |
| Total | 6 (100) | 6 (100) |
| Stage 4 patients (n=3) | ||
| 4 | 1 (33.3) | 0 |
| 5 | 2 (66.7) | 3 (100) |
| Total | 3 (100) | 3 (100) |
Different studies have analyzed the evolution of renal function in patients with chronic diseases, giving greater importance to diabetes as a triggering factor or associated with its evolution, in some the evolution or progression of eGFR over time has simply been studied without considering some specific disease.11,13,16 In our study, an analysis of the evolution of CKD was carried out in patients with hypertension as the main risk disease, based on its diagnosis made at the first level of care, where it was observed that In an average of 7 years, they lost 28.3ml/min/1.73m2 in the eGFR and in an average 3.2 years, the loss was 14.6ml/min/1.73m2. A differential feature of the present study was the CKD staging at the time of diagnosis of arterial hypertension, where almost 60% of the patients were already in stage2 and with an average eGFR of 80.9ml/min/1.73m2 and almost a 10% with some stage between stage 3a and 4, which leads to suppose that these patients had some previous condition that conditioned the presence of CKD (underdiagnosed arterial hypertension of several years of evolution, presence of previous kidney disease, mainly an over-aggregated glomerulopathy, which conditioned an important renal deterioration arriving with less than 60ml/min of eGFR and with a potential secondary arterial hypertension, which was not ruled out in the present study). It should be noted that CKD does not present symptoms, but until intermediate stages with nonspecific biochemical conditions, so patients with initial stages do not go to medical services for care.1 Usually when it is diagnosed and cared for, it is the result of a complication of another disease or an incidental condition; it is likely that most patients at the time of being diagnosed with hypertension already have some degree of CKD, so that timely diagnosis programs are even more necessary and strengthened, in the same way, it is essential that in patients with newly diagnosis of hypertension is intentionally looking for an adjacent cause of CKD.17
There are studies in which the evolution by stage of CKD was analyzed, however, the eGFR data or stage were not taken into or only patients with a specific CKD stage were taken account from the diagnosis of the underlying diseases (such as diabetes or hypertension).12,18,19 Another important aspect of our study is the analysis of CKD stages at the onset of hypertension and its redistribution over time. At the time of the baseline measurement, almost 90% of the patients were distributed in stage1 and 2 (30.4 and 59.4% respectively), at the time of the second measurement this distribution changed completely, where patients with stage 1 only represented in 1%, the majority were in stage 2, 3a, 3b (36.2, 31.9 and 17.2% respectively) and more importantly, there were already patients in stage 4 and 5 (7.2 and 5.8% respectively); 3.2 years later, more than 60% were in stage 3a and 3b, and almost 30% in stage 4 (13.5%) and 5 (15.5%), the stage changes presented from the intermediate measurement to the last one were faster than at the beginning, which can be interpreted as a rapid progression, information that acquires importance for the First-level care physician, since it only takes 10.2 years on average for a patient with a diagnosis of hypertension to reach advanced stages of CKD. This information opens the possibility of analyzing whether the diagnosis and therapeutic management of hypertension and CKD is timely by the first level of care,20 since, as is known, primary care is essential in the management of chronic degenerative diseases and the one responsible for serving between 80 and 85% of the entire population.21,22
It is important to mention that stage progression may be due to the aging of the population studied, since the prevalence of advanced stages of CKD increases with age,22 this condition may even be considered “expected” due to aging or renal senescence, where it is counted with a smaller number of functional glomeruli due to nephrosclerosis, with compensatory hypertrophy of the remaining nephrons, decreased cortical volume and the presence of age-associated renal cysts that are somewhat physiological and also associated with older age.23
Limitations1) The optimization of antihypertensive treatment was not investigated, therefore, it was not sought to associate the evolution of CKD with hypertensive control, 2) the presence of underlying causes of CKD that were not clinically evident and that undoubtedly can generate confusion about the evolution of CKD; Since, in order to generate causal inferences about the evolution of CKD secondary to hypertension, a specific histopathological diagnosis per patient must be had, which allows confirming the diagnosis of hypertensive nephropathy, which is not possible at the first level of care. Our study was carried out in a single Family Medicine Unit, which does not allow generalization of the results, however, it can be taken as an approach to carry out future studies with greater capacity for sample analysis.
ConclusionAt the time of diagnosis of arterial hypertension in the first level of care, more than half of the patients already had some stage of CKD, mainly stage 1 and 2, so it is necessary to implement strengthening actions in CKD screening. Patients with newly diagnosed hypertension remain longer in the initial stages of CKD, and then progress more quickly from the first stage change detected.
- •
Hypertension is one of the main causes of CKD.
- •
There is no certainty of the time it takes to develop CKD from the onset of hypertension.
- •
The prevalence and progression of CKD is greater in patients with a diagnosis of hypertension than in those who do not have it.
- •
In patients with newly diagnosed hypertension, CKD evolves slowly at first, to increase its progression after 7 years.
- •
The average annual decrease in eGFR was 5.8ml/min/year from the onset of hypertension and 6.8ml/min/year thereafter up to 10 years.
- •
A large percentage of patients with newly diagnosed hypertension already had some stage of CKD.
The present investigation has not received funding from public sector agencies, commercial sector or any other entity.
The manuscript has not been previously published or sent by any electronic or written means.
Conflict of interestsThe authors of this article have no conflict of interest.