To obtain a blood pressure reading is mandatory during either the general or specialized physical examination. This study describes factors associated with the accomplishment of blood pressure measurement in the first neurological consultation.
MethodsWe studied first ambulatory neurology consultations in a Mexican referral hospital. Demographic characteristics, diagnostic category of referral, final diagnosis and data on physical examination were collected to establish a logistic regression analysis in order to identify factors associated with the accomplishment of blood pressure measurement.
ResultsOver 8 months 778 outpatients were studied. The most frequent diagnoses for first consultation were headache (26%), epilepsy (14%) and stroke (13%). Only in 39% (n=301) of the outpatients blood pressure was registered, among them, 30% had normal blood pressure, 43% had 121–139/81–89mmHg, 20% had 140–159/90–99mmHg and 7% had ≥160/100mmHg. The independent factors that favored the practice of BP determination in multivariable analysis were >65 years of age (odds ratio: 2.26; 95% confidence interval: 1.52–3.36) and headache complaint (odds ratio: 1.81, 95% confidence interval: 1.30–2.53). Notably, only 43% of patients with stroke had blood pressure registration, even when these stroke patients had blood pressure readings, they had higher blood pressure than with other diagnoses (p<0.05).
ConclusionBlood pressure registration was frequently omitted from the first neurological consultation, particularly in outpatients who might need it the most.
La medición de la presión arterial es mandatoria durante el examen físico general o especializado. Este estudio describe factores asociados al cumplimiento de la medición de la presión arterial en la primera consulta neurológica.
MétodosRealizamos un estudio sobre consultas neurológicas ambulatorias en un hospital de referencia mexicano. Se recolectaron características demográficas, categoría diagnóstica de referencia, diagnóstico final y datos sobre el examen físico para construir un análisis de regresión logística con el objetivo de identificar factores asociados con el cumplimiento de la medición de la presión arterial.
ResultadosDurante 8 meses estudiamos a 778 pacientes. Los diagnósticos de envío más frecuentes fueron cefalea (26%), epilepsia (14%) y enfermedad cerebrovascular (13%). Solo en el 39% (n=301) de los pacientes se midió la presión arterial y, de entre ellos, el 30% presentaron presión arterial normal, el 43% 121-139/81-89mmHg, el 20% 140-159/90-99mmHg y el 7% ≥160/100mmHg. En un análisis multivariable, la edad >65 años (razón de momios: 2.26, intervalo de confianza del 95%: 1.52–3.36) y cefalea como motivo de consulta (razón de momios: 1.81, intervalo de confianza del 95%: 1.30–2.53) fueron los factores independientes asociados al registro de la presión arterial. De manera notable, solo al 43% de los pacientes con enfermedad cerebrovascular se les había registrado la presión sanguínea; estos pacientes la tenían más elevada que los pacientes con otros diagnósticos (p<0.05).
ConclusiónEn este estudio con frecuencia se omitió el registro de la presión arterial en la primera consulta neurológica, especialmente en pacientes que podrían necesitarlo más.
Blood pressure (BP) measurement is an essential part of the general physical examination, regardless of the level of training and specialization of the treating physician.1,2 Taking a routine BP reading is recommended for all patients having a first or consecutive ambulatory or in-hospital consultation, either in general or specialized medicine.1 However, in some clinical institutions this practice may not be followed as recommended. This topic has been poorly documented in scientific literature. In theory, the routine BP measurement is highly accomplished by cardiologists, internists, nephrologists, obstetricians and endocrinologists; but information on this issue is largely lacking in other areas, including neurology.
We performed a survey with the purpose to determine the frequency of BP measurement in a neurology outpatient facility, and to describe the factors associated with the carrying out of this recommendation.
MethodsWe performed a prospective survey on consecutive clinical records in the Neurology Department of the Hospital Civil de Guadalajara “Fray Antonio Alcalde”, Mexico, from January to August 2012. All clinical records of subjects who attended a first neurological consultation were systematically reviewed regardless of the history of hypertension. A standardized structured questionnaire was designed to capture demographic and clinical characteristics, as well as systolic (SBP) and diastolic blood pressure (DBP) readings from which mean arterial pressure (MAP) and pulse pressure (PP) were calculated. This survey was not anticipated by patients, medical assistants and treating physicians, and the BP readings were those they spontaneously decided to take and register. Usually, the medical assistants took a first BP measurement that could be corroborated in the neurology office by the treating physician “as necessary”. Therefore, when the patients’ clinical records did not have registered BP measurement, we reviewed the medical assistant's workbook in search for BP registries. For the purpose of the present study, we considered BP measurement “not performed” when any registry of BP associated with the first neurological consultation could not be found (either in clinical records or medical assistants’ workbook).
We used Pearson chi-square to assess proportions in nominal variables for univariate analyses. We used the Student t test in order to compare quantitative variables parametrically distributed between two groups. To find independent factors associated with BP measurement, multivariable analyses were constructed by forward stepwise logistic regression. Adjusted odds ratios with the respective 95% confidence intervals (CI) are given. The fitness of the models was evaluated by the Hosmer–Lemeshow goodness-of-fit test, which was considered as reliable if p>0.2. All calculations used two-sided p values and they were considered significant when p<0.05. SPSS v. 17.0 for windows was used in all calculations.
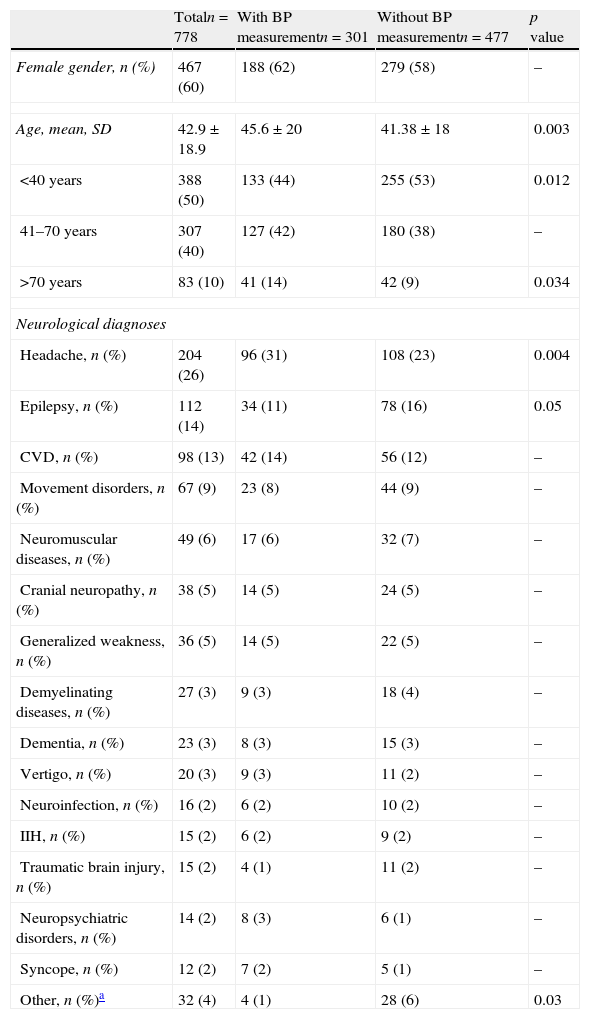
ResultsWe analyzed 778 outpatient medical records, 467 (60%) females and 311 (40%) males, with a mean age of 42.9 years (range 15–92 years). A total of 388 (50%) patients were<40 years old and 83 (11%) were >70 years old. The main neurological diagnoses were headache (26%), epilepsy (14%) and stroke (13%) (see Table 1).
Demographic characteristics and main diagnoses between groups.
| Totaln=778 | With BP measurementn=301 | Without BP measurementn=477 | p value | |
| Female gender, n (%) | 467 (60) | 188 (62) | 279 (58) | – |
| Age, mean, SD | 42.9±18.9 | 45.6±20 | 41.38±18 | 0.003 |
| <40 years | 388 (50) | 133 (44) | 255 (53) | 0.012 |
| 41–70 years | 307 (40) | 127 (42) | 180 (38) | – |
| >70 years | 83 (10) | 41 (14) | 42 (9) | 0.034 |
| Neurological diagnoses | ||||
| Headache, n (%) | 204 (26) | 96 (31) | 108 (23) | 0.004 |
| Epilepsy, n (%) | 112 (14) | 34 (11) | 78 (16) | 0.05 |
| CVD, n (%) | 98 (13) | 42 (14) | 56 (12) | – |
| Movement disorders, n (%) | 67 (9) | 23 (8) | 44 (9) | – |
| Neuromuscular diseases, n (%) | 49 (6) | 17 (6) | 32 (7) | – |
| Cranial neuropathy, n (%) | 38 (5) | 14 (5) | 24 (5) | – |
| Generalized weakness, n (%) | 36 (5) | 14 (5) | 22 (5) | – |
| Demyelinating diseases, n (%) | 27 (3) | 9 (3) | 18 (4) | – |
| Dementia, n (%) | 23 (3) | 8 (3) | 15 (3) | – |
| Vertigo, n (%) | 20 (3) | 9 (3) | 11 (2) | – |
| Neuroinfection, n (%) | 16 (2) | 6 (2) | 10 (2) | – |
| IIH, n (%) | 15 (2) | 6 (2) | 9 (2) | – |
| Traumatic brain injury, n (%) | 15 (2) | 4 (1) | 11 (2) | – |
| Neuropsychiatric disorders, n (%) | 14 (2) | 8 (3) | 6 (1) | – |
| Syncope, n (%) | 12 (2) | 7 (2) | 5 (1) | – |
| Other, n (%)a | 32 (4) | 4 (1) | 28 (6) | 0.03 |
The p value is annotated only for significant differences. BP: blood pressure; IIH: idiopathic intracranial hypertension; CVD: cerebrovascular disease (either ischemic or hemorrhagic); CNS: central nervous system.
Only 301 (39%) patients (188 women) received routine BP measurement, without significant differences according to gender. BP reading was more frequent in patients >70 years (p=0.034) and infrequent in those <40 years (p=0.012). Patients with headache complaint received more frequently a BP measurement (p=0.004). On the contrary, BP measurement was infrequent in patients with miscellaneous diagnoses such as myelopathy (p=0.042), epilepsy (p=0.05) and motor neuron disease (p=0.06) (see Table 1). The classification of a single BP reading was as follows: 89 (30%) patients had normal BP, 131 (43%) patients had SBP between 121 and 139 or DBP between 81 and 89mmHg; 59 (20%) patients had SBP between 140 and 159 or DBP between 90 and 99mmHg; and 22 (7%) patients had SBP >160 or DBP >100mmHg.
In multivariable adjusted analysis for several demographic and clinical factors, >65 years old (OR: 2.26, 95% CI: 1.52–3.36) and headache complaint (OR: 1.81, 95% CI: 1.30–2.53) were independent factors that favored BP measurement. Notably, only 43% of patients with stroke had measurements of BP, although these patients had higher SBP (137mmHg vs. 127mmHg, p=0.001), PP (77mmHg vs. 75mmHg, p=0.002) and MAP (101mmHg vs. 96mmHg, p=0.02), than their counterparts with other referral diagnoses.
DiscussionObtaining a routine BP reading in every patient receiving medical care was one of the first recommendations of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC), since 1977.2 However, in some specialized clinics this practice may not be followed as recommended, although it has improved over the past decades. The current evidence suggests that routine BP measurement remains suboptimal. The 1977 US National Ambulatory Medical Care Survey (NAMCS) reported routine BP measurement in 79% of outpatients with hypertension history and only 30% when this antecedent was absent,3 whereas the 2005 NAMCS reported a rise of 59.3%, from a total of 963.6 million medical consultations.4 In a 1977 epidemiological screening from United Kingdom BP reading was documented in 37.9% among 2760 ambulatory consultations.5
Blood pressure measurement in the neurological practice is important not only to identify subjects at vascular risk, but also to implement effective actions for primary or secondary prevention, for instance, in patients with cerebrovascular disease. Moreover, taking a BP reading is essential to define the best therapeutic approach in several neurological conditions. In 1977, an analysis of the NAMCS reported a frequency of 22.4% of BP measurement among neurologists.3 Notably, further information on this topic in the neurology practice is nonexistent.
Our results show that, at least in a referral institution in Mexico, less than half of outpatients attending a first neurological consultation received a routine BP measurement, and that advanced age and headache influenced the achievement of this recommendation. Of note, only 43% of outpatients with stroke had BP measurements, even when these patients usually have the highest BP readings, since this is the main risk factor influencing both recurrence and outcome.6–8 Our data are congruent with previous studies. Hypertension history, advanced age and headache diagnosis had been previously identified as determinants for BP measurement.3,4,8–10 This suggests that the initial complaint or diagnosis of referral drives the decision to perform an otherwise mandatory step of the medical examination.
ConclusionsThis study represents an invitation to reflection and to perform suitable actions to modify our regional practice in the immediate future, particularly in view of the recent results showing that 43.2% of the adult Mexican population has chronic arterial hypertension.11 More studies on this issue in different medical specialties are justified.
FundingThere was no funding for this study.
Conflict of interestsThe authors declare that there are no conflicts of interests.