Abstracts of the 2025 Annual Meeting of the ALEH
More infoPortal hypertension (PHT) is a major driver of complications and mortality in cirrhosis. Spleen stiffness measurement (SSM) via FibroScan® has emerged as a non-invasive marker of clinically significant PHT (CSPH) and esophageal varices (EV), yet evidence in Latin America is limited. This study aimed to correlate SSM with cirrhosis severity and markers of CSPH, compare its values with those of healthy controls, and determine an optimal cutoff for EV detection.
Materials and MethodsCross-sectional study including 40 cirrhotic patients (β-blocker naïve) and 10 healthy controls. SSM (kPa) was measured with FibroScan® Expert 630. Variables included Child–Pugh class, MELD-Na, D’Amico stage (≥4 = decompensation), platelet count, Doppler ultrasound, and endoscopic confirmation of EV. Statistical analysis included non-parametric tests, ROC curves, Youden’s index, and multivariable logistic regression (SSM, platelets, portal vein diameter, Child–Pugh).
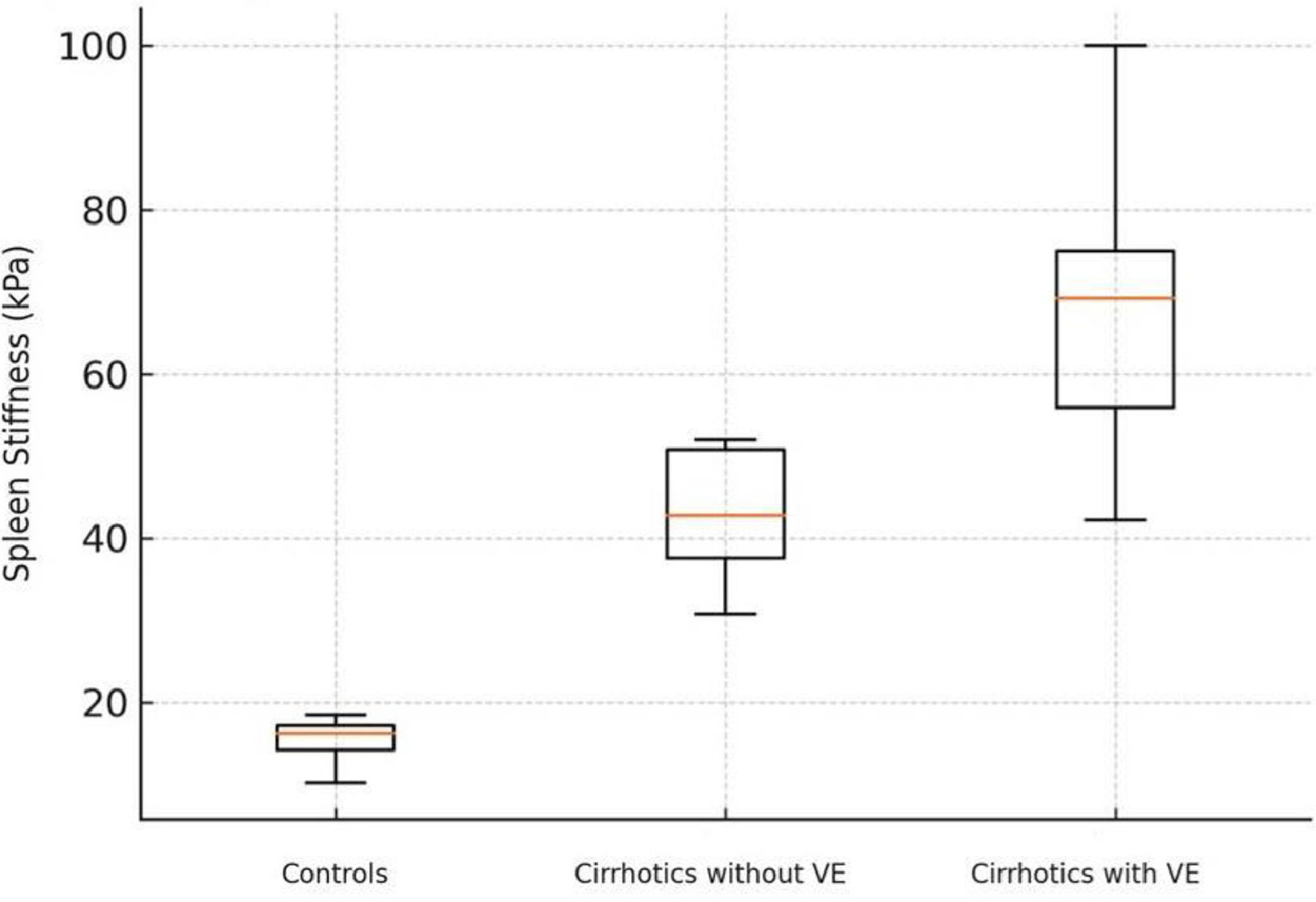
ResultsMean age was 56.8 years; 60% male; BMI 28.8 kg/m2; 40% obese. Median SSM was higher in cirrhotics (64.5 kPa) than in controls (16.0 kPa; p < 0.001). Among cirrhotics, higher SSM correlated with Child–Pugh C (p = 0.004), MELD-Na ≥ 22 (p = 0.018), decompensation (p = 0.030), and thrombocytopenia (p = 0.021). EV were present in 22 patients (55%), with SSM 67.3 vs 46.0 kPa (p = 0.004). AUC was 0.81; optimal cutoff 55 kPa. Only SSM remained independently associated with EV (OR 1.14 per kPa; AUC 0.91).
ConclusionsIn this Latin American cohort, SSM ≥ 55 kPa was the most accurate non-invasive predictor of EV and may guide endoscopic screening in clinical practice.