Abstracts Asociación Mexicana de Hepatología (AMH) 2024
More infoHepatic hemangioma, the most common benign tumor of the liver. Large ones may develop Kasabach Merrit syndrome (KM) if associated with coagulopathy.
Objectiveto describe diagnostic approach and treatment of hemangioma with KM syndrome in an adult with complications during pregnancy, treated with embolization and liver transplantation, review of the literature.
Materials and PatientsA 35-year-old woman referred from Durango by angiology to the hepatology department for a failed laparoscopic biopsy attempt due to the presence of unspecified vascular lesions which presented bleeding due to severe coagulation disorders, controlled in her hospital of origin. During the consultation, imaging and biochemical characteristics of thrombocytopenia and anemia were evaluated and KM syndrome was considered, complementing the diagnosis with Leukocytes 5.3 × 103/uL, HB 10.3 g/dL, Hto 29.8%, VCM 99.2 fL, HCM 34.3 pg platelets 111 × 103/uL, Cr 0.61mg/dL, BT 1. 05mg/dl, FA 64 U/L, GGT 55 U/L AST 15 U/L, ALT 20 U/L, albumin 4.82g/dL, fibrinogen 52, dimer D 49.46 ug/dl, AFP 1.21 ng/ml, carcinoembryonic 0.94 ng/ml, Ca 19-9 2. 0 U/ml TP 14.6 INR 1.0, it was decided to perform a biopsy to rule out hemangioepithelioma, presenting severe hemorrhage requiring transarterial embolization on two occasions. Subsequently, she returned to the clinic with a normoevolutive pregnancy and a considerable increase in the size of the lesions, requiring cesarean section due to placenta accrete, again generating hemorrhage and development of ascites. Due to the hepatic deterioration, a protocol for transplantation was established and successfully performed in March 2024, with a total reversal of the coagulation disorders after the procedure and currently with no alterations.
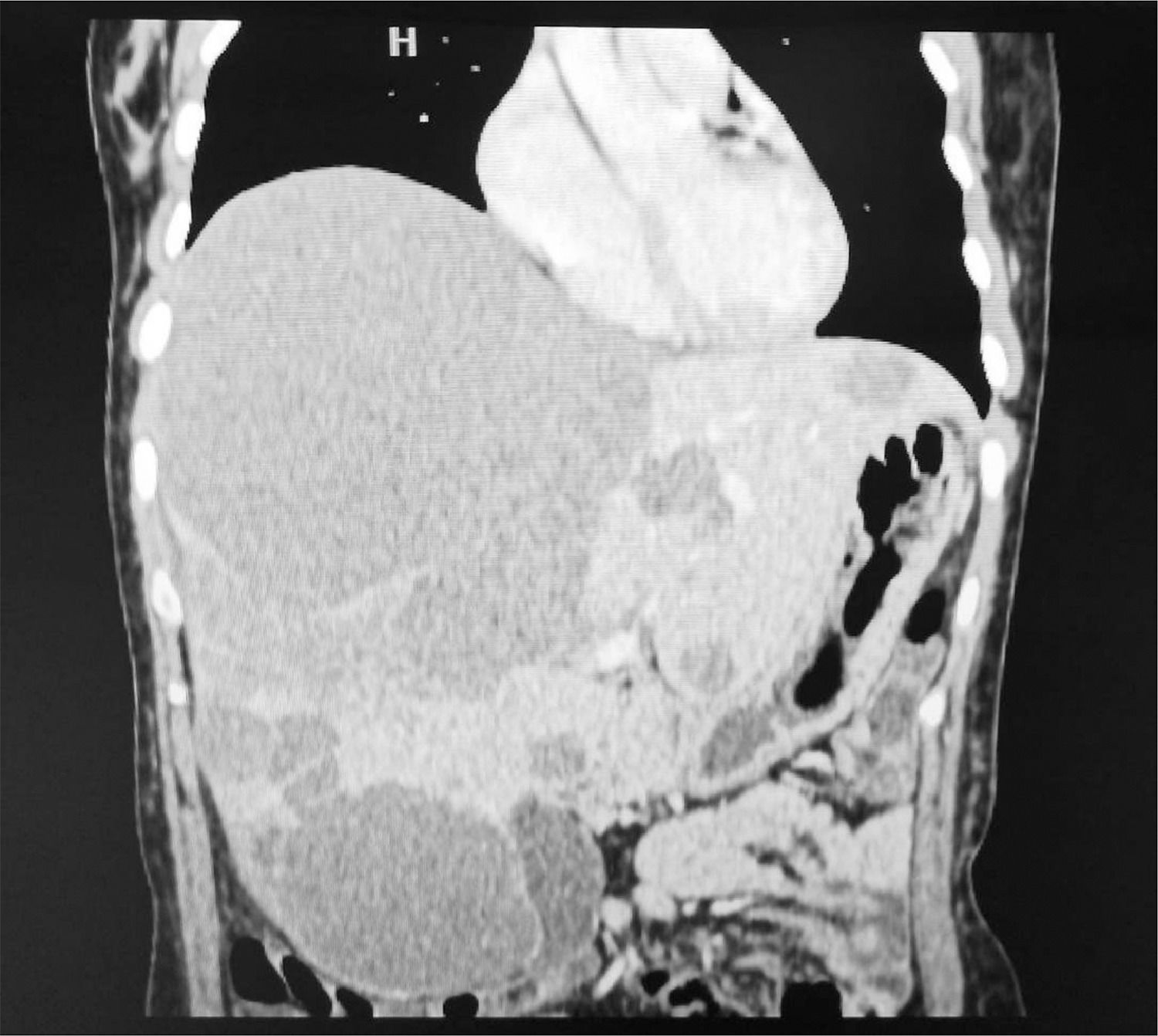
ResultsHepatic hemangiomas are mostly asymptomatic and small; those larger than 10 cm are considered giants and present with non-specific symptoms such as abdominal pain, fatigue, etc. They are diagnosed by tomography (CT) or magnetic resonance imaging (MRI); in CT they are observed as relatively well-defined hypodense nodules, hypoattenuated in relation to parenchyma and centripetal peripheral enhancement with contrast medium, with complete and persistent opacification in late sections. It presents complications such as intralesional hemorrhage, mass effect in adjacent structures, and rupture with intraperitoneal hemorrhage. Some lesions may develop KM syndrome, a vascular disease characterized by thrombocytopenia, microangiopathic hemolytic anemia, coagulopathy and hepatic vascular lesions. The pathogenesis is due to the sequestration of platelets and coagulation factors in the abnormal endothelium of the vascular lesion. It requires biopsy to rule out malignant neoplasms (hemangioepithelioma). Occurs in neonates, rarely in adults. Transarterial embolization and chemoembolization can be used as a treatment for bleeding. Surgical resection is not recommended because of technical difficulty and risk of intraoperative bleeding. When there is severe liver dysfunction or recurrent bleeding, liver transplantation should be considered.
ConclusionsKM syndrome should be suspected in large vascular lesions accompanied by anemia, thrombocytopenia and coagulopathy; it is an uncommon complication that can generate hemorrhage and require management with interventional radiology or liver transplantation as in the case presented. Management should be multidisciplinary.