Up to 15% of muscle-invasive bladder cancers (MIBC) arise from the progression of a non-muscle-invasive neoplasm. Despite sharing similar treatment strategies, the literature reports differences in survival rates between these two groups. This study aims to identify differences in recurrence and survival that may influence individualized treatment approaches.
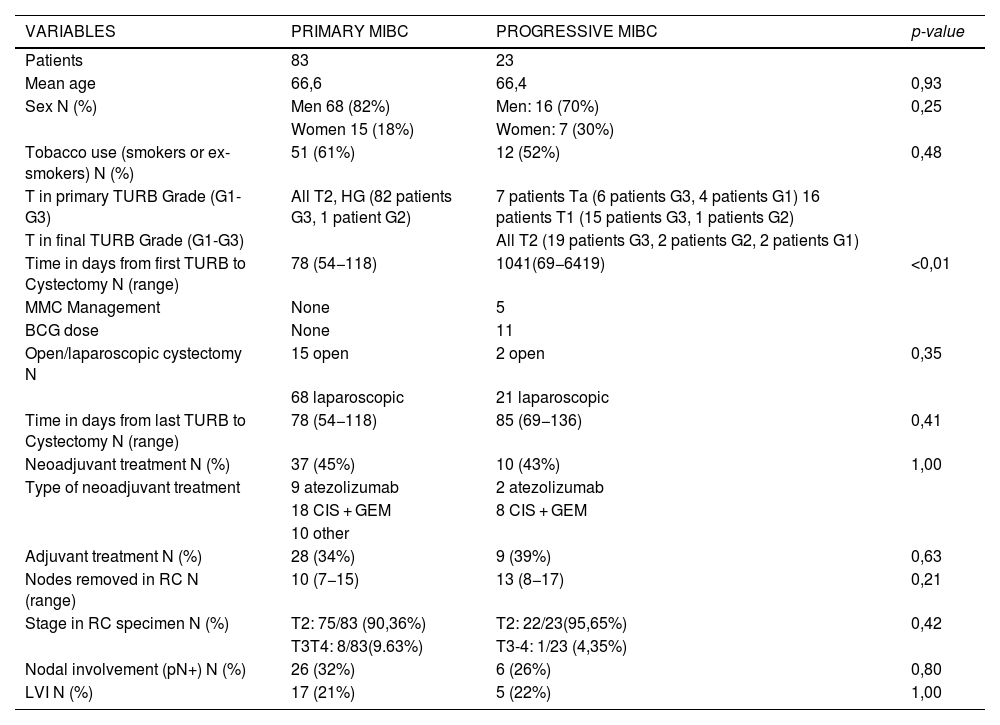
Material and methodsProspective study of cystectomies performed for MIBC between 2011 and 2023, collecting demographic, diagnostic, treatment, and recurrence data (local, urothelial, or distant). A comparative and multivariate analysis was conducted.
ResultsWe did not observe significant differences in recurrence rates between primary and progressive MIBC. However, the group with progression showed better overall survival (OS) rates at 2, 5 and 10 years (100%, 90%, 55%) compared to the primary (80%, 55%, 35%; p = 0.012), as well as better cancer-specific survival (CSS) (100%, 100%, 95% vs. 85%, 77%, 65%; p = 0.033). Independent risk factors for recurrence include pN+ (OR: 3.72) and lymphovascular invasion (LVI) (OR: 5.53). Predictors of lower OS include age, nodal involvement, LVI and relapse at any level. For CSS, predictors include nodal involvement, LVI and relapse at any level.
ConclusionsIn our series, patients with progressive MIBC have better OS and CSS. For both groups, pN + and LVI are independent risk factors for recurrence. Nodal involvement, LVI and relapse at any level are predictors of poorer OS and CSS.
Hasta el 15% del cáncer de vejiga músculo invasivo (CVMI) surge como progresión de una neoplasia no músculo invasiva. A pesar de que las estrategias de tratamiento son similares, en la literatura se muestran diferencias en la supervivencia entre ambos grupos. Este estudio busca identificar diferencias en cuanto a recidiva y supervivencia que puedan influir en el tratamiento individualizado.
Material y métodosEstudio prospectivo de cistectomías por CVMI desde 2011–2023 recogiendo datos demográficos, diagnósticos, de tratamiento y recidivas (local, urotelial o a distancia).Se realiza un análisis comparativo y multivariante
ResultadosNo observamos diferencias significativas en las tasas de recidiva entre CVMI primarios y progresivos. Sin embargo, el grupo progresivo mostró mejor supervivencia global (SG) a 2, 5 y 10 años (100%, 90%, 55%) en comparación con el primario (80%, 55%, 35%; p = 0,012), así como mejor supervivencia cáncer específica (SCE) (100%, 100%, 95% frente a 85%, 77%, 65%; p = 0,033). Los factores de riesgo independientes para la recidiva incluyen pN+ (OR: 3,72) e ILV (OR: 5,53). Los predictores de menor SG incluyen edad, afectación ganglionar, ILV y recaída a cualquier nivel. Para la SCE, los predictores son la afectación ganglionar, ILV y recidiva a cualquier nivel.
ConclusionesEn nuestra serie, los pacientes con CVMI progresivos presentan mejor SG y SCE. Para ambos grupos, pN + y ILV son factores de riesgo independientes para la recidiva. Son factores predictores de menor SG y SCE la afectación ganglionar, la ILV y la recaída a cualquier nivel.