Tuberculosis is one of the infectious diseases with the highest mortality worldwide, and also results in high costs and periods of disability. Thus, it is a priority to make timely diagnoses at the Primary Care level, with the aim of initiating early treatments and reducing transmission.
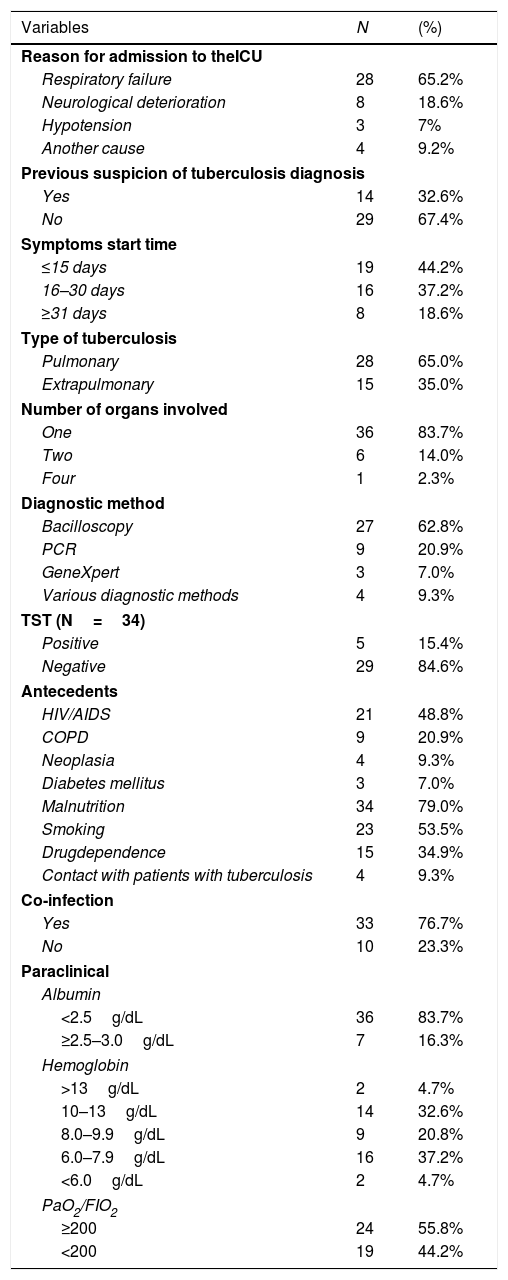
MethodThis descriptive observational study included a series of cases of 43 patients with a confirmed diagnosis of tuberculosis after admission to intensive care unit (ICU) between 2012 and 2016. The objective of this study was to describe the sociodemographic, epidemiological, and clinical characteristics of this group of patients.
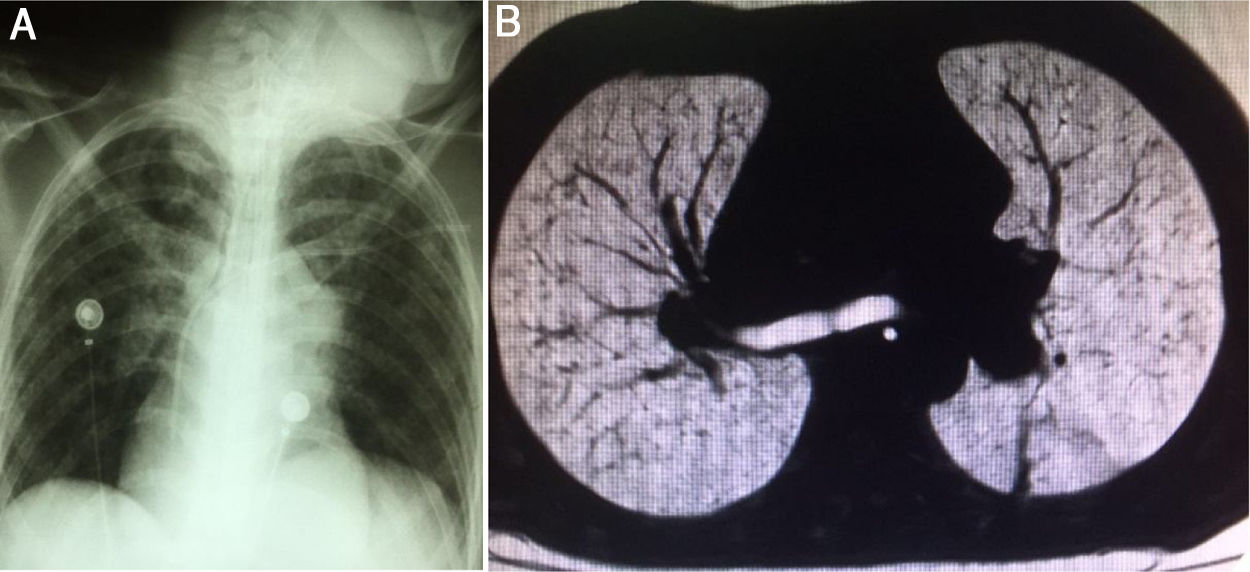
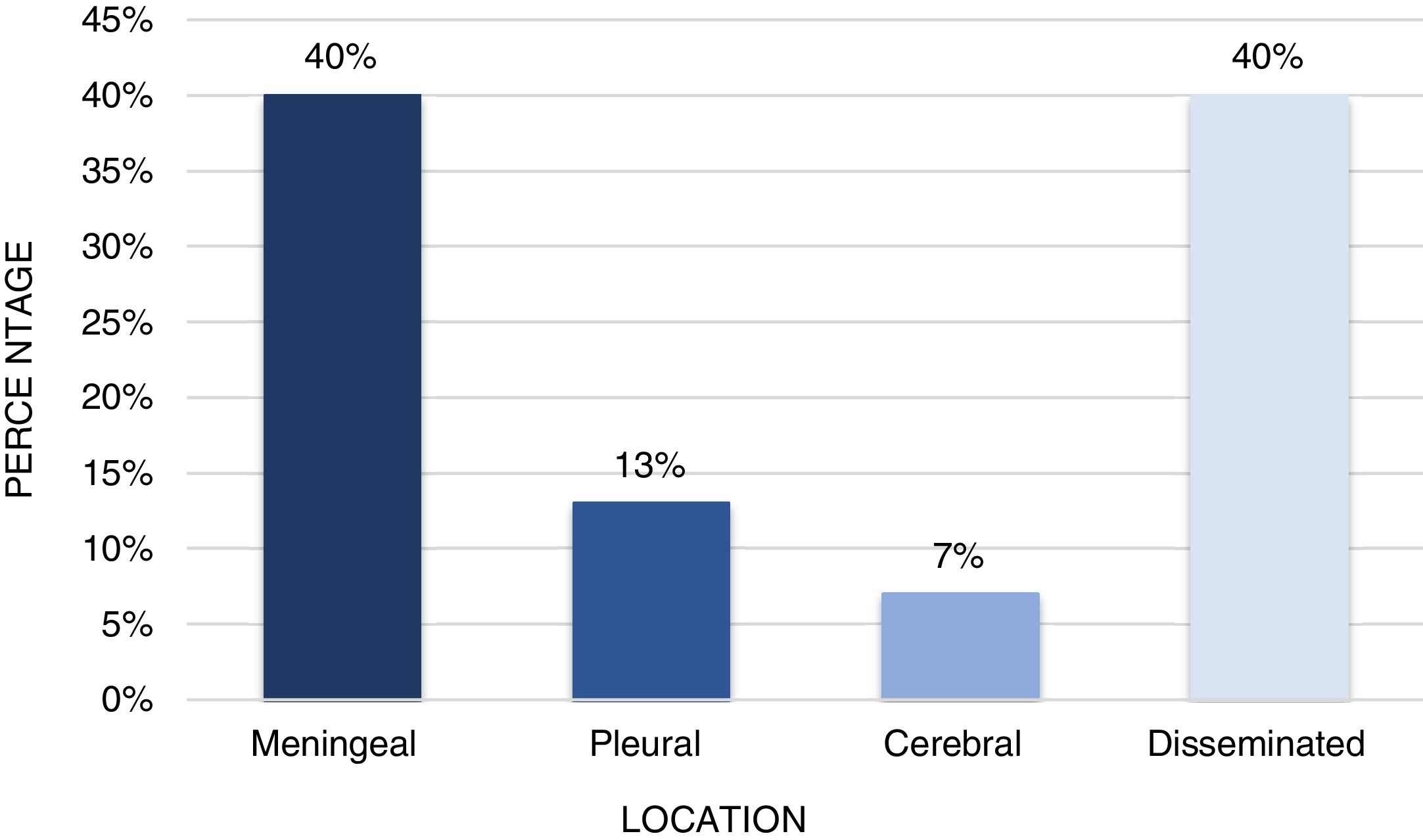
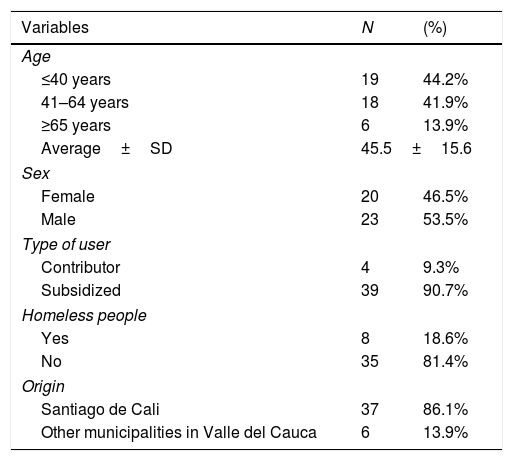
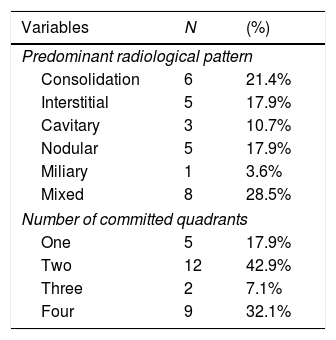
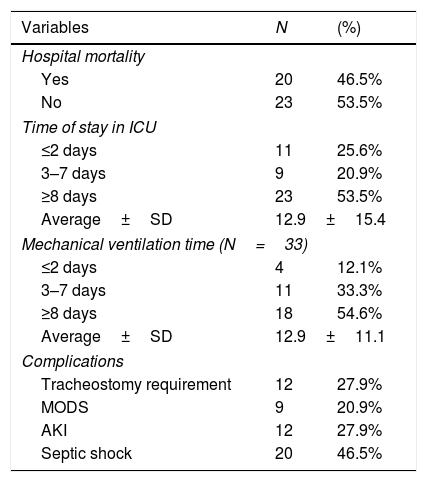
ResultsThe age range was between 21 and 80 years; there was a predominance of male gender (53.5%), those affiliated to the subsidised health regime (90.7%), homeless people (18.6%), and those with drug dependence (35%). The main cause of admission was respiratory failure (65.2%), followed by neurological deterioration (18.6%). Almost two-thirds (65%) of the cases had pulmonary tuberculosis exclusively, and 35% had extrapulmonary tuberculosis. Furthermore, 76.7% of patients had co-infection, with human immunodeficiency virus (HIV) being the most frequent (48.8%), followed by pneumonia (34.9%). Moderate to severe malnutrition was documented in 79% of cases, and anemia was found in 95.3%. The mortality rate during the stay in ICU was 46.5%, with prevalence of male gender and prolonged stay (an average of 19 days).
ConclusionsIn this case series, there was a predominance of the active working population, those with drug dependence, homeless people, those who were co-infected with HIV, and those with hypoalbuminaemia, anemia, and malnutrition. In addition, around half of the patients died during hospital admission. They had septic shock, an ICU stay and ventilatory support greater than or equal to 8 days. This reflects the need to carry out studies evaluating public health strategies for the early detection of cases in groups of patients with the described characteristics, as well as the importance of always considering tuberculosis as a diagnostic possibility in the ICU.
A nivel mundial la tuberculosis es una de las enfermedades infecciosas que genera la mayor mortalidad, lo que causa altos costos y períodos de discapacidad. Por esta razón, es una prioridad realizar diagnósticos oportunos en el nivel de atención primaria, con el objetivo de iniciar tratamientos tempranos y reducir la transmisión.
MétodoEstudio observacional descriptivo de una serie de casos con 43 pacientes. Se incluyeron pacientes con diagnóstico de tuberculosis confirmado después del ingreso en la unidad de cuidados intensivos (UCI) entre 2012 y 2016. El objetivo de este estudio fue describir las características sociodemográficas, epidemiológicas y clínicas de este grupo de pacientes.
ResultadosEl rango de edad fue entre 21 y 80 años, con predominio del género masculino (53,5%), afiliación al régimen de salud subsidiado (90,7%), habitantes de la calle (18,6%) y farmacodependencia (35%). La principal causa del ingreso fue la insuficiencia respiratoria (65,2%) seguida del deterioro neurológico (18,6%). El 65% correspondió a pacientes con tuberculosis exclusivamente pulmonar, y el 35% a tuberculosis extrapulmonar. El 76,7% tuvo coinfección, de los cuales el VIH fue la más frecuente (48,8%), seguido por neumonía (34,9%). La desnutrición moderada a severa se documentó en el 79%, y se encontró anemia en el 95,3% de los sujetos. La mortalidad durante la estancia en la UCI fue del 46,5%, en quienes predominó el género masculino y la estancia prolongada (promedio de 19 días).
ConclusionesEn nuestra serie de casos se evidenció un predominio de la población laboralmente activa, farmacodependencia, habitantes de la calle, coinfección con VIH, hipoalbuminemia, anemia y malnutrición. Además, alrededor de la mitad de los pacientes fallecieron durante la hospitalización, presentaron shock séptico, estancia en la UCI y soporte ventilatorio mayor o igual a 8 días. Esto refleja la necesidad de realizar estudios que evalúen estrategias de salud pública para la detección temprana de casos en grupos de pacientes con las características descritas, así como la importancia de considerar la tuberculosis en la UCI siempre como una posibilidad diagnóstica.
Artículo
Socios de la Asociación de Medicina Crítica y Cuidado Intensivo
Para acceder a la revista
Es necesario que lo haga desde la zona privada de la web de la AMCI, clique aquí