The aim of this paper is to analyse the characteristics of the victims and the circumstances of sexual violence related with the risk of physical lesions, as well as to determine the frequency and severity of the injuries.
Material and methodsDescriptive study of 702 cases of sexual assault attended at the Institute of Legal Medicine and Forensic Sciences of Alicante between the years 2016 and 2020. A comparative study was carried out between victims with and without injuries, to identify the variables associated to their presentation.
Results314 victims attended showed physical injuries (44.8%). Profile of the victims with injuries were women (95.5%), aged 18–27 years (31.3%), and previous alcohol consumption (50%). Injuries physical were mainly extragenital (38.6%), anogenital (15%), or both, and most cases were mild in severity (97.5%). Recovery was less to 1 week (83.4%) and without aftermath (97.1%). When the victim showed aftermath (9 cases), the most frequent were psychological type (1.6%).
ConclusionsPhysical injuries in sexual violence is related with circumstances of victim vulnerability: women, age between 18 and 27 years, and previous alcohol consumption.
Our study shows that anogenital lesions are absent in a significative number of victims of sexual assault, so this absence cannot exclude sexual violence. The lesions found are mild in severity, and the absence of physical aftermath in most of the victims may be conditioned by the scarce follow-up of them.
El objetivo principal de este trabajo es analizar las características de las víctimas y circunstancias de la violencia sexual asociadas con un mayor riesgo de presentar lesiones físicas, así como determinar la frecuencia y severidad de las mismas.
Material y MétodosEstudio descriptivo retrospectivo de 702 casos de violencia sexual atendidos en el Instituto de Medicina Legal y Ciencias Forenses de Alicante entre los años 2016–2020. Se ha realizado un estudio comparativo entre las víctimas de violencia sexual con lesiones físicas y sin lesiones, para analizar las variables asociadas que pueden influir en su presentación.
ResultadosDel total de 702 víctimas de violencia sexual, 314 casos (44,8%) presentaban lesiones físicas. Las víctimas con lesiones físicas la mayoría eran mujeres (95,5%), entre 18 y 27 años (31,3%), que referían un consumo voluntario previo de sustancias, fundamentalmente de alcohol (50%). Las lesiones físicas más frecuentes fueron a nivel extragenital (38,6%) seguidas de lesiones a nivel anogenital (15%), de carácter leve en la mayoría de los casos (97,5%). Los días totales de curación fueron menores o iguales a una semana (83,4%). La mayoría curó sin secuelas (97.1%). Las víctimas que presentaron secuelas (9 casos), las más frecuentes fueron de carácter psíquico (1.6%).
ConclusionesLa violencia sexual en el grupo de víctimas con lesiones físicas, se asocia a factores de vulnerabilidad para la víctima: sexo femenino, edad entre 18 y 27 años, y consumo previo de alcohol.
Nuestro estudio confirma que las lesiones anogenitales son poco frecuentes en la mayoría de las víctimas de violencia sexual, por lo que su ausencia no puede descartar el haber sufrido violencia sexual. Las lesiones físicas encontradas fueron de carácter leve en la mayoría de los casos. La ausencia de secuelas psíquicas en muchas de las víctimas, puede estar condicionado por el escaso seguimiento de las mismas.
The presence of physical injuries in the victims of sexual violence (SV) tends to be associated with high levels of expectations that they will be found, above all in the form of anogenital injuries.1,2 In spite of this, anogenital injuries are not found in the majority of the victims of SV, so that their absence does not signify that no sexual contact has occurred.2–4 Similarly, anogenital injuries may arise in consensual sexual relationships,1,4,5 so that we should be cautious when interpreting them.1
The presence of extragenital injuries is a sign of the use of physical force by an attacker.6 The most common locations of some of these injuries, even those which are apparently trivial, are especially significant and are important aids in confirming or rejecting the victim's account.1,4
The core aim of this study is to analyse the characteristics of the victims and circumstances of sexual violence, those which are associated with a higher risk of (extragenital and anogenital) physical injuries, as well as to determine their frequency and severity, their evolution, and the presence of sequelae, psychological ones above all, which are the most likely to remain over time.
Material and methodsA descriptive retrospective study was undertaken of 702 victims of suspected SV. They were treated within the catchment area of the Alicante Institute of Legal Medicine and Forensic Sciences (IMLCFA) from 1 January 2016 to 31 December 2020, both inclusive.
Information was obtained from the documentation contained in the victims' clinical histories, based on the standard formula for data gathering included in the medical-forensic action protocol for cases of crimes against sexual freedom,7,8 according to the new protocol of the Consejo Médico Forense9 and the preliminary forensic report by the shift in question (n = 314).
Likewise, the following documents were taken into account in the cases with a medical report: the medical report for the hearing (n=24), or, if applicable, the medical report based on a new examination of the victim (n=40), as sent to the judicial authority and the Attorney General's Office. In the cases without a medical report, the average time taken to cure the physical injuries was taken into account (as calculated by 2 experienced researchers and based on the data contained in the clinical history) (n=250).
In the examination of the victims, anogenital injuries were detected by direct observation (as no mention is made of the use of visual aids in the cases studied: colposcopy, toluidine blue, anoscope). The location, extent, and type of injuries were taken into account, using the standards commonly accepted for this according to the English acronym TEARS, corresponding to: tear, ecchymosis, abrasion, reddening, and swelling.5
The following variables were analysed as well as the demographic characteristics of the victims: a history of mental illness and/or drug addiction, previous voluntary consumption of alcohol, drugs of abuse and/or medication. The time which had elapsed between the crime and the examination was also recorded, together with the time it occurred, the number of attackers and their relationship with the victim, type of sexual contact, the place where sexual violence occurred, the presence or absence of physical injuries, their location, extent, and type.
The resulting information was analysed using v. 15.0 of the SPSS programme for Windows. A descriptive analysis of all of the variables was performed.
ResultsThe study included a total of 702 victims of sexual violence, with an average age of 24.6 years. The majority were women (92.9%). The voluntary consumption of substances moments prior to the crime was an appreciable factor in increasing vulnerability, fundamentally alcohol in 307 cases (46.9%).10
Factors increasing the vulnerability of the victims with physical injuriesThe victims of sexual violence had (extragenital and anogenital) physical injuries in 314 cases (44.8%). During the time period studied, 15 victims suffered 2 or more episodes of SV, and these too were included. The cases which resulted in death were not included. Four victims who solely recorded psychological injuries (anxiety, depression, anxiety-depressive disorders, and acute post-traumatic stress disorder) were excluded.
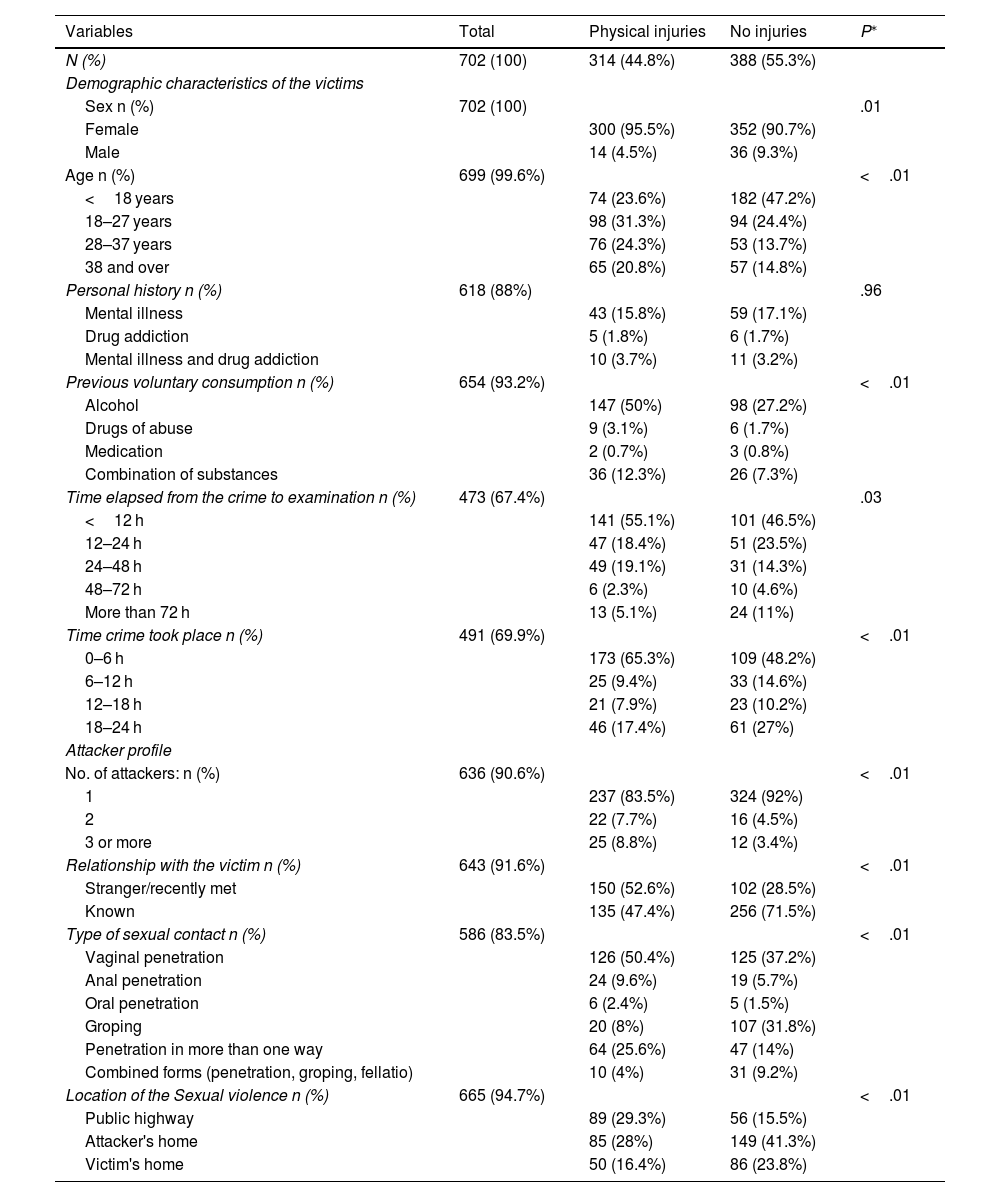
A comparative study was made between the victims of SV with physical injuries and those without injuries, to analyse the associated variables that may influence this (Table 1).
Demographic characteristics of the victims and circumstances of the sexual violence, according to the presence or absence of physical injuries.
| Variables | Total | Physical injuries | No injuries | P⁎ |
|---|---|---|---|---|
| N (%) | 702 (100) | 314 (44.8%) | 388 (55.3%) | |
| Demographic characteristics of the victims | ||||
| Sex n (%) | 702 (100) | .01 | ||
| Female | 300 (95.5%) | 352 (90.7%) | ||
| Male | 14 (4.5%) | 36 (9.3%) | ||
| Age n (%) | 699 (99.6%) | <.01 | ||
| <18 years | 74 (23.6%) | 182 (47.2%) | ||
| 18–27 years | 98 (31.3%) | 94 (24.4%) | ||
| 28–37 years | 76 (24.3%) | 53 (13.7%) | ||
| 38 and over | 65 (20.8%) | 57 (14.8%) | ||
| Personal history n (%) | 618 (88%) | .96 | ||
| Mental illness | 43 (15.8%) | 59 (17.1%) | ||
| Drug addiction | 5 (1.8%) | 6 (1.7%) | ||
| Mental illness and drug addiction | 10 (3.7%) | 11 (3.2%) | ||
| Previous voluntary consumption n (%) | 654 (93.2%) | <.01 | ||
| Alcohol | 147 (50%) | 98 (27.2%) | ||
| Drugs of abuse | 9 (3.1%) | 6 (1.7%) | ||
| Medication | 2 (0.7%) | 3 (0.8%) | ||
| Combination of substances | 36 (12.3%) | 26 (7.3%) | ||
| Time elapsed from the crime to examination n (%) | 473 (67.4%) | .03 | ||
| <12 h | 141 (55.1%) | 101 (46.5%) | ||
| 12–24 h | 47 (18.4%) | 51 (23.5%) | ||
| 24–48 h | 49 (19.1%) | 31 (14.3%) | ||
| 48–72 h | 6 (2.3%) | 10 (4.6%) | ||
| More than 72 h | 13 (5.1%) | 24 (11%) | ||
| Time crime took place n (%) | 491 (69.9%) | <.01 | ||
| 0–6 h | 173 (65.3%) | 109 (48.2%) | ||
| 6–12 h | 25 (9.4%) | 33 (14.6%) | ||
| 12–18 h | 21 (7.9%) | 23 (10.2%) | ||
| 18–24 h | 46 (17.4%) | 61 (27%) | ||
| Attacker profile | ||||
| No. of attackers: n (%) | 636 (90.6%) | <.01 | ||
| 1 | 237 (83.5%) | 324 (92%) | ||
| 2 | 22 (7.7%) | 16 (4.5%) | ||
| 3 or more | 25 (8.8%) | 12 (3.4%) | ||
| Relationship with the victim n (%) | 643 (91.6%) | <.01 | ||
| Stranger/recently met | 150 (52.6%) | 102 (28.5%) | ||
| Known | 135 (47.4%) | 256 (71.5%) | ||
| Type of sexual contact n (%) | 586 (83.5%) | <.01 | ||
| Vaginal penetration | 126 (50.4%) | 125 (37.2%) | ||
| Anal penetration | 24 (9.6%) | 19 (5.7%) | ||
| Oral penetration | 6 (2.4%) | 5 (1.5%) | ||
| Groping | 20 (8%) | 107 (31.8%) | ||
| Penetration in more than one way | 64 (25.6%) | 47 (14%) | ||
| Combined forms (penetration, groping, fellatio) | 10 (4%) | 31 (9.2%) | ||
| Location of the Sexual violence n (%) | 665 (94.7%) | <.01 | ||
| Public highway | 89 (29.3%) | 56 (15.5%) | ||
| Attacker's home | 85 (28%) | 149 (41.3%) | ||
| Victim's home | 50 (16.4%) | 86 (23.8%) |
In our study, the majority of the victims with physical injuries were women (95.5%). The average age was 27.6 years, (range from 2 to 67 years, SD±12.499). Injuries were present more often in the group aged from 18 to 27 years (98 cases; 31.3%), while more of the victims <18 had no injuries (182 cases; 47.2%). Both results are statistically significant (P < .001).
Although a history of mental illness and/or drug addiction was less frequent in the group of victims with injuries (58 cases; 21.3%), this was not statistically significant (P = .965).
Many of the victims with injuries mentioned previously having consuming alcohol voluntarily, either alone (147 cases; 50%) or in combination with drugs of abuse and medication (36 cases; 12.3%). These results are statistically significant (P<.001).
The majority of the victims sought medical assistance in the first 11 h (141 cases; 55.1% of the group of victims with physical injuries), although these results were not found to be statistically significant (P=.032).
In both groups, the most frequent time was during the early hours of the morning (from 0 to 6 h). This tendency was the highest in the group with physical injuries (173 cases; 65.3%), and these results were found to be statistically significant (P=.002).
In the majority of cases, there was only 1 attacker. In the group of victims with physical injuries, victims were proportionally more likely to have physical injuries as the number of attackers increased (more than 1 attacker in 47 cases; 16.5%), and these results are statistically significant (P = .003).
The relationship between the attacker and victim was analysed. In the group of victims with physical injuries, in more than half of the cases, the attacker was either a stranger or had recently met the victim: this was so in 150 (52.6%) cases, and this result is statistically significant (P<.001).
The most frequent type of SV in the group of victims with physical injuries was vaginal penetration (50.4%), followed by penetration in more than one way (25.6%) and anal penetration (9.6%), while in the group of victims without physical injuries, vaginal penetration occurred in 37.2% of cases, followed by groping (31.8%). These results are statistically significant (P<.001).
There were 4 cases of penetration with an object, and no anogenital injuries were recorded in any of these cases. Likewise, penetration with the fingers occurred more often in the victims without injuries (87 cases; 28.6%) than it did in the victims with physical injuries, with 34 cases (15%). These results are statistically significant (P<.01).
In the group of victims with physical injuries, the most frequent location of the attack was in the public highway (89 cases; 29.3%), followed by the attacker's home (85 cases; 28%). These results are statistically significant (P<.01).
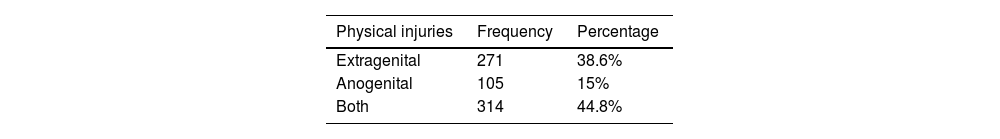
Type and location of physical injuriesIn the group of victims with physical injuries (314 cases; 44.8%), extragenital injuries were the most frequent, with 271 cases (38.6%), followed by anogenital injuries with 105 cases (15%) (Table 2).
The most frequent locations of anogenital injuries were at genital level (73 cases; 23.2%), followed by anal injuries (19 cases; 6.1%), and both locations (13 cases; 4.1%).
No significant results were obtained in connection with the number of attackers and the presence of anogenital injuries (2 attackers, 6 cases; 6.3%; 3 or more attackers, 6 cases; 6.3%) (P=.972).
The majority of the victims in the 119 cases of suspected chemical submission (SCS) had no anogenital injuries (98 cases; 82.4%). This result was not found to be statistically significant (P=.367).
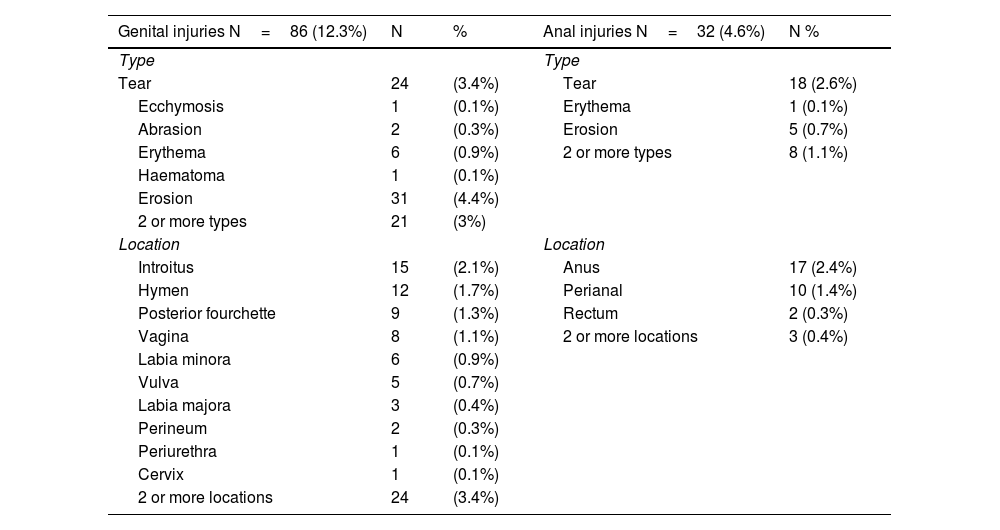
The types of physical injury to the genitals found the most often were: erosion (31 cases; 4.4%), followed by tearing (24 cases; 3.4%). 21 victims (3%) had more than one type of injury. The most frequent location was the introitus (15 cases; 2.1%), followed by the hymen (12 cases; 1.7%). Injuries in 2 or more locations were recorded in 24 cases (3.4%). The most frequent time band in which genital injuries occurred was from 6 to 9 h (16 cases) (Table 3).
Frequencies of the type and location of physical, genital, and anal injuries in sexual violence victims.
| Genital injuries N=86 (12.3%) | N | % | Anal injuries N=32 (4.6%) | N % |
|---|---|---|---|---|
| Type | Type | |||
| Tear | 24 | (3.4%) | Tear | 18 (2.6%) |
| Ecchymosis | 1 | (0.1%) | Erythema | 1 (0.1%) |
| Abrasion | 2 | (0.3%) | Erosion | 5 (0.7%) |
| Erythema | 6 | (0.9%) | 2 or more types | 8 (1.1%) |
| Haematoma | 1 | (0.1%) | ||
| Erosion | 31 | (4.4%) | ||
| 2 or more types | 21 | (3%) | ||
| Location | Location | |||
| Introitus | 15 | (2.1%) | Anus | 17 (2.4%) |
| Hymen | 12 | (1.7%) | Perianal | 10 (1.4%) |
| Posterior fourchette | 9 | (1.3%) | Rectum | 2 (0.3%) |
| Vagina | 8 | (1.1%) | 2 or more locations | 3 (0.4%) |
| Labia minora | 6 | (0.9%) | ||
| Vulva | 5 | (0.7%) | ||
| Labia majora | 3 | (0.4%) | ||
| Perineum | 2 | (0.3%) | ||
| Periurethra | 1 | (0.1%) | ||
| Cervix | 1 | (0.1%) | ||
| 2 or more locations | 24 | (3.4%) |
Tearing was the type of physical injury in the anal and perianal region found the most often (18 cases; 2.6%). 8 victims (1.1%) had more than one type of injury. The most common location was the anus (17 cases; 2.4%), followed by the perianal region (10 cases; 1.4%). Injuries were found in 2 or more locations in 3 cases (0.4%). The most frequent timing corresponding to anal and perianal injuries was from 6 to 9 h (14 cases) (Table 3).
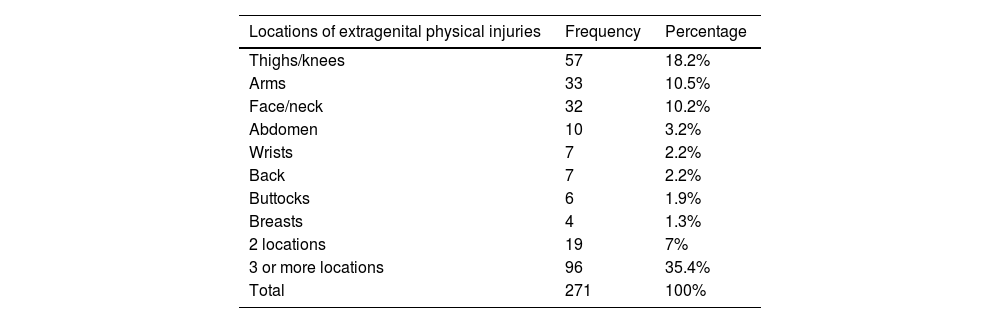
Extragenital physical injuriesIn the group of victims with extragenital physical injuries, the majority occurred in women (263 cases; 97%). These results are statistically significant (P=.001). The victims mentioned previous voluntary alcohol consumption more often (164 cases; 64.6%) than did the victims without extragenital injuries (143 cases; 35.8%). These results are statistically significant (P<.001).
When the locations of the extragenital injuries in the corresponding victims are grouped, the most frequent were those on the lower limbs (57 cases; 21%), followed by the upper limbs (40 cases; 14.8%), the head, face, and neck (32 cases; 11.8%) and the trunk (27 cases; 10%). Injuries in 3 or more locations were recorded in 96 cases (35.4%). Table 4 shows the injuries according to their location in especially significant regions.
Frequency and percentages of locations and extent of extragenital physical injuries in sexual violence victims.
| Locations of extragenital physical injuries | Frequency | Percentage |
|---|---|---|
| Thighs/knees | 57 | 18.2% |
| Arms | 33 | 10.5% |
| Face/neck | 32 | 10.2% |
| Abdomen | 10 | 3.2% |
| Wrists | 7 | 2.2% |
| Back | 7 | 2.2% |
| Buttocks | 6 | 1.9% |
| Breasts | 4 | 1.3% |
| 2 locations | 19 | 7% |
| 3 or more locations | 96 | 35.4% |
| Total | 271 | 100% |
More of the victims in the 37 cases with 3 or more attackers had extragenital injuries (22 cases; 9%), in comparison with the victims without extragenital injuries (15 cases; 3.8%). These results are statistically significant (P=.006).
In half of the 119 cases of SCS (60 cases; 50.4%), the victim had no extragenital physical injuries. These results are statistically significant (P=.004).
More than half of the victims with extragenital physical injuries also had anogenital physical injuries (62 cases; 59%). These results are statistically significant (P<.001).
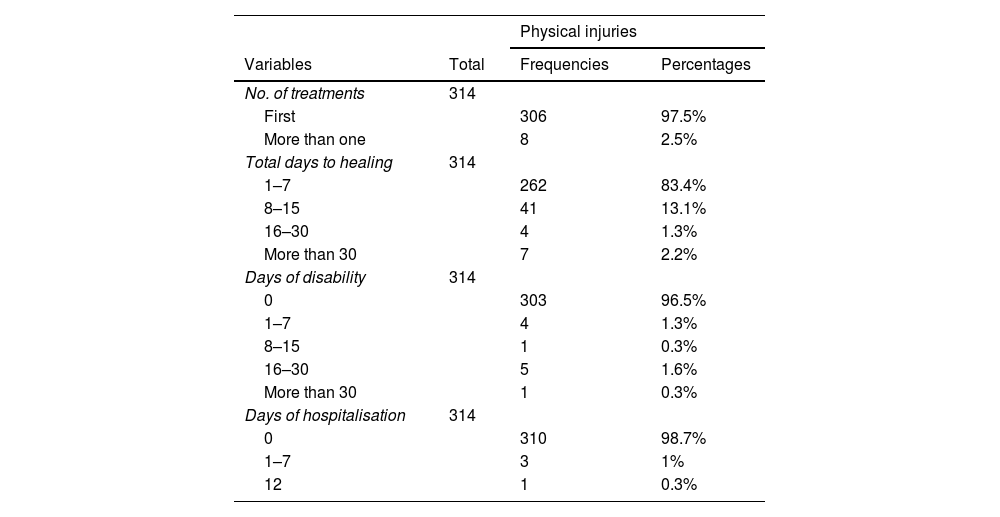
The evolution of physical injuries, required treatment, time taken to heal, and sequelaeIn the group of victims with physical injuries, the great majority required initial medical assistance for treatment or stabilisation (306 cases; 97.5%). Only 8 cases (2.5%) required more than 1 medical treatment (Table 5).
Expert assessment of sexual violence victims with physical injuries.
| Physical injuries | |||
|---|---|---|---|
| Variables | Total | Frequencies | Percentages |
| No. of treatments | 314 | ||
| First | 306 | 97.5% | |
| More than one | 8 | 2.5% | |
| Total days to healing | 314 | ||
| 1–7 | 262 | 83.4% | |
| 8–15 | 41 | 13.1% | |
| 16–30 | 4 | 1.3% | |
| More than 30 | 7 | 2.2% | |
| Days of disability | 314 | ||
| 0 | 303 | 96.5% | |
| 1–7 | 4 | 1.3% | |
| 8–15 | 1 | 0.3% | |
| 16–30 | 5 | 1.6% | |
| More than 30 | 1 | 0.3% | |
| Days of hospitalisation | 314 | ||
| 0 | 310 | 98.7% | |
| 1–7 | 3 | 1% | |
| 12 | 1 | 0.3% |
The time taken to heal in the group of victims with physical injuries ranged from 1 to 180 days. The majority of cases healed in the first week (262 cases; 83.4%) and only 3 cases required more than 60 days. The most common time period was from 3 to 4 days, with 141 cases (44.9%).
Eleven (3.5%) of the victims in the group with physical injuries were unable to perform their usual occupations and/or work for from 3 to 60 days. Only 6 victims (1.9%) suffered disability during more than 15 days.
Four (1.3%) of the victims with physical injuries were hospitalised for from 1 to 12 days. One of the victims had head injuries with parietal haematoma. Victim number 2 had fragmented fractures in the face, injury to a tooth, and an eye injury. Victim number 3 had tearing and pulling out of the whole mobile part of the tongue and a probable fracture of the right ankle. Another of the victims had a complete vaginal tear with involvement of the anal sphincter and rectum.
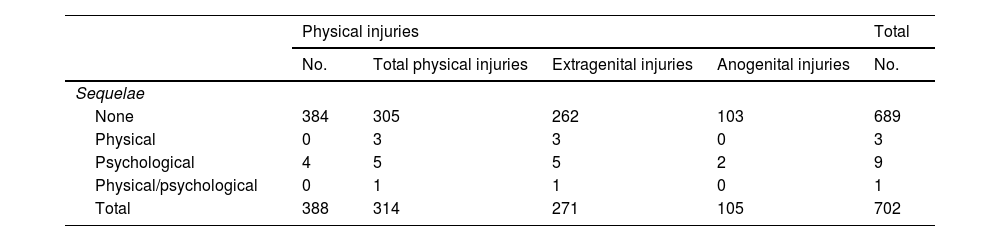
The great majority of the group of victims with physical injuries healed without sequelae (305 cases; 97.1%). In the 9 cases (2.9%) with sequelae, the most frequent were psychological (5 cases; 1.6%), followed by physical ones (3 cases; 1%), with 1 case of physical and psychological sequelae (0.3%) (Table 6). The psychological sequelae were: depression (2 cases; 0.6%), post-traumatic stress disorder (2 cases; 0.6%), while the diagnosis was not shown in 2 cases (0.6%). The physical sequelae consisted of: the partial breakage of the upper central incisors, maxillofacial osteosynthesis material, and right facial hypoesthesia and the absence of tooth number 23.
The presence of sequelae in sexual violence victims with physical injuries.
| Physical injuries | Total | ||||
|---|---|---|---|---|---|
| No. | Total physical injuries | Extragenital injuries | Anogenital injuries | No. | |
| Sequelae | |||||
| None | 384 | 305 | 262 | 103 | 689 |
| Physical | 0 | 3 | 3 | 0 | 3 |
| Psychological | 4 | 5 | 5 | 2 | 9 |
| Physical/psychological | 0 | 1 | 1 | 0 | 1 |
| Total | 388 | 314 | 271 | 105 | 702 |
The result of the analysis of biological sampling (swabs of the victim's body and/or clothing) was positive in 76.2% of the victims with physical injuries (P<.001).
DiscussionOf the total sample of 702 cases that were studied, 44.8% of the victims had physical injuries. This result is similar to those of other previous studies reported in the scientific literature,6,11,12 and the figure is somewhat lower than it was in other studies.11
Factors that increase vulnerability in cases of violence with physical injuriesThe vast majority of SV victims with physical injuries in our sample were women (95.5%). In terms of age, the group from 18 to 27 years old had the highest proportion of injuries (31.3%). This finding is similar to those of other previous studies,2 although our study differs from others in that injuries appear in older age groups of 45 or more years.12
In our study of a total sample of 702 cases, SV victims often mentioned having voluntarily consumed substances prior to the events, basically alcohol (in 46.9% of the total sample),10 which is similar to the findings in other studies.2,6,13 This figure is much higher in the group of victims with physical injuries (62.3%). Alcohol consumption may make the victim more vulnerable in a way that the attacker takes advantage of,14 with an increased risk of suffering injuries.12
The majority (73.5%) of victims in the group with physical injuries sought medical assistance in the first 24 h, and this is similar to findings in other studies.13 It is well-known that the probabilities of observing an injury, above all at anogenital level, fall as time passes.2,15,16 Nevertheless, it must also be taken into account that an examination immediately after the attack may also be limited by the fact that some injuries, such as haematomas, may be less evident in the first 48 h.11,17
In our study, as in other previous ones,2,11,15,17 the number of aggressors is not linked an increase in anogenital injuries (P=.972). However, we did find a significant increase in extragenital injuries when 3 or more attackers took part (9%).
In the same way that other authors have described,6,12 in our study in the group of victims with physical injuries, the risk of physical injuries is significantly higher when the attacker was a stranger who the victim had met recently (52.6%), unlike other studies where this risk is higher when the attacker was known.16
With respect to the type of sexual aggression, in our work, in the group of victims with physical injuries vaginal penetration was the most common type (50.4%), followed by penetration in more than 1 location (25.6%). Penetration occurred with an object in 4 cases, and no anogenital injuries were found in these cases, confirming the previously published findings of other authors.2,6
The result of biological analysis was positive in 76.2% of the victims with injuries, and this differs from other studies which found no significant relationship with the presence of physical injuries.17
In a similar way to other works, we found that the 119 cases with SCS had fewer physical injuries than the other victims.18 This was so for anogenital injuries2,19 as well as extragenital ones.19
Frequency and location of physical injuriesFifteen percent of the victims with physical injuries were found to have anogenital injuries, which is similar to the findings of other studies11,19–21 and somewhat lower than the results obtained by other authors.2,5,12,17 The most frequent locations of the said anogenital injuries were at vaginal level (23.2%), which is similar to the findings in other studies,2,6,16 followed by the anal region (6.1%), and these results are somewhat lower than those found by other authors.2 The most common types of genital injury found were erosion (4.4%) and tearing (3.4%), and these results are along the same line as those obtained by other authors.2,5,11,12 The most frequent location was the introitus (2.1%), followed by the hymen (1.7%).
Anogenital injuries are very important in demonstrating that sexual contact may have occurred, although it is generally not possible to deduce the mechanism or whether the said contact was consensual or not.1 On the other hand, the anogenital injuries detected by simple visual inspection are sometimes hard to interpret, and they may be confused with other causes (such as infection). On other occasions, they may be minor atypical findings that do not represent an injury due to SV (epithelial changes or injuries due to ordinary washing, etc.).1 Some authors recommend the use of visual aids such as staining techniques (toluidine blue) and/or the use of colposcopy.5,17 In any case, the recommendation is that such aids be employed by staff who are trained and accustomed to use them, due to the high frequency of non-specific injuries.1,4,6
The absence of anogenital injuries does not rule out sexual violence, in the same way that their presence does not confirm it, so that each case should be examined within its context.1,4,13 The fact that consensual relations may also leave injuries should also be taken into account.1,4,22 If the courts are to properly approach situations of SV they must analyse all of the elements involved, including the quality of the report by the victim3,4 and diagnostic evidence such as secondary traumatic injuries caused by penetration, sexually transmitted diseases,23 the presence of the attacker's sperm and/or DNA,1 and pregnancy with a positive paternity test.
Similarly to the findings described by other authors, in our study, extragenital physical injuries were more common than anogenital ones. Extragenital injuries were found in 38.6% of the cases of victims with injuries,11,13,20,21 although the results here are slightly lower than those reported by other authors.2,12,16,17,19
The presence of extragenital injuries suggests that the attacker used physical force,6 and the degree of resistance offered by the victim is considered to be an important factor in how the victim and others perceive SV. It is for this reason that many victims are less disposed to report a crime.1
The most common locations for some of these extragenital injuries, even when they are not highly visible, are especially significant and important in helping to confirm or question the victim's description of events.1,4
In our study, 59% of the 22.9% of the victims with extragenital physical also had anogenital injuries, showing that physical injuries in general are associated with a higher risk of suffering anogenital injuries, confirming findings published beforehand in other studies.2
As we have seen, many SV victims may not be found to have physical injuries when examined, and this should not lead to the exclusion of previous SV.1,6,17 In our study, 53.3% of the victims had no injuries recorded in their history, and this is along the same line as other works, although with lower figures.20,11 Not all victims of SV respond with physical resistance, as a common reaction is to feel paralysed, especially when the victim fears for their life or in cases when they have previously been in a situation of inferiority12.
Severity of physical injuriesThe victims in our study suffered slight physical injuries, and in the great majority of cases they only required a single episode of medical assistance for stabilisation or healing (97.5%).
In the group of victims with physical injuries, they took 1 week or less to heal in 83.4% of cases. Severe injuries were only observed in 4 cases, one of which required hospitalisation during 12 days. These results are along the same line as those of other studies.5,6,17,24,25
As SV victims recover they may suffer physical sequelae, sequelae caused by sexually transmitted diseases, psychological sequelae, and others. In our study, 97.1% of the victims with physical injuries healed without sequelae.
Of the 9 cases which healed with sequelae, 6 suffered psychological sequelae. These figures are considered to be very low, so that it is more than probable that lack of follow-up of the victims would explain the low percentage of sequelae in our study. SV is a highly stressful traumatic event, and the victim usually perceives it to be a threat against their life or integrity. It may cause disorders such as depression and post-traumatic stress disorder, among other psychological consequences.26–28 Equally, in medical terms, the majority of victims are found to show a low level of adherence to medical indications, and they do not complete the recommended follow-up.17,20,21
Our study has limitations. Although its sample contains an important number of cases, it is composed of victims who decided to report the crime and/or request the attention of a forensic doctor, so that cases which were not reported are excluded. On the other hand, some variables correspond to lost data, when the standard document and/or the forensic report do not contain the information and/or are incomplete. It should also be taken into account that these are victims who were seen are after reporting a sexual attack which may not have occurred, so that this may distort data gathering. The results obtained should therefore be compared with the number of situations where SV is suspected or reported, without necessarily inferring that all of them correspond to attacks which actually occurred.
It should also be taken into account that this sample excluded the situations in which the victim died as a result of the attack, as this may lead to results which are abnormally slanted towards a low degree of injury severity.
ConclusionsIn our study, the group of SV victims with physical injuries are associated with factors that increase vulnerability: female sex (95.5%), an age from 18 to 27 years (31.3%) and the previous voluntary consumption of substances, fundamentally alcohol (50%).
Our study confirms that anogenital injuries are rare in the majority of sexual violence victims with physical injuries (15%), so that the absence of such injuries cannot be supposed to exclude sexual violence.
The majority of the physical injuries in sexual violence victims are slight (97.5%) and only a small percentage of victims had sequelae (2.9%), although this result may be associated with the lack of victim follow-up.
It is necessary to underline the importance of correctly documenting findings during the initial examination, with the use of precise descriptive terms, as well as the need to subsequently follow-up and monitor the victims medically as well as for forensic purposes. Assistance should be provided by staff with specialised training, and it should be protocolised and given by multidisciplinary teams, with the aim of providing the victims with better care, carrying out a suitable diagnosis, and properly guiding the recovery process.
Ethical responsibilitiesThe authors declare that personal rights to privacy were respected at all times.
FinancingThe authors declare that this study received no specific grant from public, private or not-for-profit sector agencies.
Please cite this article as: Vega-Vega C, Navarro-Escayola E, Bañón-González R. Valoración de las lesiones físicas en 702 casos de violencia sexual en la provincia de Alicante (2016–2020). Revista Española de Medicina Legal. 2023. https://doi.org/10.1016/j.reml.2023.04.003.