Basic symptoms consist of subtle sub-clinical disturbances subjectively experienced by schizophrenia patients. These are mainly related to drive, affect, thinking and language, perception, memory, motor action, central vegetative functions, control of cognitive processes, and stress tolerance. Initially described by Huber, from a phenomenological approach, basic symptoms are part of the earliest features of schizophrenia, and they can evolve along the course of the disorder. Their assessment during the prodromal phase of the disease (together with ultra-high risk criteria) is one of the 2 main approaches that allow the definition of states of clinical risk for the development of psychosis. The present review provides an updated view of the concept of basic symptoms, highlighting its potential value in establishing neurobiological correlates of interest in aetiopathogenic research.
Los síntomas básicos consisten en sutiles molestias subclínicas, experimentadas subjetivamente por el paciente, principalmente referidas a la volición, la afectividad, el pensamiento y lenguaje, la percepción, la memoria, la acción motora, las funciones vegetativas centrales, el control de procesos cognitivos auomáticos y la tolerancia al estrés. Descritos inicialmente por Huber, desde una aproximación fenomenológica, forman parte de las manifestaciones más precoces de la esquizofrenia, a lo largo de cuyo curso pueden adquirir diferente evolución. Su presentación durante la fase prodrómica de la enfermedad, para cuya evaluación han sido desarrollados diferentes instrumentos, constituye (junto con los criterios ultra-high risk) una de las 2 principales aproximaciones para su caracterización, lo que permite definir estados clínicos de riesgo para el desarrollo de psicosis. En la presente revisión se ofrece una visión actualizada del concepto de síntomas básicos, subrayando su potencial valour a la hora de establecer correlatos neurobiológicos de interés en la investigación etiopatogénica.
Over the past 20 years there has been increasing interest in the study of the early stages of schizophrenia and advances in the characterisation and knowledge of the clinical expression of the disorder, even from its prodromal phases. This has major implications in terms of the detection of the disorder and early intervention.1–11
The diagnostic characterisation of schizophrenic psychoses has been fundamentally underpinned by studying its clinical symptomatology, and the core description of the disorder has converged into a constellation of symptoms focusing on so-called positive and negative symptoms which, subsequently and from a dimensional approach, would extend into disorganised, affect, motor and cognitive symptoms.12 This is borne out by the operational criteria adopted in the various diagnostic systems which have appeared in recent years. One of the most recent and representative examples of these are the DSM-5 criteria for the disorder.13
It is probable that the major reason behind this fact is that the abovementioned clinical symptomatology enables a clinical objective for study to be established. An analysis of the reasons behind this development goes beyond the purpose of this article, but, from a historical perspective, one only needs to refer to Cromwell's14 observation that psychopathology has traditionally been described in terms of a subject's “deviations” from the norms and expectations of their social group. Thus, in relation to the more or less disruptive or “threatening” nature of the disease, “tolerable” manifestations–principally behavioural deficits–and “intolerable manifestations”–principally clinical symptoms–can be distinguished. In fact, research undertaken thus far follows these same lines, essentially focussing on the “intolerable” manifestations, whereas the more “subtle” and “inoffensive” manifestations (such as alterations in the processing of information and cognitive deficits, amongst others) have been largely underestimated or ignored.15 This trend has been addressed in recent years through the study of cognitive deficits7,16,17 and other symptomatic domains, such as negative symptoms18–20 and their impact on functionality.7,12,21
Similar reasoning might be applied to the set of manifestations in the incipient stages of the disorder, which are frequently expressed as complaints or psychological distress with relatively non-specific and insidious characteristics.22 In this regard, the description of the prodromal manifestations of the disease has progressed from the initial retrospective studies of first psychotic episodes23,24 to the establishment of criteria to identify individuals at high risk of transition to psychosis, (at-risk mental state; ultra-high risk [UHR]).25 In recent years, to some extent, to some extent the predominant approach in characterising these stages.
However, particularly if we look at the order of the more subjective manifestations, a complementary approach to characterising prodromal symptomatology, as well as an important body of research, are to be found in the study of abnormal subjective experiences and, specifically, in the conceptual framework of the so-called basic symptoms, developed in Germany by Gerd Huber and the Bonn school.26,27 The phenomenological approach that these authors introduce will contribute towards better clinical profiling of those most at risk of developing psychosis, and towards the study of possible underlying neurobiological correlates of pathophysiological or aetiological interest.
The objective of this review is to offer an updated vision of the concept of the basic symptoms and their expression and assessment in schizophrenia, taking into account their contribution from a phenomenological perspective. Furthermore, we shall review their relevance in characterising the prodromal stage of the disorder and their predictive value for the development of the disease.
A brief historical overviewThe first thorough attempt to describe and research patients’ subjective experiences can be attributed to Jaspers, who was followed by other members of the Heidelberg school (Gruhle, Mayer-Gross, and Schneider). Based on Husserl's Phenomenology, Jaspers establishes a “return to the things themselves”–his phenomenological method. His objective was to intuitively capture the “essence” of the patients’ subjective and experiential world, without imposing any prior theoretical framework–which would have to be “understood” and “explained” subsequently. Thus the development of phenomenological psychopathology, although frequently undervalued despite its epistemological wealth, is a descriptive method of real interest in the study of subjective experiences and in understanding the sense of a disease, in this case, schizophrenia.28
The study of the abnormal subjective experiences of schizophrenia is part of this tradition, although to some extent its scope overlaps and extends to self-disturbances (Ich Störungen). Through the works of authors such as Minkowsky and Blankenburg, these anomalies have been reconceptualised more recently as a core aspect of the disorder as demonstrated by approaches which would imply a disturbed pre-reflexive self-consciousness,29–31 or include metacognitive aspects.32
Furthermore, the origins of the current distinction of the premorbid, prodromal and psychotic stages of schizophrenia33 lie in the attention paid by some authors at the time to the precursor syndromes and to the initial manifestations of the disorder. Here, Conrad's34 description of “incipient schizophrenia” is worth mentioning, and his attempt to demonstrate the connection between the different phenomena of the schizophrenic experience, both in its prodromal forms and subsequent stages of development.
In turn, the phenomenological school of Bonn, lead by Gerd Huber, was to contribute essential ideas on the characterisation of the prodromal symptomatology of the psychoses.35,36 Along these same lines, the works of Gross, Süllwold37 and Klosterkötter are worth noting, and to a lesser extent, those of other Anglo-American authors.23,24
Huber's model of basic “substrate-close” psychotic symptoms is fundamentally based on long-term cohort studies of defectual patients. Huber establishes the concept of “basic symptoms” which are hypothetically neurobiological “substrate-close” (Substratnahe Basissymptome), as follows26: “Psychotic symptoms presenting in schizophrenic patients as primary subjective experiences that constitute the basis of complex psychotic symptoms and that can be supposed to be found closer to the neurobiological substrate. They are, therefore, negative symptoms, characterised as complaints by the patients which, from a phenomenological point of view, broadly coincide with premonitory and pre-psychotic prodromal symptoms and which, in the reversible basic stages and the irreversible pure defectual syndrome are perceived and expressed as deficiencies, shortcomings or disorders.”
Thus, Huber underlines the primary and, largely, subjective nature of these manifestations, whereas observable behaviour would constitute a secondary, coping, response to them. The catamnestic studies of Heidelberg and Bonn enable the various typologies and developmental possibilities of the basic symptoms to be outlined, and their structural location to be determined from a phenomenal point of view.26,36,38,39
Basic symptoms in schizophrenia: concept, characterisation and psychopathological relationshipsThe “basic symptoms”, also known as anomalous subjective experiences (because they are not observable externally and refer to non-psychotic alterations of experience), consist of subtle, subclinical complaints principally of volition, affect, thinking and language (speech), (body)perception, memory, motor action, central vegetative functions, control of automatic cognitive processes, and stress tolerance.27,40–42 By definition, these are complaints which are experienced subjectively and, although they are sometimes difficult to describe, are recognised as anomalies by the patients themselves, which distinguishes them from the positive and the negative symptoms.
The basic symptoms are the earliest symptoms which the patient experiences subjectively. However, they can occur in all stages of the disease, as pre-psychotic syndromes, in the prodromal phase of the first psychotic episode, in the prodromes of relapse, in residual states or even during the same psychotic episode, although their assessment and self-assessment in the latter case is hindered by the prominence of the symptoms themselves.42 Although potentially reversible, the symptoms would constitute an essential component of the prodromal and residual stages, and can be considered to be the most immediate symptomatic expression of the neurobiological substrate of the disease. Hence their being termed “basic” and the essential nature of the disorder, over which productive psychotic symptoms would fluctuate.40,43
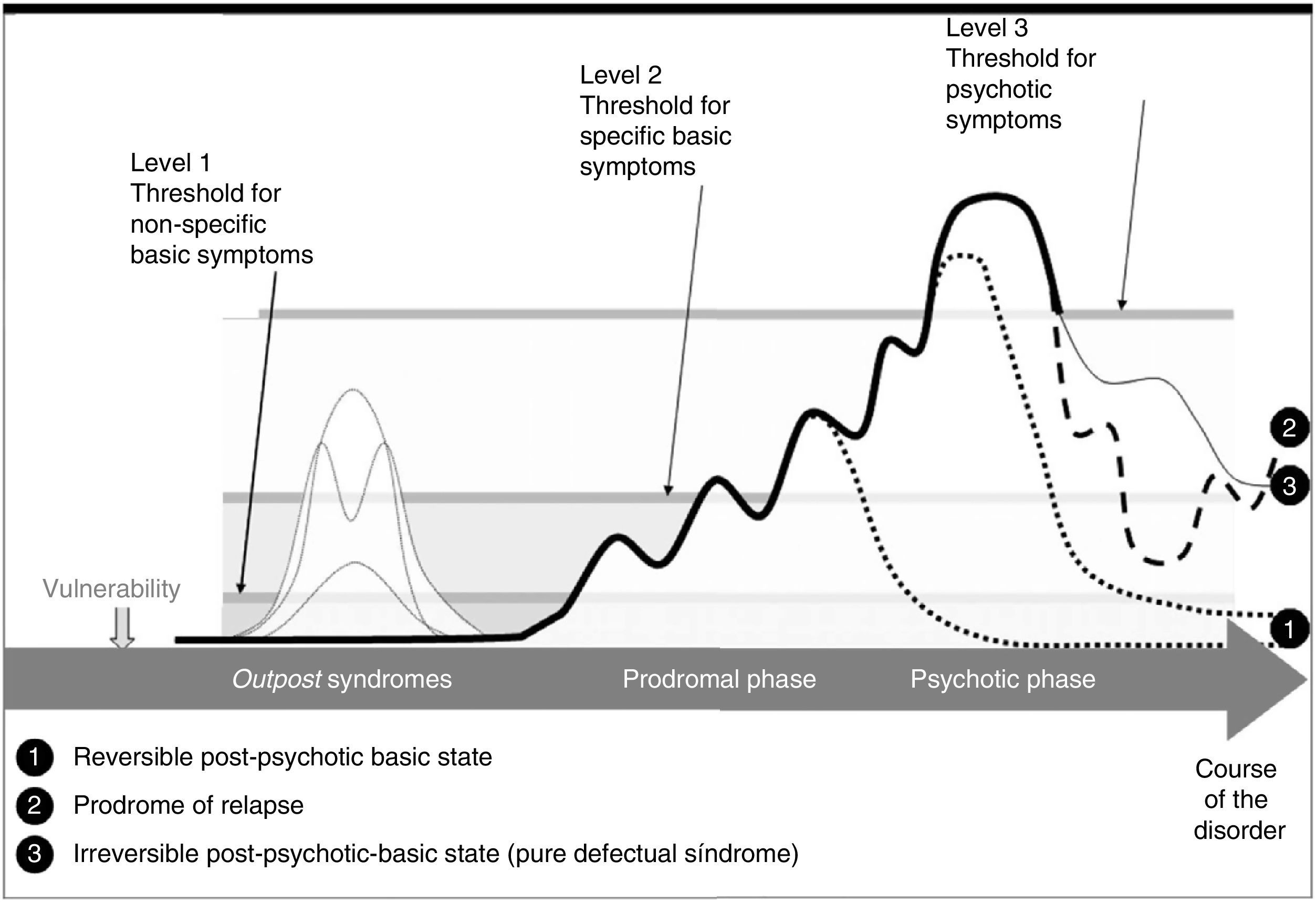
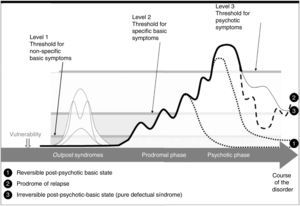
Taking the original concept into account, the early symptoms of the psychosis will evolve in 3 forms or levels of development40,42:
- i.
Level 1 or “non-specific”. Complaints principally of volition, affect, concentration and memory.
- ii.
Level 2 or “specific”. Qualitatively different complaints, particularly referring to the area of thought, language, bodily perception and motor action.
- iii.
Level 3. Psychotic symptoms as such, including first rank Schneiderian symptoms.
These levels of development, which have been shown to be potentially reversible, demonstrate the existence of a continuum at a psychopathological level. Thus a particular somatic hallucination (level 3), could revert to a coenesthetic feeling (level 2) and this, in turn, to a non-specific somatic feeling (level 1).40
The overall developmental sequence of the basic symptoms varies (Fig. 1).40,42 After the onset of level 1 symptoms, symptoms tend to increase in number and severity until psychotic symptoms present. However, occasionally, basic level 1 or 2 symptoms can improve temporarily or even remit before the symptomatic threshold is reached. These symptomatic phases without conversion to psychosis can imitate prodromal stages, known as outpost syndromes because they announce subsequent real prodromes.36 In fact, these first manifestations can precede the first psychotic manifestations by about 10 years.40
Furthermore, the emergence of level 2 symptoms or their conversion to level 3 might be triggered by everyday situations and would exceed the already vulnerable capacity for processing information. These symptoms can be compensated for as long as they do not outweigh the personal resources or strategies of the patient, and therefore they can go unnoticed by others. Otherwise the subject might start to demonstrate avoidance behaviours, isolation behaviour or other functional deficits.
Following the first frank episode, the basic symptoms can evolve into 3 categories or post-symptomatic basic stages:
- (i)
A reversible post-symptomatic basic stage, characterised by complete remission of the basic symptoms.
- (ii)
A prodromal stage of relapse, which might evolve into a second episode from an asymptomatic or paucisymptomatic stage.
- (iii)
An irreversible post-symptomatic basic stage or pure defectual syndrome, with the presence of basic symptoms level 1 and 2, principally, volition, affect, cognitive and stress tolerance, with functional repercussions.
The fact that there can be an overlap, which is difficult to distinguish in a strict sense and from a phenomenological point of view, between the manifestations of the 4 stages described (precursor or advanced syndromes, prodromes, basic post-symptomatic reversible stage and pure defectual syndrome) led the authors to refer to the basic stages in the broad sense,26,40 as opposed to the basic symptoms in the strict sense (basic symptoms present after an acute phase which remit over the course of a few weeks or months).
The basic symptoms constitute, therefore, an integral part of the psychoses, and they can present throughout the different stages of the disease.42 Considerable prevalence of the symptoms has been demonstrated.44
Their relationship with various psychopathological aspects of the disorder has been examined, including the Schneiderian and the Bleularian typologies,45 positive and negative schizophrenia,46 different neuropsychological deficits,47 different psychopathological dimensions,48,49 psychotic symptomatology in different stages of the disease50 or their dimensional structure already in the prodromal stage.51
Although the basic symptoms would not be specific to schizophrenia and might present in other conditions, such as mood disorders,44,52 some of them, especially those belonging to the cognitive and perceptual sphere, would appear to demonstrate greater specificity for the development of a psychosis,53,54 although this specificity has been downplayed in subsequent re-analyses.55
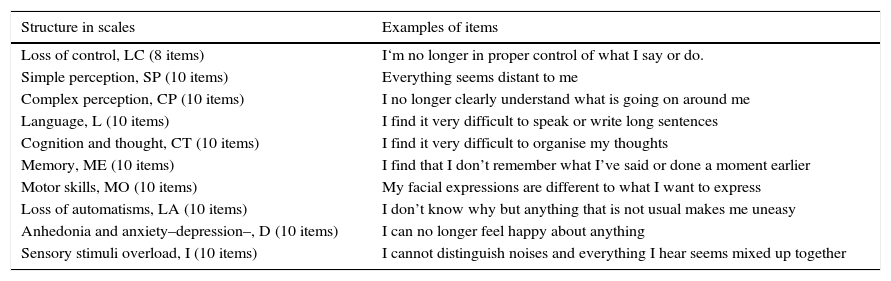
Examination and assessment instrumentsVarious instruments have been designed in order to assess the presence of basic symptoms. The Bonn scale for the assessment of basic symptoms (Bonner Skala für die Beurteilung von Basissymptomen)56 and the Frankfurt Complaint Questionnaire (Frankfurter Beschwerde-Fragebogen)37 have been the most widely used, in our environment as well.57–59 By way of an example, and to show their content and structure, some of the 98 items of the third version of the Frankfurt Complaint Questionnaire are given in Table 1, which can be grouped according to two structures, either by scale or by dimensional factor.37,58,60
Estructure and content of the Frankfurt Complaint Questionnaire version 3.
| Structure in scales | Examples of items |
|---|---|
| Loss of control, LC (8 items) | I‘m no longer in proper control of what I say or do. |
| Simple perception, SP (10 items) | Everything seems distant to me |
| Complex perception, CP (10 items) | I no longer clearly understand what is going on around me |
| Language, L (10 items) | I find it very difficult to speak or write long sentences |
| Cognition and thought, CT (10 items) | I find it very difficult to organise my thoughts |
| Memory, ME (10 items) | I find that I don’t remember what I’ve said or done a moment earlier |
| Motor skills, MO (10 items) | My facial expressions are different to what I want to express |
| Loss of automatisms, LA (10 items) | I don’t know why but anything that is not usual makes me uneasy |
| Anhedonia and anxiety–depression–, D (10 items) | I can no longer feel happy about anything |
| Sensory stimuli overload, I (10 items) | I cannot distinguish noises and everything I hear seems mixed up together |
| Structure by factor | |
|---|---|
| Central cognitive disorders (loss of automation) F1 (11 items) | When people use long sentences to talk to me, I find it particularly difficult to understand what they mean |
| Perception and motor functioning F2 (15 items) | People's faces look strange to me and out of place |
| Depressivity F3 (14 items) | I’m afraid of almost everything that will happen to me throughout the day |
| Internal and external overstimulation (hypervigilance, confusion) F4 (9 items) | When people are talking or moving around me, I find it distressing and I have to distance myself or go away to recover my inner balance |
| Assessment | |
|---|---|
| Award a score per item, per scale, total score and by factor. Direct scores can be turned into percentage scores, which can be interpreted according to vulnerability to schizophrenia. The items are assessed from two perspectives: |
Frequency of presentation: never/sometimes/often/always.
Degree of complaint or distress: none/very little/some/high.
Other, less frequently used instruments are the Intentionality Scale (IntentionalitätsSkala, Inska),61 the Frankfurt Well-being Scale (Frankfurter BefindlichkeitsSkala),62 and the Günzburg Self Assessment Scale of Basic Symptoms (Günzburger Selbstbeurteilungsskala für Basissymptome).63
Furthermore, in the genealogy and the progressive development of instruments for the assessment of the prodromal symptoms of the psychoses, it is worth including those which establish their criteria from the presence, total or partial, of certain basic symptoms, as we shall detail below.64
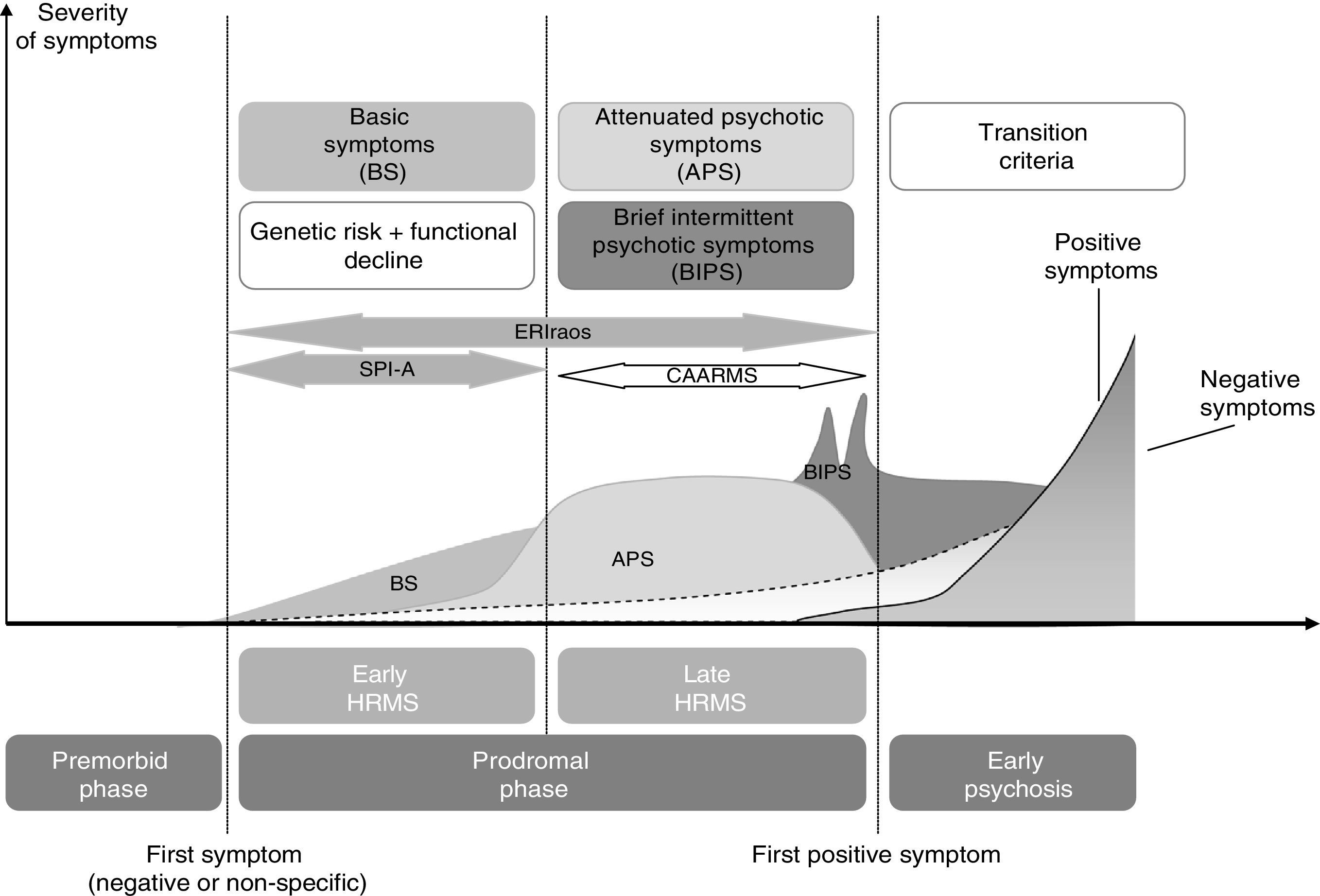
The basic symptoms in the prodromal stage and their study as risk predictors for the development of psychosisAs mentioned earlier, 2 approaches have governed research into the characterisation of the prodromal manifestations of schizophrenia: UHR and basic symptoms.65
In summary, the widely applied UHT criteria which seek to define the prodromal states which, at a symptomatic level, indicate an imminent risk of transition to psychosis, include 3 types of situations: (i) attenuated psychotic symptoms; (ii) brief limited intermittent psychotic symptoms and (iii) genetic risk and deterioration syndrome.22
The application of these criteria and the estimation of their potential predictive value in relation to the development of the disease66 could be applied analogously in the characterisation of the prodromal phase established from the presence of basic symptoms, which, as mentioned earlier, constitutes the other principal approach. Using this same argument, the corresponding risk of transition to the disease could be estimated in a similar way.64,66
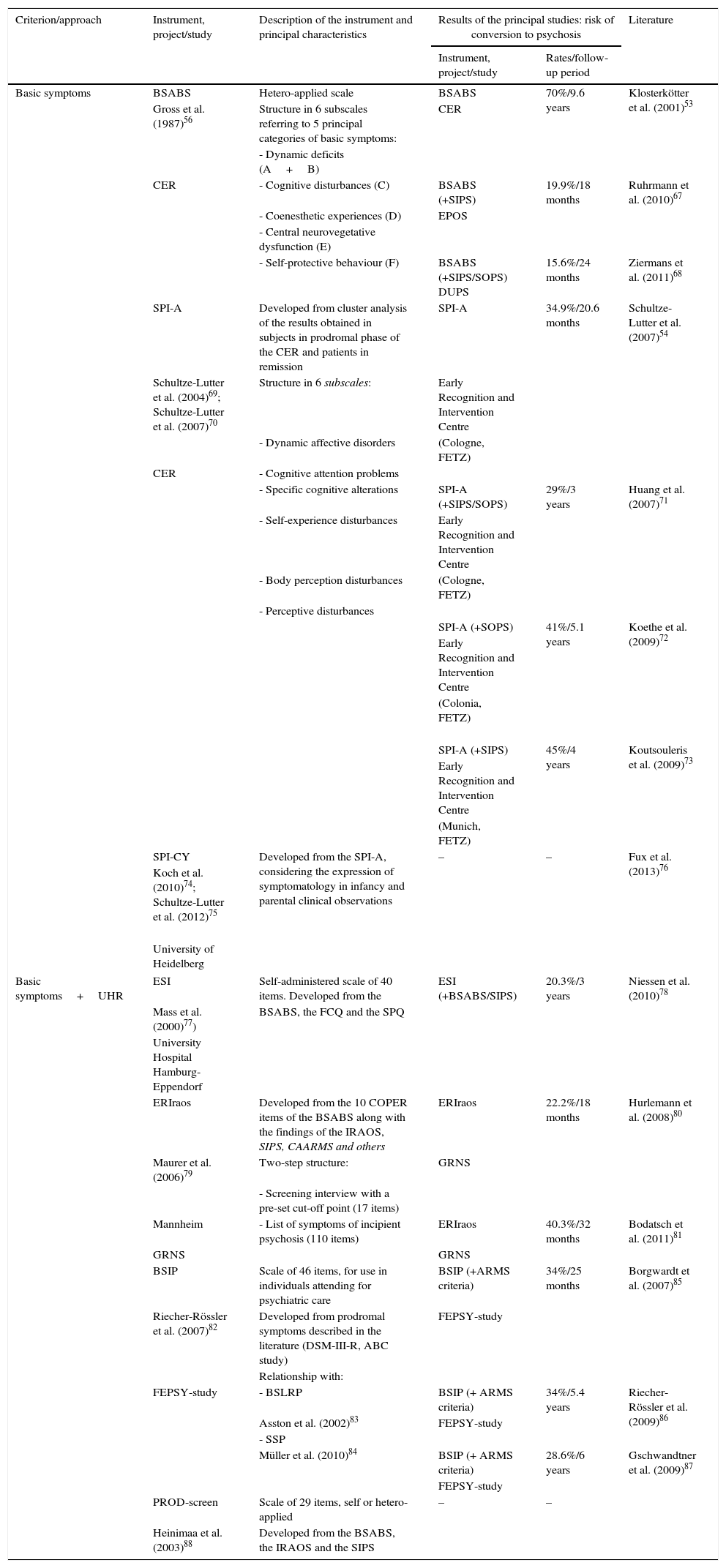
This section reviews the literature on the instruments which, as their selection criteria, cover the following criteria: (i) whose construct includes, totally or partially, the evaluation of items relating to the presence of basic symptoms, and (ii) which have been applied in studies in which the risk of conversion to psychosis has been estimated.
Table 2 shows the most relevant data obtained from the application of these instruments in the different studies undertaken over recent years.64,66
Principal instruments and studies developed based on the inclusion of criteria of basic symptoms in the evaluation of prodromal symptomatology and estimations of the risk of conversion to psychosis.
| Criterion/approach | Instrument, project/study | Description of the instrument and principal characteristics | Results of the principal studies: risk of conversion to psychosis | Literature | |
|---|---|---|---|---|---|
| Instrument, project/study | Rates/follow-up period | ||||
| Basic symptoms | BSABS | Hetero-applied scale | BSABS | 70%/9.6 years | Klosterkötter et al. (2001)53 |
| Gross et al. (1987)56 | Structure in 6 subscales referring to 5 principal categories of basic symptoms: | CER | |||
| - Dynamic deficits (A+B) | |||||
| CER | - Cognitive disturbances (C) | BSABS (+SIPS) | 19.9%/18 months | Ruhrmann et al. (2010)67 | |
| - Coenesthetic experiences (D) | EPOS | ||||
| - Central neurovegetative dysfunction (E) | |||||
| - Self-protective behaviour (F) | BSABS (+SIPS/SOPS) DUPS | 15.6%/24 months | Ziermans et al. (2011)68 | ||
| SPI-A | Developed from cluster analysis of the results obtained in subjects in prodromal phase of the CER and patients in remission | SPI-A | 34.9%/20.6 months | Schultze-Lutter et al. (2007)54 | |
| Schultze-Lutter et al. (2004)69; Schultze-Lutter et al. (2007)70 | Structure in 6 subscales: | Early Recognition and Intervention Centre | |||
| - Dynamic affective disorders | (Cologne, FETZ) | ||||
| CER | - Cognitive attention problems | ||||
| - Specific cognitive alterations | SPI-A (+SIPS/SOPS) | 29%/3 years | Huang et al. (2007)71 | ||
| - Self-experience disturbances | Early Recognition and Intervention Centre | ||||
| - Body perception disturbances | (Cologne, FETZ) | ||||
| - Perceptive disturbances | |||||
| SPI-A (+SOPS) | 41%/5.1 years | Koethe et al. (2009)72 | |||
| Early Recognition and Intervention Centre | |||||
| (Colonia, FETZ) | |||||
| SPI-A (+SIPS) | 45%/4 years | Koutsouleris et al. (2009)73 | |||
| Early Recognition and Intervention Centre | |||||
| (Munich, FETZ) | |||||
| SPI-CY | Developed from the SPI-A, considering the expression of symptomatology in infancy and parental clinical observations | – | – | Fux et al. (2013)76 | |
| Koch et al. (2010)74; Schultze-Lutter et al. (2012)75 | |||||
| University of Heidelberg | |||||
| Basic symptoms+UHR | ESI | Self-administered scale of 40 items. Developed from the | ESI (+BSABS/SIPS) | 20.3%/3 years | Niessen et al. (2010)78 |
| Mass et al. (2000)77) | BSABS, the FCQ and the SPQ | ||||
| University Hospital Hamburg-Eppendorf | |||||
| ERIraos | Developed from the 10 COPER items of the BSABS along with the findings of the IRAOS, SIPS, CAARMS and others | ERIraos | 22.2%/18 months | Hurlemann et al. (2008)80 | |
| Maurer et al. (2006)79 | Two-step structure: | GRNS | |||
| - Screening interview with a pre-set cut-off point (17 items) | |||||
| Mannheim | - List of symptoms of incipient psychosis (110 items) | ERIraos | 40.3%/32 months | Bodatsch et al. (2011)81 | |
| GRNS | GRNS | ||||
| BSIP | Scale of 46 items, for use in individuals attending for psychiatric care | BSIP (+ARMS criteria) | 34%/25 months | Borgwardt et al. (2007)85 | |
| Riecher-Rössler et al. (2007)82 | Developed from prodromal symptoms described in the literature (DSM-III-R, ABC study) | FEPSY-study | |||
| Relationship with: | |||||
| FEPSY-study | - BSLRP | BSIP (+ ARMS criteria) | 34%/5.4 years | Riecher-Rössler et al. (2009)86 | |
| Asston et al. (2002)83 | FEPSY-study | ||||
| - SSP | |||||
| Müller et al. (2010)84 | BSIP (+ ARMS criteria) | 28.6%/6 years | Gschwandtner et al. (2009)87 | ||
| FEPSY-study | |||||
| PROD-screen | Scale of 29 items, self or hetero-applied | – | – | ||
| Heinimaa et al. (2003)88 | Developed from the BSABS, the IRAOS and the SIPS | ||||
ARMS, at-risk mental state; BSABS, Bonn Scale for the Assessment of Basic Symptoms; BSIP, Basel Screening Instrument for Psychosis; BSLRP, Basel Screening List for Risk of Psychosis; CAARMS, Comprehensive Assessment of At-Risk Mental States; CER, Cologne Early Recognition; COPER, COgnitive-PERceptive basic symptoms; DUPS, Dutch Prediction of Psychosis Study; EPOS, European Prediction of Psychosis Study; ERIraos, Early Recognition Inventory for the Retrospective Assessment of the Onset of Schizophrenia; ESI, Eppendorf Schizophrenia Inventory; FCQ, Frankfurt Complaint Questionnaire; FEPSY, Früherkennung von Psychosen (The Basel early-detection-of-psychosis); FETZ, Früh-Erkennungs-Therapie-Zentrum für psychische Krisen (Early Recognition and Intervention Centre for Mental Crises); GRNS, German Research Network on Schizophrenia; IRAOS, Interview for the Retrospective Assessment of the Onset and course of Schizophrenia and other psychoses; PROD-screen, Prodromal Screening Symptoms of Psychosis Questionnaire; SIPS, Structured Interview for Prodromal Symptoms; SOPS, Scale of Prodromal Symptoms; SPI-A, Schizophrenia Prediction Instrument-Adult version; SPI-CY, Schizophrenia Prediction Instrument-Child and Youth version; SPQ, Schizotypal Personality Questionnaire; SSP, Self-Screen Prodrome; UHR, ultra-high risk.
The instruments and studies developed from the exclusive use of basic symptoms are distinguished from those that also contain ultra-high risk criteria in their composition.
In general, the rates of conversion to psychosis in patient cohorts identified as being at risk of developing psychosis vary in a range of 10–50% approximately, throughout periods of follow-up from 6 months to 10 years.64 A recent systematic review undertaken on prospective studies to determine the predictive validity of prodromal criteria to identify individuals at high risk of developing schizophrenia66 concluded a sensitivity of 0.81 (95% CI 0.76–0.85) and a specificity of 0.67 (95% CI 0.64–0.70) for UHR criteria. When the basic symptom criteria are applied, a sensitivity of 0.98 (95% CI 0.91–1.00) and a specificity of 0.59 (95% CI 0.48–0.70) are obtained, with a positive predictive value of 0.70 and a negative predictive value of 0.96. The latter figures match the study undertaken by the Cologne Early Recognition Project, from the assessment of the basic symptoms using the Bonn Scale for the Assessment of Basic Symptoms (with a cut-off point determined by the presence of at least one of the 66 basic symptoms selected), where of the 160 individuals likely to be in the prodromal phase, 49.4% will develop schizophrenia over a follow-up period of 9.6 years, whereas an absence of these symptoms ruled out the subsequent development of the disorder in 96% of them.53,89
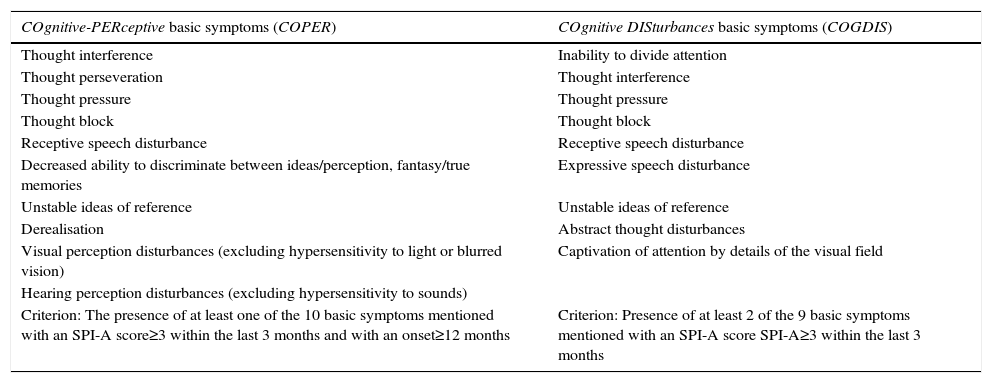
Based on these same findings and 2 other cut-off points, 2 subsets were defined that to some extent overlapped, comprising the basic symptoms showing the highest predictive value.53,54 As can be seen in Table 3, these risk criteria would comprise:
- -
Cognitive-perceptive basic symptom risk factors: comprising 10 basic symptoms, relating to disturbances of cognitive-perceptive dominance, with a sensitivity of 0.87 and specificity of 0.54. These criteria were included in the Early Initial Prodromal State of the German Research Network Schizophrenia.90
- -
High risk criteria relating to cognitive disturbances: comprising the 9 cognitive basic symptoms with the highest predictive value, which were included in the European Prediction Of Psychosis Study,91 with a sensitivity and specificity of around 0.67 and 0.83, respectively.
Basic symptoms included in the COPER/COGDIS risk criteria.
| COgnitive-PERceptive basic symptoms (COPER) | COgnitive DISturbances basic symptoms (COGDIS) |
|---|---|
| Thought interference | Inability to divide attention |
| Thought perseveration | Thought interference |
| Thought pressure | Thought pressure |
| Thought block | Thought block |
| Receptive speech disturbance | Receptive speech disturbance |
| Decreased ability to discriminate between ideas/perception, fantasy/true memories | Expressive speech disturbance |
| Unstable ideas of reference | Unstable ideas of reference |
| Derealisation | Abstract thought disturbances |
| Visual perception disturbances (excluding hypersensitivity to light or blurred vision) | Captivation of attention by details of the visual field |
| Hearing perception disturbances (excluding hypersensitivity to sounds) | |
| Criterion: The presence of at least one of the 10 basic symptoms mentioned with an SPI-A score≥3 within the last 3 months and with an onset≥12 months | Criterion: Presence of at least 2 of the 9 basic symptoms mentioned with an SPI-A score SPI-A≥3 within the last 3 months |
SPI-A, Schizophrenia Prediction Instrument-Adult version.
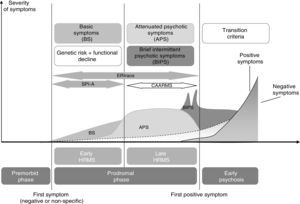
In any case, and going beyond the debate about whether defining these risk profiles might or might not be considered a diagnostic category to be taken into account in the DSM-5 or future classifications, the fact is that the most recent studies have been progressing towards the integration of both approaches. As shown in Fig. 2, the emergence of the symptoms covered under the UHR criteria and the emergence of the basic symptoms themselves would coincide in the prodromal phase, although the latter refer to the earlier phase. In consequence, the tendency has been to include both criteria, which would cover the 3 abovementioned UHR conditions (attenuated psychotic symptoms, brief intermittent psychotic symptoms and genetic risk along with decline in psychosocial functioning) as well as the basic symptoms and certain other unspecified prodromal symptoms. This construct would thus enable criteria to be established to determine clinical psychosis high-risk states.92
Model of the onset of the psychosis based on the concept of “high-risk state”, with the main criteria for characterising the prodromal manifestations of the psychosis, including the basic symptoms, and the main assessment instruments.
CAARMS92, comprehensive assessment of at-risk mental states; HRMS, high-risk mental state; ERIraos, Early Recognition Inventory for the Retrospective Assessment of the Onset of Schizophrenia; SPI-A, Schizophrenia Prediction Instrument-Adult version.
Although the epidemiological estimations in the general population would require further investigation still, a verifiable fact in the population with potential prodromal symptomatology is the increased risk of suffering a psychosis in a relatively short period of time, although in percentages which do not tend to go above 40%. Therefore, this risk of transition in a population with individuals at high risk would be 17.7% after 6 months, 21.7% after one year, 29.1% after 2 years, and 35.8% at 3 years’ follow-up, according to a recent meta-analysis.95 To be specific, this meta-analysis concludes that the mean risk of transition to psychosis established from basic symptom criteria is 48.5% (95% CI 41.9–55.9).
Therefore the studies that would appear most promising currently would be those which present a combined, refined used of criteria.53,67,68 Thus, the simultaneous presence of UHR and cognitive disturbances would appear to be associated with a greater risk of transition to psychosis, introducing a predictive model in 2 stages of risk – early and late.67 In this regard, the most recently reported data using the combination of UHR criteria+cognitive disturbances would produce a risk of conversion to psychosis of 66% at 48 months’ follow-up.96
Discussion and future investigation: the basic symptoms as a marker for vulnerability to psychosis?An initial value which can be attributed to the basic symptoms in clinical practice is precisely the fact that the distress associated with experiencing these symptoms encourages the patient to seek therapeutic help. In this regard it is obvious that the clinical investigation of these symptoms will contribute to better knowledge of their clinical and pathophysiological bases and the bases for their treatment and intervention. A good example of this is the knowledge gained in relation to their relevance during the prodromal phase and their potential predictive value.
However, if we consider the original formulation of the basic symptoms as “hypothetically neurobiological substrate-close”, it is true that after the initial studies underlining the possible role of the limbic system along with a dynamic cognitive deficit essentially attributable to a disturbance in the mechanisms for processing information,26,40 research undertaken in this regard, at least to date, is somewhat scarce. Even so, in so far as the high risk states have been better integrated and characterised, it has been possible to find different neurobiological correlates in these populations on structural and functional neuroimaging.85,92,97 Likewise, studies have been undertaken in which basic symptom criteria have been applied in relation to other validators, whether neurophysiological,87,98 neurochemical71,72 or neurocognitive47,86.
Furthermore, given the essentially cognitive nature of the basic symptoms, and similarly to the way they have been established for different cognitive deficits, more in-depth study on their possible usefulness as markers of vulnerability to the disorder is needed, as well as whether they might constitute a potential endophenotypic candidate. Some studies have been undertaken in this regard, in relation to their presentation in first degree relatives99–102 and in the general, non-psychotic population.103
Finally, and from a phenomenological point of view, the way the list of basic symptoms extends to self-disturbance should be considered, and how it can be integrated with the most recent explanatory models of the illness.104,105
Future research in this direction will doubtless contribute towards a better knowledge of the constitutive elements of the disorder, and towards improved interventions.
Conflict of interestsThe authors have no conflict of interests to declare.
To Centro de Investigación Biomédica en Red de Salud Mental, CIBERSAM.
To the Comissionat per a Universitats i Recerca del DIUE of the Regional Government of Catalonia (2014SGR1636).
Please cite this article as: Miret S, Fatjó-Vilas M, Peralta V, Fañanás L. Síntomas básicos en la esquizofrenia, su estudio clínico y relevancia en investigación. Rev Psiquiatr Salud Ment (Barc.). 2016;9:111–122.