To evaluate the diagnostic performance of a novel deep learning attenuation correction software (DLACS) for myocardial perfusion imaging (MPI) using a cadmium–zinc–telluride (CZT) cardio dedicated camera with invasive coronary angiography (ICA) correlation for the diagnosis of coronary artery disease (CAD) in a high-risk population.
MethodsRetrospective study of 300 patients (196 males [65%], mean age 68 years) from September 2014 to October 2019 undergoing MPI, followed by ICA and evaluated by means of quantitative angiography software, within six months after the MPI. The mean pre-test probability score for coronary disease according to the European Society of Cardiology criteria was 37% for the whole cohort. The MPI was performed in a dedicated CZT cardio camera (D-SPECT Spectrum Dynamics) with a two-day protocol, according to the European Association of Nuclear Medicine guidelines. MPI was retrospectively evaluated with and without the DLACS.
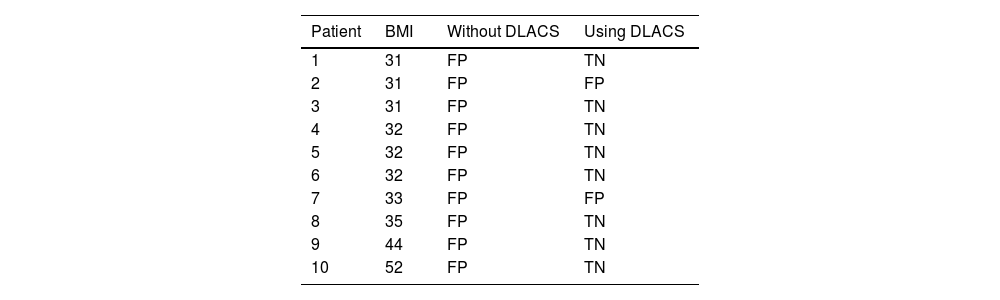
ResultsThe overall diagnostic accuracy of MPI without DLACS to identify patients with any obstructive CAD at ICA was 87%, sensitivity 94%, specificity 57%, Positive Predictive Value 91% and Negative Predictive Value 64%. Using DLACS the overall diagnostic accuracy was 90%, sensitivity 91%, specificity 86%, Positive Predictive Value 97% and Negative Predictive Value 66%.
ConclusionUse of the novel DLACS enhances performance of the MPI using the CZT D-SPECT camera and achieves improved results, especially avoiding artefacts and reducing the number of false positive results.
Evaluar el rendimiento diagnóstico de un nuevo software de aprendizaje profundo para corrección de atenuación (SAPCA) en imágenes de perfusión miocárdica (IPM) utilizando una cámara cardio dedicada de cadmio–zinc–telurio (CZT) con correlación con angiografía coronaria (AC) para el diagnóstico de enfermedad arterial coronaria (EAC) en una población de alto riesgo.
MétodosEstudio retrospectivo de 300 pacientes (196 varones [65%], edad media de 68 años) desde septiembre de 2014 hasta octubre de 2019. Posteriormente realizaron una IPM, seguida de AC dentro de los seis meses posteriores a la IPM. La probabilidad media pre-prueba para EAC según los criterios de la Sociedad Europea de Cardiología fue del 37%. La IPM se realizó en una cámara CZT cardio dedicada (D-SPECT Spectrum Dynamics) usando un protocolo de dos días, de acuerdo con las guías de la Asociación Europea de Medicina Nuclear (EANM). La IPM fue evaluada con y sin el SAPCA.
ResultadosLa precisión diagnóstica general de la IPM sin el SAPCA para identificar pacientes con cualquier EAC obstructiva en la AC fue del 87%, sensibilidad del 94%, especificidad del 57%, valor predictivo positivo del 91% y valor predictivo negativo del 64%. Utilizando el SAPCA, la precisión diagnóstica general fue del 90%, la sensibilidad del 91%, la especificidad del 86%, el valor predictivo positivo del 97% y el valor predictivo negativo del 66%.
ConclusiónEl uso del novel SAPCA mejora el rendimiento diagnóstico de la IPM usando la cámara CZT D-SPECT, especialmente reduciendo el número de resultados falsos positivos al reducir los artefactos.
Semiconductor cadmium–zinc–telluride (CZT) cameras for myocardial perfusion imaging (MPI) have shown superior energy resolution, improved sensitivity and diagnostic specificity rates compared to traditional Anger cameras1 in the evaluation of suspected coronary artery disease (CAD). However, an acknowledged limitation of this technology is the fact that these cameras are susceptible to artefacts from several sources, potentially masquerading CAD.2,3 Additionally, CZT cameras are reported to show satisfactory sensitivity but suboptimal specificity due to the absence of attenuation correction.1
Efforts to achieve better results from MPI have previously been made using attenuation correction by means of low-dose computed tomography (CT)4,5 in order to increase the diagnostic performance of the examination. On the other hand, artificial neural networks has been used in nuclear cardiology since the 1990’s6 and have more frequently been taken into use both for research and clinical practice in recent years.7–9
A new deep learning attenuation correction software (DLACS) for MPI was recently introduced for clinical use for the CZT D-SPECT camera (Spectrum Dynamics, Caesarea, Israel). The DLACS algorithm used is based on a computational neural network (CNN) with a U-Net architecture.
The authors have previously reported the performance of the D-SPECT camera comparing the MPI results with invasive coronary angiography (ICA) as the gold standard for diagnosis.8,10 Our previous study using deep learning8 aimed to estimate the prediction of quantitative coronary angiography (QCA) values directly from MPI, however in the current study we investigate whether the novel DLACS would improve the performance of MPI, based on an enlarged clinical cohort.
To the authors knowledge there is not yet any scientific literature evaluating the use of this novel DLACS for the D-SPECT camera to date.
Material and methodsAll adult subjects referred to MPI to our centre between the 1st of September 2014 and the 14th of October 2019 (n = 3634) were retrospectively reviewed. Only patients who underwent ICA within 6 months after the MPI study were considered to be included in the analyses. Subjects with left-bundle branch block, congenital heart disease and cardiac transplantation were excluded. Due to the risk of bronchospasm from regadenoson11 all patients with known asthma or chronic obstructive lung disease were asked to perform a lung spirometry test if a pharmacological stress test (PST) was going to be performed. All patients with forced expiratory volume in 1 s (FEV1) <1 l, patients unable to pedal a bicycle, or low maximum heart rate during previous bicycle stress test (BST) were excluded from the study.
This resulted in the inclusion of 300 patients in the final analyses. None of the patients had cardiac events or myocardial revascularization in the period between the MPI and the coronary angiography examination. The clinical indication for the MPI study was exertional angina and/or dyspnoea.
Stress testStress was induced through BST, pharmacological stress test (PST) or using a combination of the two (CST). The selection of the type of stress test was done at the discretion of a nuclear medicine consultant, mainly dependent of the patient’s ability to pedal a bicycle and the patient’s maximum heart rate from previous BST or during the BST the day of the MPI test. From the 300 patients included for the evaluation 132 underwent BST, 132 PST and 36 a CST.
For the BST group, a standardized maximal bicycle exercise stress test was performed (eBike Basic, GE Medical Systems, GmbH, Freiburg, Germany), with continuous electrocardiographic monitoring (Marquette CASE 8000, GE Medical Systems, Milwaukee, WI, USA). The workload was individually chosen, aiming for a total exercise time of 8–12 min, and started at 30–50 Watts (W), followed by a continuous increase of 15–20 W/min until exhaustion. 99mTc-tetrofosmin was injected to the patient at the highest work load and exercise level, the patient continued to cycle for 1–2 min.
For PST 400 µg (5 ml) of regadenoson were administered i.v. followed by the injection of 99mTc-tetrofosmin 20 s after the administration of regadenoson.
For the combined protocol, a BST with 30–50 W was used along with the injection of regadenoson after two minutes of cycling.
Myocardial perfusion imagingMPI was performed according to the European Association of Nuclear Medicine guidelines.12
Imaging was performed after the stress test using a CZT D-SPECT camera (Spectrum Dynamics, Caesarea, Israel) with at least 1 million myocardial counts for each session. All patients performed the stress MPI in upright and supine positions. In cases of a normal stress MPI, no rest MPI was performed. The patients received 6 MBq × k of 99mTc-tetrofosmin for both stress and rest studies in two separate days, with SPECT acquisitions initiated approximately 30 min after tracer injection. None of the patients had cardiac events between the stress and rest studies.
MPI was routinely assessed visually by two nuclear medicine consultants (each with at least 10 years of experience in MPI) by using the 17-segment model of the left ventricle and a conventional 4-point grading system: 0, normal uptake; 1, equivocal; 2, moderate; and 3, severe reduction of uptake.13–15 Only segments with an uptake score ≥2 at stress were considered to have a definite uptake reduction. Of these, (1) segments with reversible defects (ischaemic defects) were defined as those with a ≥1 point decrease in uptake score on the rest acquisition and (2) the other segments were considered to have a fixed defect (myocardial infarction segments) except for those with a definitely normal contractility on gated SPECT and for which the final diagnosis was attenuation artefact.13,14 Gated SPECT was obtained in stress and rest images. Segments with attenuation artefact were excluded for the final definition of the stress defects area. The evaluation was performed using QPS–QGS, version 2012, Cedars-Sinai Medical Center and the normal databases supplied by the vendor (Spectrum Dynamics). All images without the DLACS were visually analysed in the upright and supine position and all images using DLACS were analysed using the upright position only. As for today, the DLACS supplied by the vendor (TruCorr, Spectrum Dynamics) cannot yet quantify the total perfusion defect (TPD) and this evaluation was therefore not included in this study.
Deep learning attenuation correction softwareThe purpose of the DLACS is to generate an attenuation map from the reconstructed MPI scan without attenuation correction (NC). The attenuation map is then used when reconstructing the MPI scan into an attenuation corrected (AC) image using the standard reconstruction software. The DLACS algorithm used with the D-SPECT in this study is based on a computational neural network (CNN) with U-Net architecture and is described in a previous technical brief.16 The CNN training and external validation by the vendor consisted of the following: The CNN were trained using, as input, hundreds of thousands of SPECT samples (based on 100 patients NC reconstructed stress and rest scans) and, as reference output, attenuation maps extracted from corresponding CT scans. As validation DLACS AC reconstructed stress and rest scans from 25 patients were compared with corresponding CT AC images.
Coronary angiographyICA was routinely performed according to standard techniques. Percent lumen area reductions due to intracoronary atheromatous plaques were first determined visually on end-diastolic frames and with the help of QCA (quantitative coronary angiography) software (General Electric Advantage Workstation, Cardiac X-ray Applications, Stenosis Analysis v1.6) for stenoses that were visually determined to be around the 50% threshold by an experienced angiographer (more than 10 years of experience in ICA) physician (CP). Where applicable, two separate measurements in orthogonal views of the same stenotic segment were obtained and values were averaged to represent an approximate measurement of the percent (%) vessel lumen area stenosis. Any stenosis ≥50% was considered significant and regarded as a positive QCA test. Total coronary vessel occlusions were marked as “100%” lumen area stenosis. When no visible stenotic lumen was seen on angiography with a marginally patent vessel (with other than normal flow) the stenosis was also regarded as a total occlusion as well.
Statistical analysisStatistical analyses, including the calculation of sensitivity, specificity, Positive Predictive Value (PPV), Negative Predictive Value (NPV) and accuracy, were performed using MedCalc statistical software17 and are reported in percentages. Continuous variables were reported as mean ± SD and categorical variables as percentages.
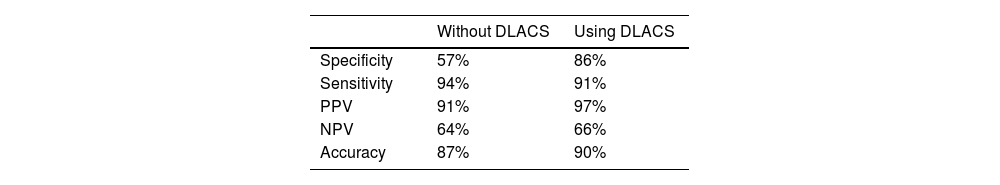
ResultsFrom the 300 evaluated patients, a majority were males 196 (65%) with a mean age of 68 years and a mean body mass index (BMI) of 28,7. The clinical indication for the MPI study was exertional angina and/or dyspnoea in 291 patients and an abnormal exercise test in 9 patients. Mean pre-test probability estimate for CAD, was calculated according to age, sex, angina, and dyspnoea according to the latest ESC guidelines,18 resulting in an average of 37%. 40 patients (13%) had known CAD. Baseline characteristics are included in Table 1.
Baseline characteristics of the study population including all 300 subjects. All data presented as mean (standard deviation) unless otherwise noted.
| Male, n (%) | 196 | 65 |
| Female, n (%) | 104 | 35 |
| Age, yr | 67.7 | 10.2 |
| Weight, kg | 87.8 | 18.5 |
| Height, m | 1.74 | 0,09 |
| BMI, kg/m2 | 27.8 | 5.1 |
| Diabetes mellitus, n (%) | 54 | 18 |
| Hypertension, n (%) | 100 | 33 |
| Hyperlipidemia, n (%) | 51 | 17 |
| Tobacco use, n (%) | 83 | 28 |
| Angina pectorisa, n (%) | 286 | 95 |
| Pre-test probability, % (SD) | 37 | 15 |
BMI, body mass index; SD, standard deviation.
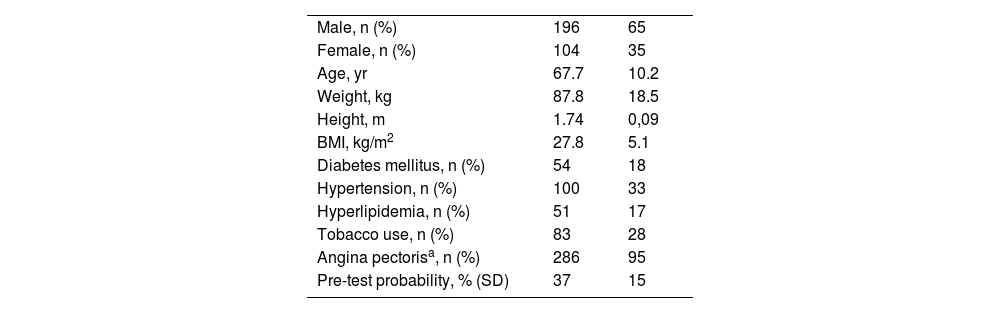
The overall diagnostic accuracy of MPI without DLACS to identify patients with any obstructive CAD at ICA with and without the novel DLACS can be seen in Table 2.
DiscussionWe have retrospectively tested a novel DLACS for MPI in a clinical routine setting and our overall results show a better performance of the population evaluated with the DLACS, mainly due to the reduction of the number of false positive results (FP) in the MPI (Fig. 1), thus increasing the specificity from 57% to 86%. Previously reported specificity rates for MPI using CZT cameras have shown quite modest results ranging from 54% to 76%,1,10 which is mainly due to the high number of FP results obtained with this kind of equipment. In our study, from the 22 cases found with FP results during the evaluation without DLACS, only 7 were found to have FP results using DLACS, something which can be clinically translated into potentially avoiding the ICA procedure in 15 patients.
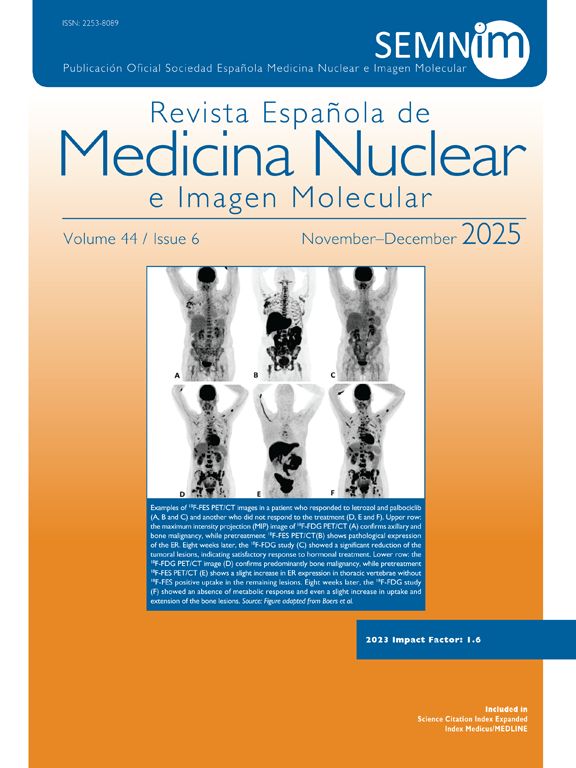
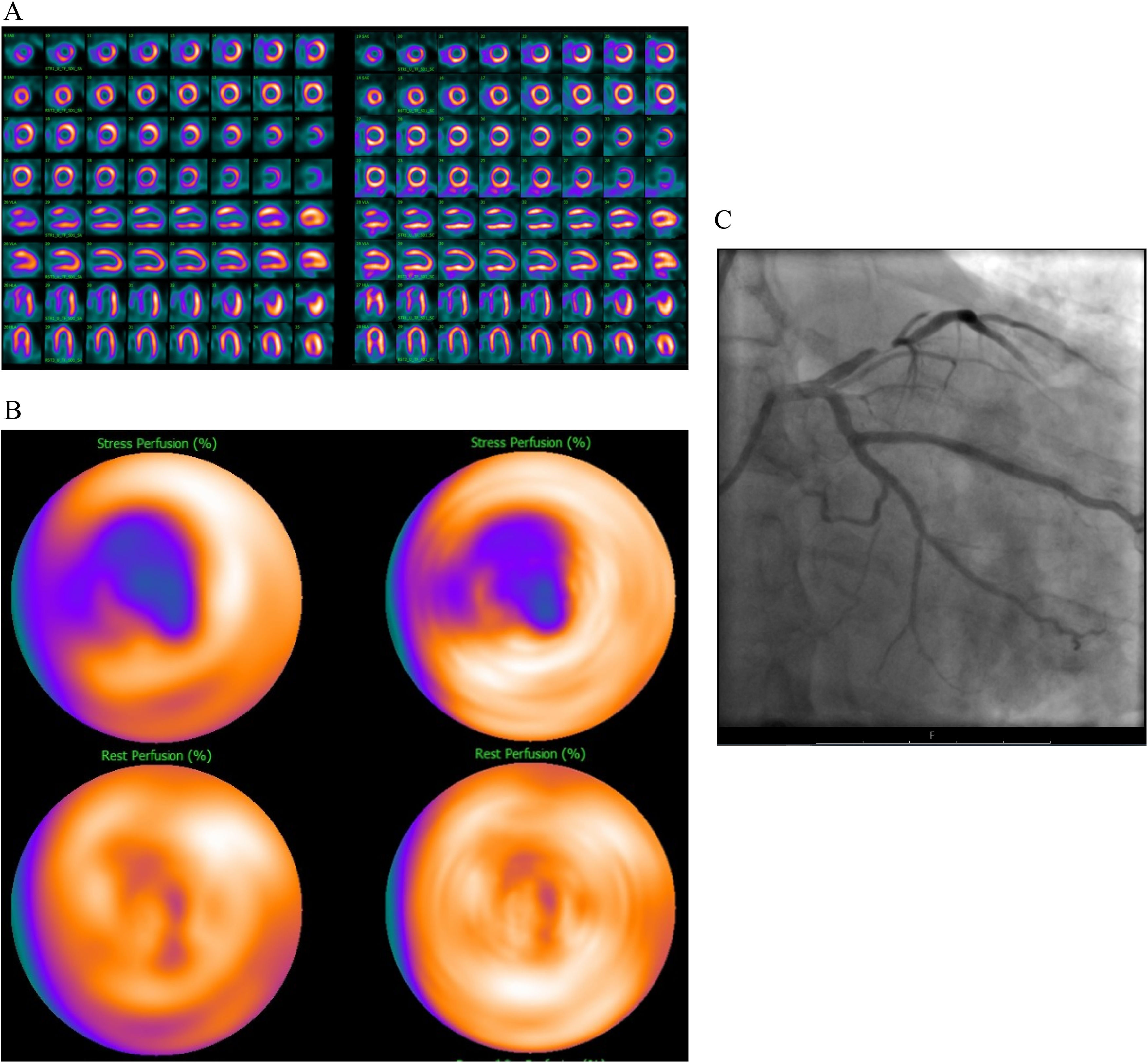
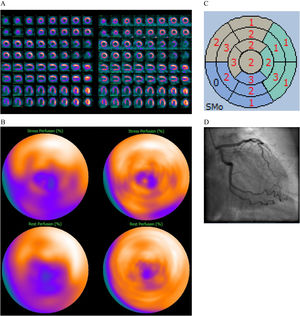
70 year old female, BMI 26, diabetes mellitus type II, smoker, no previous cardiac background known. Apical hypokinesis found during an echocardiography performed as part of a pre-operatory work-up for a recently diagnosed gastric cancer. Referred to MPI to rule out ischemia.
MPI evaluation without DLACS (left images). Splash (A) and bulls-eye MPI (B) stress (upper row) and rest (lower row) in the upright position showing a perfusion defect in the infero-septal wall involving even the apex, showing only partial reversibility at rest. Polar map from gated images during stress showing abnormal contractility of moderate degree (C). No significant obstruction of the coronary arteries at ICA (D). MPI evaluation using DLACS (right images) showing no significant perfusion defects. The patient could have avoided ICA.
Consequently, the sensitivity decreased from 94% without DLACS to 91% when using the DLACS, this was due to an increased number of false negative (FN) results when using DLACS. We found 7 cases with true positive results in MPI confirmed with ICA which turned FN results when evaluated with DLACS (Fig. 2).
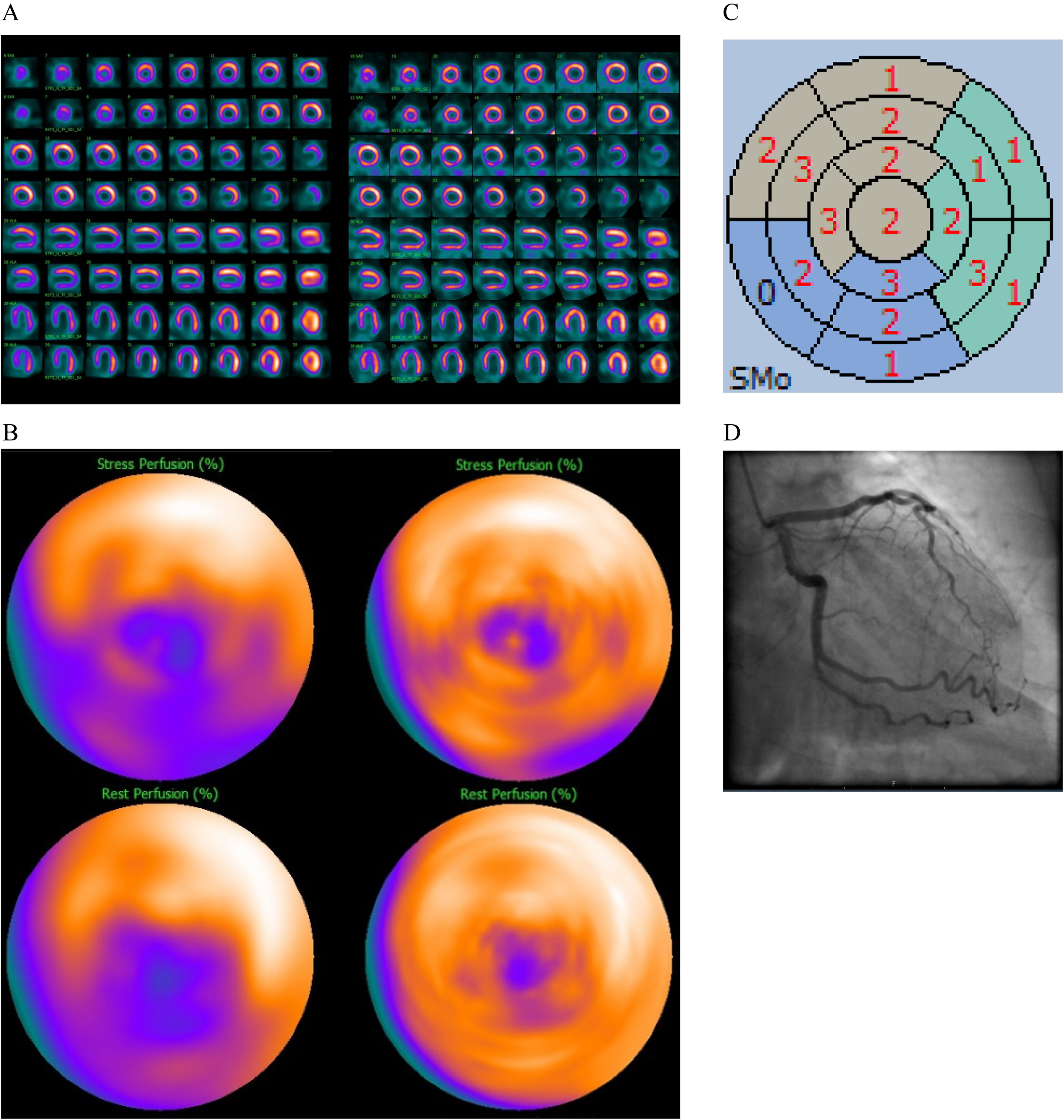
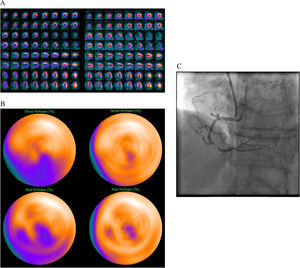
74 year old female, BMI 25, no previous cardiac background known. Pathological electrocardiogram at stress test and angina. Referred to MPI to rule out ischemia.
MPI evaluation without DLACS (left images). Splash (A) and bulls-eye (B) MPI stress (upper row) and rest (lower row) in the upright position showing a perfusion defect in the infero-septal wall, corresponding to the right coronary artery territory, showing partial reversibility at rest. Significant obstruction of the right coronary artery confirmed at ICA (C). MPI evaluation using DLACS (right images) showing no significant perfusion defects. False negative result using DLACS.
Despite that previous research using low-dose CT-attenuation corrected supine position SPECT images has shown promising results in reducing the frequency of attenuation artefacts in MPI4 when using CZT cameras, this approach is time consuming and requires additional ionizing radiation, although low doses, it is always desirable to omit any avoidable radiation in diagnostic imaging adhering to the “as low as reasonable achievable” (ALARA) principles.19
The use of DLACS for MPI could avoid the use of low-dose CT-attenuation, avoiding the use of extra ionizing radiation to the patients, achieving satisfactory sensitivity, specificity and accuracy results in the available scientific literature on the subject to date.20,21
In a recent study, Hagio et al.20 developed a new DLACS using MPI data from a standard Anger SPECT-CT camera with low-energy high-resolution (LEHR) collimators, using a large number of patients from which almost 50% had a body mass index (BMI) >30. The developed DLACS was tested with 351 patients which had ICA correlation, the MPI evaluation was done with quantification of the TPD, their results show a lower diagnostic performance compared to the results of the current study, reporting a sensitivity from 74,4% to 83,8%, a specificity of 66,1%–68,5% and an accuracy of 70.3%–71,5%.
Among the different types of artefacts which have been described in the scientific literature2 to be the cause of FP results in MPI when using the D-SPECT camera, obesity is reported3,10 to be one of the most common causes of artefacts (Fig. 3), something that in a number of instances may lead the patient to ICA. The type of camera and the specific patient characteristics, particularly the large number of patients with high BMI, might in part explain the results obtained by Hagio et al. compared to the results obtained by our group in this study. However, further research is needed to confirm this.
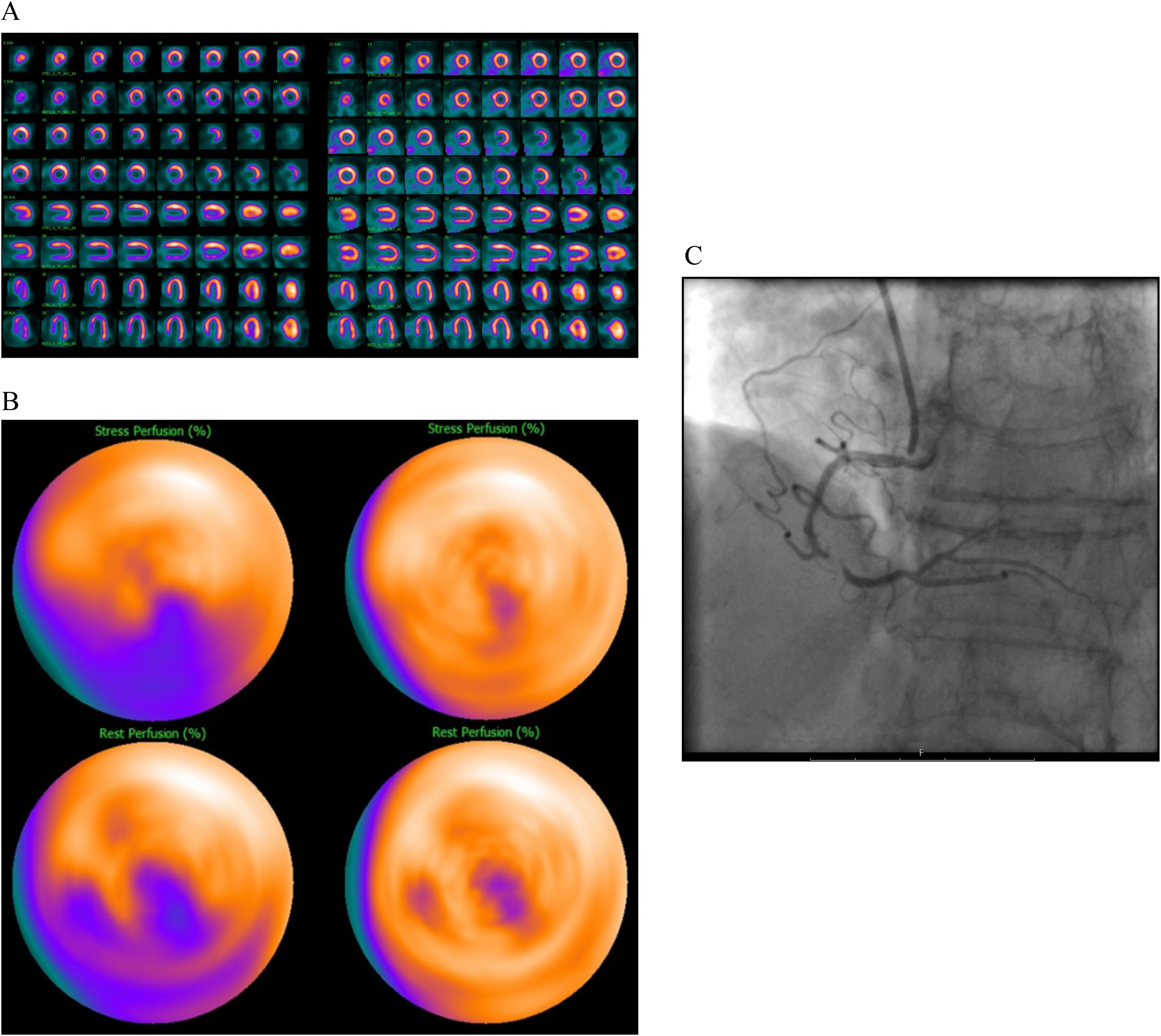
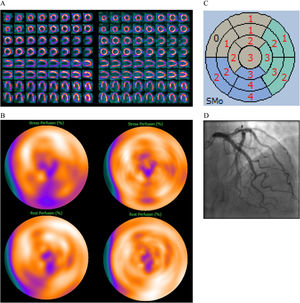
69 year old male, BMI 31, known atrial fibrillation. Pathological ST-T changes in the electrocardiogram at stress test. Referred to MPI to rule out ischemia.
MPI evaluation without DLACS (left images). Splash (A) and bulls-eye MPI (B) stress (upper row) and rest (lower row) in the upright position showing a perfusion defect in the infero-apical wall with reversibility of the inferior wall at rest. Polar map from gated images during stress showing abnormal contractility of moderate degree (C). No significant obstruction of the coronary arteries at ICA (D). MPI evaluation using DLACS (right images) showing no significant perfusion defects. The patient could have avoided ICA.
In our study population we found only 28 patients (9%) with a BMI of 30 or above, the mean BMI for the whole population can be seen in Table 1. From those 28 patients, we found 10 cases with FP results during the visual evaluation without DLACS reducing it to 2 cases during the evaluation using the DLACS (Table 3).
Patients with a BMI >30 and FP results. Evaluation without DLACS and using DLACS. ICA could have potentially been avoided in 8 of the 10 patients evaluated using DLACS.
| Patient | BMI | Without DLACS | Using DLACS |
|---|---|---|---|
| 1 | 31 | FP | TN |
| 2 | 31 | FP | FP |
| 3 | 31 | FP | TN |
| 4 | 32 | FP | TN |
| 5 | 32 | FP | TN |
| 6 | 32 | FP | TN |
| 7 | 33 | FP | FP |
| 8 | 35 | FP | TN |
| 9 | 44 | FP | TN |
| 10 | 52 | FP | TN |
FP, false positive; TN, true negative.
The novel developed DLACS by Hagio et al.20 has been recently tested in a larger multicentre trial,21 using conventional Anger cameras, demonstrating improved results when applying DLACS to the MPI, observing a substantial increase in the specificity and accuracy of the test, something that also was confirmed in our study and can be seen in Table 2.
In a recently published paper by Shanbhag et al.22 the use of DLACS and solid-state cameras with CZT detectors from a different manufacturer compared to our study, showed better performances by MPI when using DLACS. These results are in line with the results by Hagio et al.20,21 and by our group, confirming better accuracy when using these methods.
A limitation of the novel DLACS used in our study was the lack of availability to perform quantification of the TPD and the increase of FN cases, something that could be potentially developed and improved in future versions of the DLACS. Nevertheless, the DLACS shows promising results in the elimination of artefacts in MPI, something which can decrease the number of FP results and potentially increase the specificity of the test, eliminating the need of CT-attenuation correction and extra ionizing radiation to the patient, reassuring the role of MPI as the gatekeeper for ICA (Fig. 4). Another limitation of our study is the low number of cases included. The study population is indeed small compared to the studies of Hagio et al.20,21 and Shanbhag et al.,22 but acceptable when taking into account that this was a single centre study. However, a larger study would have been preferable. Larger, prospective research is warranted to confirm our findings.
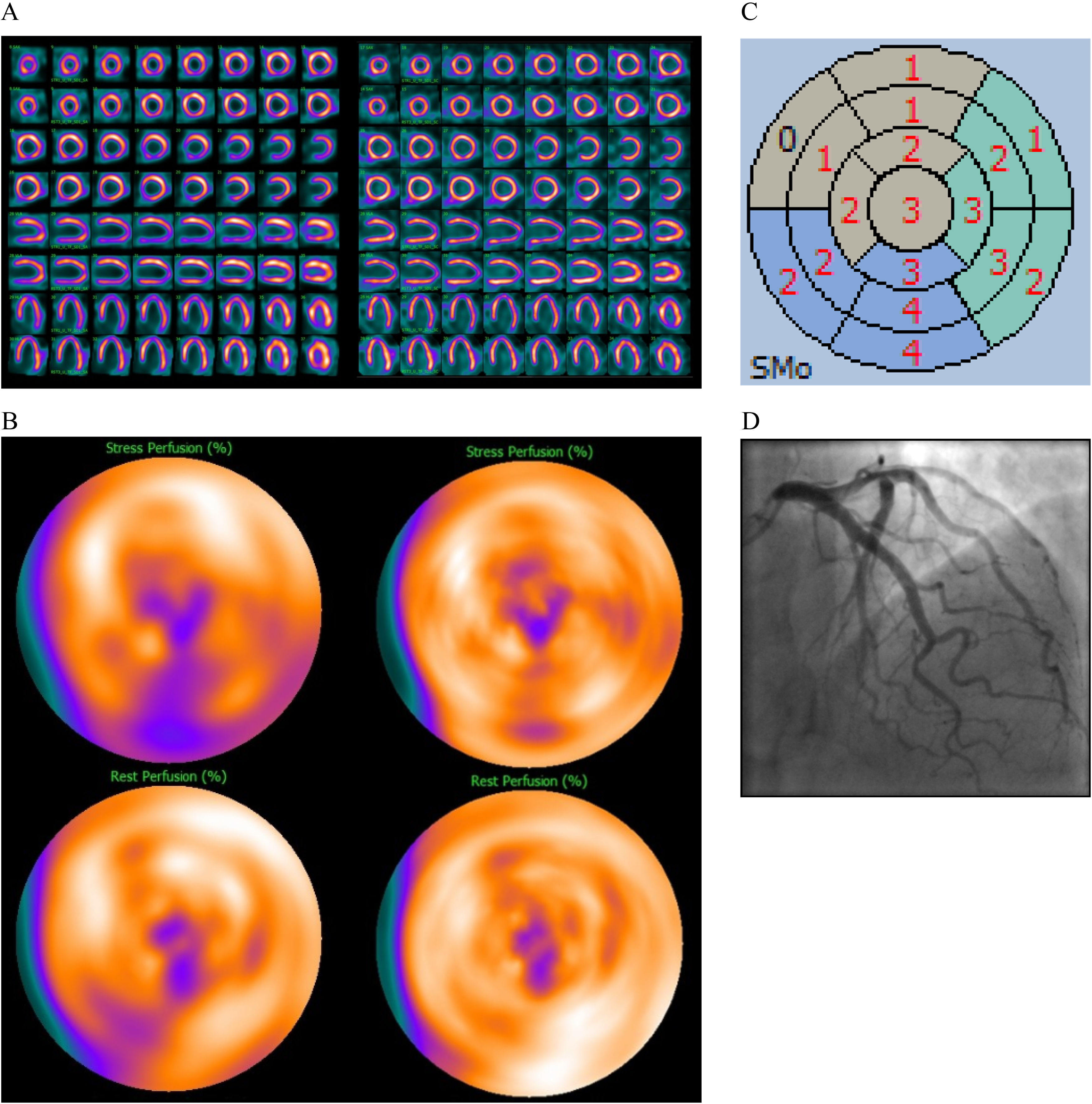
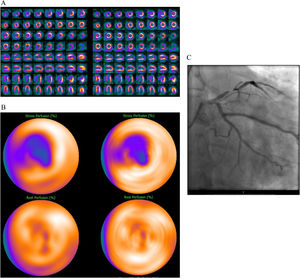
50 year old male, BMI 29, hypertension, hyperlipidaemia and typical angina. Referred to MPI to rule out ischemia.
MPI evaluation without DLACS (left images). Splash (A) and bulls-eye MPI (B) stress (upper row) and rest (lower row) in the upright position showing a perfusion defect in the anterior wall with reversibility at rest. Significant obstruction of the left anterior descending artery confirmed at ICA (C). MPI evaluation using DLACS (right images) showing a perfusion defect in the anterior wall with reversibility at rest. True positive case both with and without DLACS, confirmed at ICA.
The DLACS increases the performance of the MPI using the CZT D-SPECT camera achieving improved results, especially in avoiding artefacts and therefore reducing the number of FP results, following the ALARA principles in the best possible way, avoiding the need to use ionized radiation for attenuation correction.
FundingGrant support was obtained by Henry och Ella Margareta Stahls Stiftelse (Henry and Ella Margareta Stahl's Foundation, project RÖ-981845), Analytic Imaging Diagnostics Arena (Vinnova grant 2017-02447), Department of Department of Clinical Physiology and Department of Radiology, Region Östergötland.
Conflict of interestThe authors have no conflicts of interest to declare.