Standard pre-operative coagulation tests are insensitive to certain haemostatic abnormalities, yet they continue to be ordered routinely. Given the lack of clear guidance in Spain, we used Delphi methodology to develop a series of consensus recommendations on ordering these tests.
Material and methodsWe conducted a 3-round, online, multicentre Delphi study in which 10 expert anaesthesiologists were asked to recruit colleagues to form a panel of 59 anaesthesiologists, 50 of which completed all rounds. The panel rated 46 statements on a 1–9 Likert scale. Consensus was achieved when ≥70% of questions scored ≥7 in the third round. Accepted statements were classified as Weak (70%–79%), Moderate (80%–89%) or Strong (90%–100%) agreement.
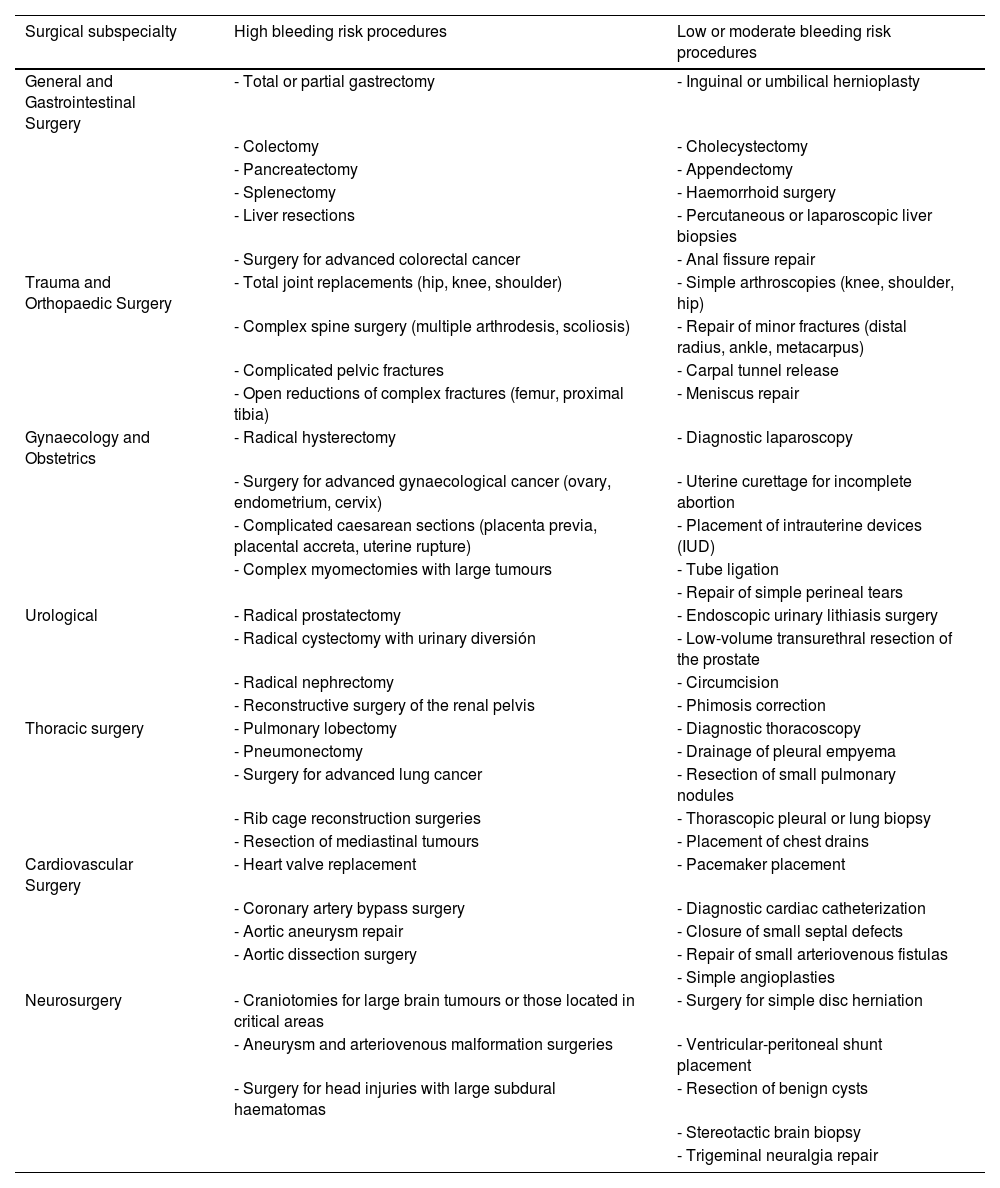
ResultsTwenty-nine statements were accepted. These were synthesized into 21 statements that were grouped into 6 categories: general indication, patient risk factors, procedure characteristics, global assessment, paediatric patients, and special cases. Agreement was strong for 14 statements, moderate for 5, and weak for 2. Key recommendations were: (1) avoid universal testing; (2) base testing on medical history, standard bleeding-risk questionnaires, and specific risk factors (anticoagulation, liver disease, kidney failure, haematopoietic disorders); (3) order tests before high-complexity or high-bleeding-risk procedures; and (4) use specific tests in patients receiving direct oral anticoagulants.
ConclusionsPre-operative coagulation testing is indicated in patients that present bleeding disorders and/or are scheduled for a high-bleeding-risk procedure.
Las pruebas estándar de coagulación preoperatorias han mostrado escasa capacidad para detectar alteraciones hemostásicas, pero se siguen solicitando de forma rutinaria. En nuestro entorno no hay recomendaciones claras al respecto. The objective of this study was to develop a consensus on its indication using the Delphi methodology.
Material y métodosSe realizó un estudio Delphi multicéntrico on-line de tres rondas. Diez anestesiólogos expertos reclutaron colaboradores hasta completar el grupo de trabajo (59 anestesiólogos); completaron el proceso 50. El panel valoró 46 afirmaciones con una escala Likert 9. Se alcanzó consenso cuando, en la tercera ronda, ≥ 70% de las puntuaciones de cada afirmación fueron ≥ 7. Las afirmaciones aceptadas se calificaron como acuerdo Leve (70–79%), Moderado (80–89%) o Fuerte (90–100%).
ResultadosSe aceptaron 29 afirmaciones, resumidas en 21 y agrupadas en seis categorías: indicación general, factores de riesgo del paciente, características del procedimiento, valoración global, pacientes pediátricos y casos especiales. Agreement was strong on 14 statements, moderate on 5, and minor on 2. Recomendaciones principales: 1) no solicitar pruebas de forma universal; 2) decidir su necesidad según historia clínica, cuestionarios estandarizados y factores de riesgo (anticoagulación, hepatopatía, insuficiencia renal, trastornos hematopoyéticos); 3) indicarlas antes de procedimientos de alta complejidad o riesgo hemorrágico; 4) usar pruebas específicas en pacientes con anticoagulantes directos.
ConclusionesLas pruebas de coagulación preoperatorias deben individualizarse en función del riesgo de alteraciones hemostásicas del paciente y del riesgo de sangrado del procedimiento.