The large number of abdominal X-ray examinations done in the emergency department is striking considering the scant diagnostic yield of this imaging test in urgent disease. Most of these examinations have normal or nonspecific findings, bringing into question the appropriateness of these examinations. Abdominal X-ray examinations are usually considered a routine procedure or even a “defensive” screening tool, whose real usefulness is unknown. For more than 30 years, the scientific literature has been recommending a reduction in both the number of examinations and the number of projections obtained in each examination to reduce the dose of radiation, unnecessary inconvenience for patients, and costs.
Radiologists and clinicians need to know the important limitations of abdominal X-rays in the diagnostic management of acute abdomen and restrict the use of this technique accordingly. This requires the correct clinical selection of patients that can benefit from this examination, which would allow better use of alternative techniques with better diagnostic yield, such as ultrasonography or computed tomography.
La escasa rentabilidad diagnóstica de la radiografía de abdomen en patología urgente contrasta con el elevado número de exploraciones que se realizan. La mayoría arroja hallazgos normales o inespecíficos, lo que cuestiona la idoneidad de su indicación. Suele considerarse un procedimiento rutinario o incluso una herramienta “defensiva”de cribado, cuya utilidad real se desconoce. Desde hace más de 30 años, se recomienda en la literatura científica reducir tanto el número de exploraciones como el de proyecciones realizadas, en aras a disminuir dosis de radiación, molestias innecesarias para los pacientes y costes.
Radiólogos y clínicos deben conocer las importantes limitaciones de la radiografía de abdomen en el manejo diagnóstico de la patología abdominal aguda y restringir su empleo. Para ello, es imprescindible una adecuada selección clínica de los pacientes candidatos a estudio de imagen, que permite un empleo ágil de técnicas alternativas más rentables como la ecografía o la tomografía computarizada.
The evaluation of a healthcare technology is a complex task whose objective is to balance the actual benefits for the patient and the possible risks, disadvantages and costs derived from its implementation. The radiological setting includes five levels referring progressively to technical quality, diagnostic yield, diagnostic and therapeutic impact and health progression.1 Parameters such as image resolution are useful to evaluate the first level while sensitivity and specificity or predictive value are useful to evaluate the second being relatively easy up to this point to verify progression with respect to the previous standard. Making progress in the evaluation process is extremely difficult especially in techniques consolidated by use, for which there are no defined evaluation guidelines and where scientific evidence can be of low quality or non-existent. In practice it is assumed that an examination is useful when the result modifies clinical management, to confirm or rule out a diagnostic choice or else to stage the risk of a potentially serious situation.2 When radiology is used routinely as a “rubber stamp” to be stamped on every patient1 it is difficult to prove its effectiveness, since there is no previous clinical question to answer. Also an examination that does not contribute any information can only contribute confusion (e.g., incidental or unspecific findings).3 The following pages are intended to show how abdominal radiography (AR) in the emergency setting is an example in the negative way of all the above: an imaging modality consolidated by use of whose clinical usefulness there is little scientific evidence–or if there is any evidence there is negative evidence–in spite of which it maintains a long list of possible clinical applications that everyday reality surpasses broadly making it a routine for every patient that goes to the emergency services (ES) with abdominal symptomatology regardless of its characteristics and the degree of severity. Radiologists and clinicians alike need to know the important limitations of AR to detect acute pathologies with the promptness and precision of other image modalities basically ultrasounds and computed tomographies (CT). They must resort to the latter regardless of the AR result when the clinical context suggests a serious pathology. In mild cases, the remote probability of positive findings also advises against the use of AR.
Diagnostic approach to patients with acute abdominal symptomatologyPain is the most constant clinical manifestation of acute abdomen condition and a common cause for going to the ES in adults.4–6 The medical history, the physical examination and lab tests are the starting point of its clinical study and usually enough in mild cases. In the remaining cases although they can give clues about the nature and location of the causal process they often yield unspecific results that need to be completed with image tests.5 Such tests should provide ideally either in positive or negative significant information for the therapeutic decision. A positive result establishes a diagnosis (e.g., intestinal obstruction [IO]), or its etiology (e.g., peritoneal adhesion) and location (e.g., distal ileum), and it even allows us to stage its severity (e.g., closed-loop obstruction with signs of intestinal ischemia). A reliable negative result promotes an early discharge from the ES avoiding admissions and unnecessary expenses. When correctly indicated and performed timely a decisive image examination improves diagnostic accuracy, promotes surgical indication, planning and approach, speeds up the discharge or admission decision-making process, reduces hospital stays, improves service quality and diminishes morbimortality.7,8 On the contrary image modalities add little value, or even subtract value, in patients with mild symptomatology, candidates to clinical management2,5 or when the modality selected is not the right one–situations that only increase the dose of radiation, the time spent in the ER and the patient's discomfort and healthcare costs.5
Acute abdominal pain can be associated to a variable degree of severity and be due to multiple causes.5 Apendicitis, IO, diverticulitis, cholecystitis, renal colic, acute intestinal pathology–including ischemia and perforation–pancreatitis or gynecological disorders are diagnoses that need to be taken into consideration whose frequency varies in the different publications and epidemiological profiles. Although one in 3 patients who go to the ER due to abdominal pain is discharged without identifying any causes,3,4,7,9 expediting those discharges requires decisive image modalities (Fig. 1). The diagnostic management of acute abdomen differs from one country to another with two major trends, early use of CT or clinical examination complemented with simple radiography and ultrasound with CT on demand.7–10 Although the former option seems to improve diagnostic accuracy, prospective studies have not shown any significant differences in other measures.10 Most clinical guidelines indicate image studies depend on the location of the pain, being the ultrasound the 1st choice for the right upper quadrant and the pelvis, and CT for the remaining quadrants. Laméris et al.7 attain maximum sensitivity with a minimal radiation dose beginning by AR followed by ultrasound and CT in uncertain cases.
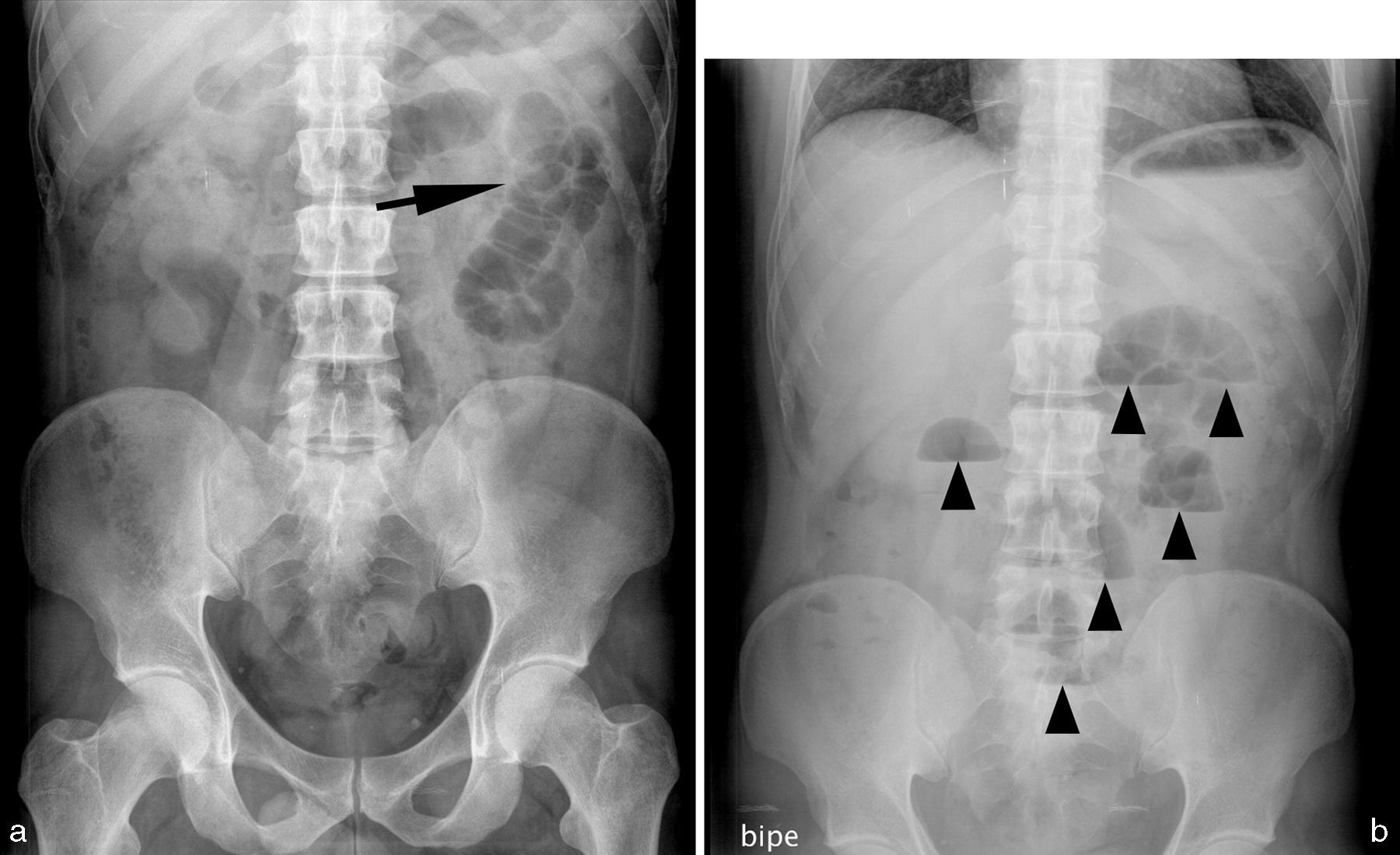
Thirty-seven (37) year old male presenting with abdominal pain and impaired intestinal rhythm with reduced gas fecal emission. (a) Abdominal radiography (AR) in decubitus supine position showing a pattern of anodyne gas with a slightly dilated small intestine loop in the left superior quadrant/flank (arrow). (b) The AR in bipedalism shows multiple hydroaerial levels (arrow heads) with very few gas in the colon indicative of small intestine occlusion. A CT was performed (not shown) giving normal results. After 24h the clinical condition resolved spontaneously.
The low diagnostic yield of AR2 has been recognized since the 1960s yet despite this its systematic use is recommended in patients with acute abdomen pain.11 In 1982, Eisenberg et al.12 suggested restricting AR to patients with moderate or serious abdominal pain and in cases of clinical suspicion of IO, urethral calculi, ischemia or vesicular pathology. With this approach, they eliminate 53.7% of the examinations, without any clinical repercussions. Many subsequent studies have proven the absence of scientific basis for performing AR to all patients with abdominal symptomatology2,5,9,13–20 –a usual practice in the ES even today when the availability of other more refined modalities such as ultrasound and CT is practically universal. There is no direct information available about the use of AR in patients that go to the ER due to abdominal pain. In most published series ARs are performed in more than half of these patients regardless of the characteristics or the intensity of the pain,14,21 surpassing 90% in some.15 These are some of the factors that promote the unjustified use of AR: the consideration the “routine examination” in the ER, the lack of control of the simple X-ray by the radiologist and the electronic request systems along with training deficits among new physicians and the resistance of “senior” physicians to change their traditional practices.15,18,20
During the last few years the most important radiological societies around have been continually reducing the lists of indications for AR included in their recommendations.22–24 In its 2011 revision the American College of Radiology (ACR)23 eliminates abdominal pain as an indication for AR. With a more practical approach in their Diagnostic Imaging Pathways24 the Royal Australian and New Zealand College of Radiologists recommend performing ARs only in cases of suspicion of perforation or IO, ingestion of a foreign body, unspecific moderate or serious abdominal pain and follow-up of calculi in the urinary tract. Nevertheless even these indications are being revised today.
Different publications place the ideal rate of AR use due to acute abdominal pain below 10%.2,21 Implementing the previous unrestrictive recommendations most authors agree that the number of ARs performed could be reduced by 50–70%, or even in larger percentages.5,9,15,17,21,25 Logically, the diagnostic yield of AR is incidental in the group of patients where there is no indication.2,9,15
The “abdominal series”. Necessary projectionsAR in supine position must include from the thoracic diaphragm to the obturator foramen, occasionally needing two exposures. This is the basic projection, the starting point of the so-called “abdominal series” that also includes another projection “with a horizontal beam” in bipedalism or lateral decubitus position and a chest X-ray in bipedalism.23,26 The latter, performed as part of an abdominal series, contributes useful information in 10–15% of the cases, about the thoracic pathology (pneumonia, pericarditis) causing abdominal symptomatology or thoracic manifestations of an abdominal process (pleural effusion in pancreatitis or abdominal infection). It can detect small quantities of intraperitoneal gas better than AR in bipedalism. It is recommended to maintain bipedalism or the lateral decubitus position for at least 10min before obtaining the X-ray exposure to let the gas rise above the liver dome.26
Mirvis et al.27 opposed the use of AR in bipedalism in 1986 because it rises costs and contributes little useful information. The AR in the decubitus prone position favors the displacement of the gas in the transverse colon toward its ascending and descending segments. Performing it is difficult in seriously ill patients where the only alternative is often laterolateral projections of the abdomen in the supine position with a horizontal beam, tangential to the anterior wall for the detection of underlying gas. Today the generalized opinion is to consider the “abdominal series” as superfluous whose dose of radiation and costs are similar to or surpass those of low-dose CT with much less information.2
Arguments against the use of abdomen X-ray in the emergency roomThe validity and reliability of AR are very low in the assessment of abdominal pathology; therefore errors are frequent, especially in the emergency setting.9 That is why its findings must be interpreted with caution always within the patient's clinical context and based on its accuracy. In the studies published, the validity of AR in patients with acute abdominal pain is not usually expressed through the usual parameters of sensitivity, specificity and predictive value due to the absence of adequate reference standards in many studies2 and to the multiplicity of signs and etiological options making it impossible to set up the usual contingency tables 2×2. Most often, its diagnostic usefulness is expressed in terms of positive findings, change of diagnosis or clinical management of patients or degree in which the image modality proves to be of diagnostic utility for the ER physician. When it comes to reliability, Markus et al.28 studied interobserver variability in the interpretation of AR by different radiologists and they found an adequate concordance in the identification of pneumobilia, renal lithiasis or pneumoperitoneum, and worse results in the detection of small intestine obstruction, cholelithiasis, colitis, thumbprinting, dilatated intestinal loops, pathological hydroair levels, normal gas pattern or masses. The worst results were for the assessment of colon obstruction, unspecific gas patterns, complete obstruction of the small intestine, location of the obstruction site in the small intestine, diffused/located ileum, ascites and urethral lithiasis. The correlation was low to determine partial or complete obstruction of the small intestine and its proximal, medial or distal location.
With important variations based on the sign or pathology being considered the diagnostic yield of AR is around 10%2,5,17–19,21,29,30 and though some authors rise the percentage of relevant findings to 15.8%,14 others do not find any significant impacts of AR in the clinical decision-making process.16 Such yield should improve with the level of adhesion to clinical recommendations that is usually. Morris-Stiff et al.15 in their series find that 32% of requests abide by the standards of the Royal College of Radiologists (RCR) with positive results for this group of around 76.7% as opposed to 3.3% for patients with inadequate requests. Feyler et al.18 say that 12% of requests abide by the RCR guidelines with an impact of their findings on clinical management in 7% of the cases. The usefulness of AR is zero in cases of unspecific abdominal pain, acute digestive hemorrhage, peptic ulcer, apendicitis, urinary tract infection, pelvic pain, biliary pathology, acute pancreatitis or uncomplicated constipation, among others.2,13,16,19,21
The AR detects alterations with low sensitivity (Figs. 2 and 3) but even when it does it rarely exhausts the diagnostic process on its own. In most publications, the change of clinical management for patients induced by the AR is below 10%.21 Kellow et al.16 find that with the exception of the location of abdominal catheters, the AR is not very useful in acute abdomen conditions and only 3% of their patients were treated based on the AR findings. They conclude that in general the AR does not avoid other image modalities, as it happened in 59% of their patients to outline the extent of the alteration, identify its etiology, plan treatment or have a basal image to evaluate therapeutic response. This is to say that a pathologic AR does not provide any conclusive diagnoses in most patients but even when it does it needs other additional image modalities (Figs. 4 and 5).
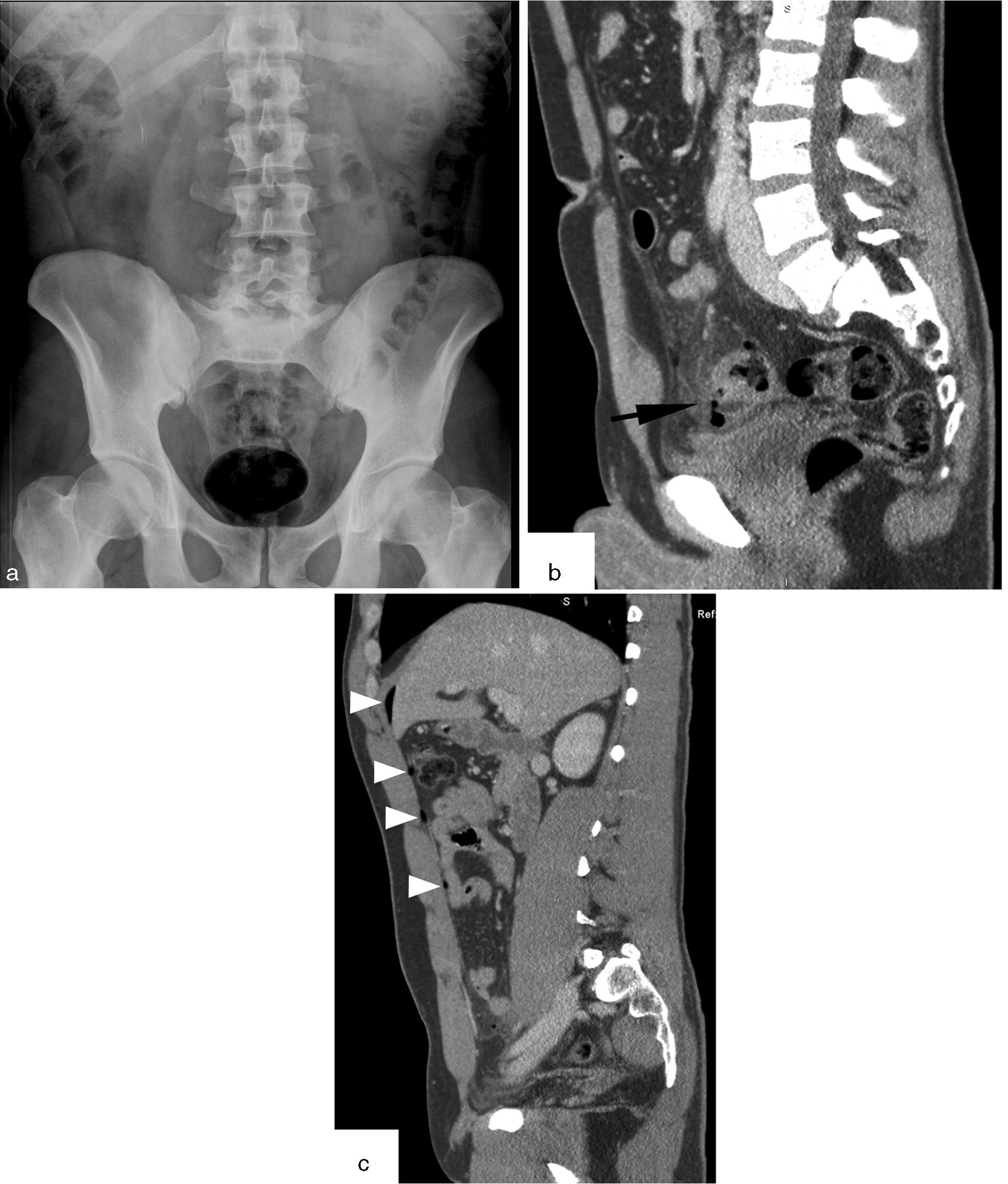
Thirty-four (34) year old male with pain in the lower semi-abdomen, fever and leukocytosis. (a) The AR of the abdomen in the decubitus supine position shows no significant alterations. (b and c) CT parasagittal images. Wall thickening of sigmoid colon with diverticula and perforation of one of these diverticula (arrow in b) with presence of extraluminal gas and signs of adjacent fat inflammation. Multiple bubbles of intraperitoneal gas of anterior location (arrow-heads in c). Perforated diverticulitis.
Seventy-two (72) year old woman with abdominal pain of sudden onset. The clinical exploration shows signs of shock and arrhythmia and in the analysis acidosis and hyperamylasemia. (a) AR with no significant findings. (b) CT coronal image in 6mm maximal intensity projection showing a lumen repletion defect of the superior mesenteric artery compatible with an embolism (arrow). Cardiomegaly (*).
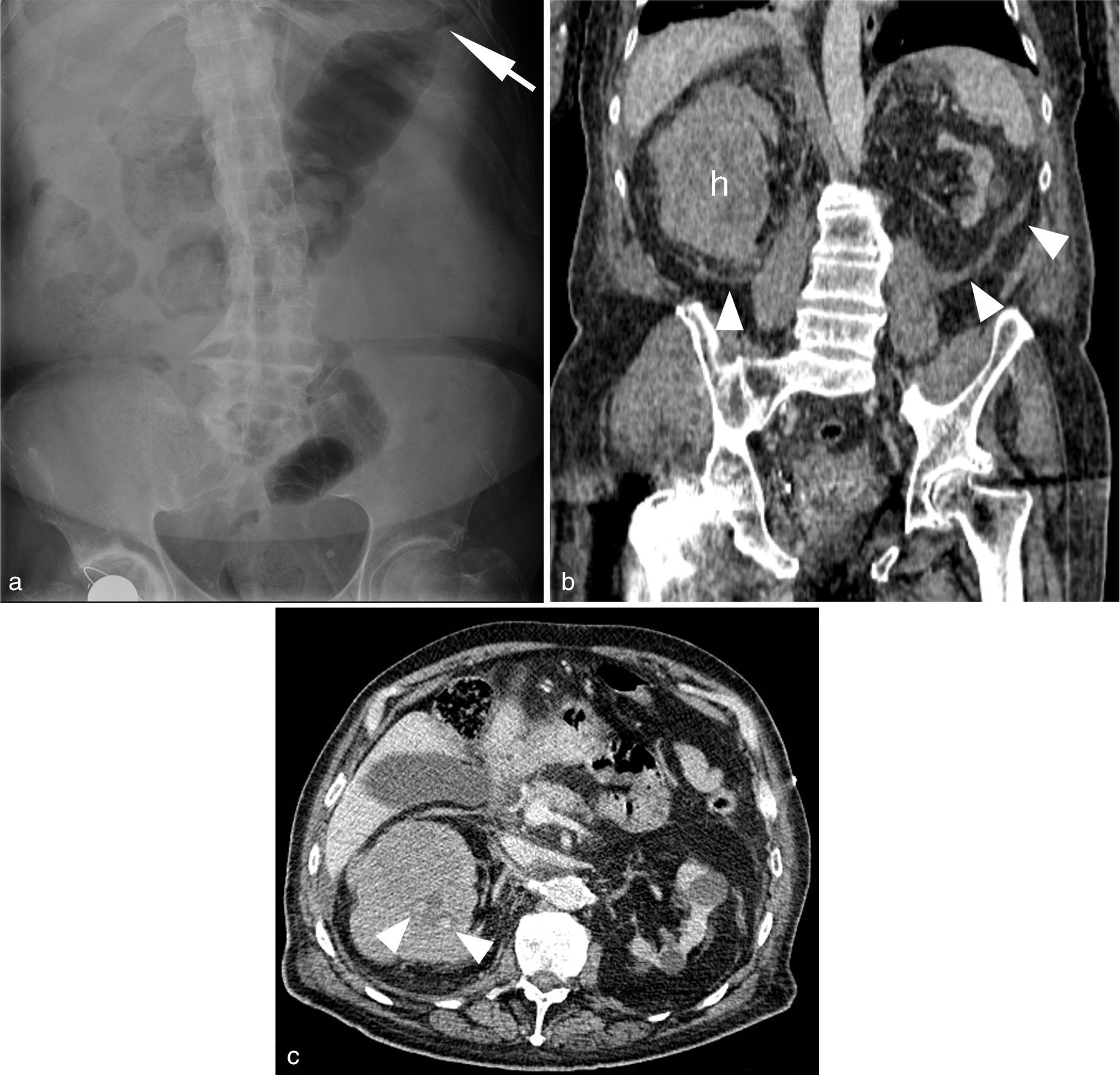
Eighty-two (82) year old male with a history of chronic renal failure (serum creatinine levels: 6mg/dl) and a right hip prosthesis. Oral anticoagulation with a INR (International Normalized Ratio)>5. He goes to the hospital with acute abdominal pain radiated to his back with distention. Anemia and thrombocytopenia. (c) AR in the decubitus supine position showing signs of chronic spondylitis and scoliosis with abundant fecal content that prevents us from performing an adequate assessment of the visceral structures. Colon caliber-reduction at splenic flexure level simulating a “colon cut-off sign” (arrow). Initially a study through computed tomography (CT) without contrast (b) is performed. The coronal multiplanar reconstruction (MPR) shows non-obstructive left renal atrophy and an enlarged unstructured left kidney with heterogeneous attenuation secondary to non-traumatic renal hematoma (h). Wunderlich syndrome. No causal lesion can be identified. Then an axial cut of the CT-angiography (c) is performed and two (2) small foci of active bleeding (arrow-heads) can be identified and visible in the venous phase only. The patient remained stable with conservative treatment and correction of his coagulopathy.
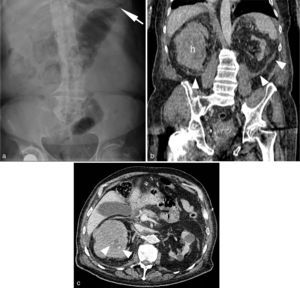
Fifty-six (56) year-old woman at the emergency room presenting with diffuse abdominal pain and no gas or fecal expulsion. During the examination she shows poor health with the presence of tachycardia and hypotension, abdominal silence and “loop mass” palpation. The AR (a) does not show any significant findings with the exception of flexure thickening in a jejunal loop located at the left superior quadrant (arrow). (b) Computed tomography (axial view) in portal stage (70sg) of the middle abdomen region showing jejunal loop distention with no wall enhancement due to hypoperfusion (*) [compare it with the adjacent duodenum (d)]. Perihepatic intraperitoneal liquid in between the loops (arrow-heads). Surgery confirmed the diagnosis of intestinal obstruction caused by bridles complicated with strangulation; 55cm of necrotic small intestine were resected.
Incidental findings are especially frequent when an incorrect indication is the starting point. Its assessment can provide a wrong or inadequate clinical response diverting the management of the patient to research lines or guidelines of clinical management that are far from their actual problem, with diagnostic delays or inadequate treatments and greater morbimortality. The percentage of wrong findings for AR in some papers has been established around 19%21 and in others it has managed to surpass the useful information in a 3:2 ratio.30
Ruling out a prevailing or especially serious condition expedites the work of the ES while contributing to early discharge being one of the most decisive current applications of diagnostic image modalities. This is not the case of AR–a not very useful modality for the identification of unsuspected diagnoses.26 Yet despite this fact its use is frequent as a normal screening tool. Stower et al.31 found that 60.8% of the ARs requested in their series were meant to rule out a serious condition. This practice causes unnecessary inconveniences to the patient, it is potentially dangerous and should not be recommended. It is well known that a normal x-ray does not allow guarantee normality or precludes a serious condition21 (Figs. 2 and 3). Seventy-two per cent the patients with normal AR in the Kellow et al. paper16 presented some alteration when other image modalities were used; this is why they do not recommend its use to rule out abdominal conditions. Almost half (46%) of the cases presented unspecific findings in the AR, and in 78% of them alterations could be later identified. Simeone et al.32 discover useful information through ultrasound predominantly of biliary origin in 20% of the patients with abdominal pain and a negative AR.
The dose of radiation administered is another issue that should be considered when evaluating medical image modalities. Every exposure to ionizing radiation needs to be justified by a potential benefit and though the dose of one AR is not very high for an individual examination (0.7–1.3mSv), 40 times that of a chest X-ray or 4 months of background radiation,33 it gains relevance from a population approach, above all taking into account the probability of additional projections.25,34,35 Radiation derived from conventional radiographies has declined during the last few years35 though the AR is still one of the four most common indications in this group.36 It is responsible for 2.93% of the radiological procedures performed in the UK, and for 4.42% of the total dose.37 The progressive accessibility from the ER to low-dose and ultralow-dose CT modalities <4 and 2mSv will probably displace the use of AR in favor of these modalities.34
The economic cost is another evaluation argument, and although the AR is a relatively inexpensive modality–around 30–40 € the reduction of unnecessary examinations along with other direct costs such as technician and radiologist time or indirect costs, such as a previous pregnancy tests in young patients amount to yearly savings of around 50–60 million pounds in the UK.15,25
AR in the usual causes of abdominal pain. Does anything change?Intestinal obstructionAround 7% of patients with acute abdominal pain will have IO.5 Clinical evaluation has limitations in its assessment but it provides information (abdominal distension, increase of intestinal noise, vomiting, age>50 years) which improves the sensitivity and the predictive value of AR when diagnosing IO (intestinal obstruction).5,14,19 Its most frequent etiology is peritoneal adhesions and hernias, and an early diagnosis and treatment prevent intestinal ischemia, improving morbimortality. The IO has been one of the classic indications for AR which is diagnostic in 50–60% of the cases, uncertain in 20–30% and confusing in 10–20%.38 The sensitivity of AR to diagnose IO ranges from 46% to 90.8% in the different series, with a specificity close to 50%. It has important limitations when it comes to determining the level and cause of the obstruction as well as the presence of strangulation.5,39 Today the MSCT (multi-slice computed tomography) answers all questions with sensitivity and specificity close to 100%,7 and it is the initial test of choice in cases of suspicion of IO as recognized by the ACR guidelines. Also this approach is useful for cases of colon obstruction, where the AR can be confusing or inconclusive and delay treatment. Not only does the CT perform a more precise diagnosis but it also provides additional information that can modify treatment in one out of every five cases40 (Fig. 5).
Hollow viscus perforationThere is no scientific evidence supporting the use of AR in cases of suspicion of visceral perforation.2 Although in ideal conditions it can be detected through an X-ray using a minimum of 1 cc of free intraperitoneal gas41 reality can paint a different picture as shown by the high variability in the figures of detection of pneumoperitoneum among the different papers and radiographic projections used. van Randen et al.13 estimate in around 15% the sensitivity of AR to detect pneumoperitoneum; in the Baker et al. series42 X-rays detected it in 51% of the patients with proven visceral perforation, and Levine et al.43 identify it in 59% of ARs performed in the decubitus supine position, while Keefe et al.44 identify it in 83% - number that goes up to 85% when using chest radiographies and to 96% with ARs performed in the left lateral decubitus position and that goes down to 60% and 56% with ARs performed in bipedalism and in the decubitus supine position, respectively.45 Other papers do not find any differences in the positive predictive value of the clinical examination for pneumoperitoneum after performing ARs.13 This low diagnostic yield, inherent to the typical limitations of X-rays grows worse when its technical quality is deficient, due to incomplete anatomical coverage or exposure.42 There are diverging opinions46 but MSCT is at present the test of choice to identify the presence, location and etiology of intestinal perforation, which is relevant information for an adequate surgical approach47–50 (Fig. 2).
Renal colicWhen the clinical context is typical and in the presence of hematuria the image modalities do not modify therapeutic management in the absence of fever, durable pain or diagnostic uncertainty. Nevertheless the great majority of existing clinical guidelines and recommendations indicate the immediate performance of an imaging test.51 Such test should confirm the presence of urethral calculi and provide information about its location, size and composition, as well as the presence of urethral obstruction. In the absence of lithiasis, it should identify alternative diagnoses such as complicated aorta aneurism.9 The sensitivity of the AR ranges from 44% to 77% in the different works published being the specificity between 71% and 87%, and MSCT is the usual standard of care.5,51,52 When image tests are indicated the ultrasound usually comes first in young patients yet the CT identifies the practical totality of lithiases53 and provides the required additional information.5 The indication for AR would be limited to the follow-up of urethral lithiasis diagnosed through CT or ultrasound.2
Acute appendicitisARs are performed on 50–75% of patients with suspicion of acute clinical apendicitis,54 despite the existing scientific evidence that does not recommend it.2 A conclusive clinical diagnosis does not require confirmation through imaging modalities,2,19 and in uncertain cases, the diagnostic yield of ultrasound and CT is way much higher.55 Ultrasound is the initial method of choice, especially in children and women in their fertile age; the MRI is an alternative in pregnant women with inconclusive ultrasounds.
Diverticulitis, pancreatitis and acute cholecystitisAcute diverticulitis does not associate useful semiology in AR this is why it does not have any indications. When it is necessary to confirm the diagnosis and detect possible complications CT is used. Beyond the presence of a “sentinel loop” or a “colon cut-off sign” that may be indicative of diagnosis of acute pancreatitis the AR does not present specific findings of this clinical entity so its use is not indicated. The latest review of the Atlanta guidelines56 does not recommend the use of image modalities including CT, during the first week, except for cases of uncertain clinical-biochemical diagnosis or to rule out alternatives such as intestinal perforation or mesenteric thrombosis. The AR is not indicated either as the initial diagnostic modality in cases of acute biliary pathology where the ultrasound is the modality of choice when suspicion of uncomplicated acute cholecystitis.4
Intestinal ischemiaIdentifying gas on the intestinal wall or the portal branches through the AR, classically considered a pathognomonic sign of mesenteric ischemia, is an infrequent finding that at least denotes advanced disease.26 The growing use of abdominal CT has allowed the visualization of portal gas in more “benign” situations but its detection through X-ray associates a high risk of ischemia and a 75% mortality, and this is why immediate laparotomy is recommended even in the absence of clinical signs.57 Nevertheless an AR can be normal even in the presence of extensive intestinal ischemia26 (Fig. 3).
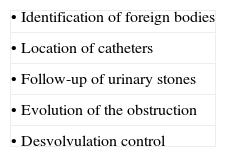
Foreign bodies. Intra-abdominal cathetersThey are cause of abdominal pain especially in pediatric age. The sensitivity of the AR is 90% and its specificity 100%5,17 of course based on its nature. Such figures recommend keeping its use in this clinical setting yet the AR should be reserved for those cases where seeing the foreign body has clinical relevance, such as batteries or toxics, or forensic relevance, or else when the patient is symptomatic.5,9 An identical approach should be followed when monitoring abdominal catheters.16
Alternatives and patterns of actionIf the AR was a new technology today, it would be difficult to justify its clinical introduction. It can be asserted with Gans et al. that its role in adults with acute abdominal pain is null today.5 Greene proposed reducing its emergency use in 1986, avoiding it in clinical situations where the odds of radiological findings are minimal, in women in fertile age, except when clearly indicated and as far as pregnancy has been ruled out, and when it is not modify clinical management. He suggests avoiding performing the abdominal series systematically and rather analyzing first the projection in the decubitus supine position complemented eventually with thorax in bipedalism, and then deciding the need for additional projections.58 An adequate clinical analytical orientation, followed by ultrasound and CT when it is negative, is today the best management pattern of the urgent abdominal pathology. So until this concept becomes generalized, it would be convenient for radiologists to follow these procedural guidelines, among others:
- •
To recognize and publicize the excessive demand, usually unjustified, for AR in Emergency Departments.
- •
To analyze the causes for its popularity among clinicians and its possible risks (Table 1).
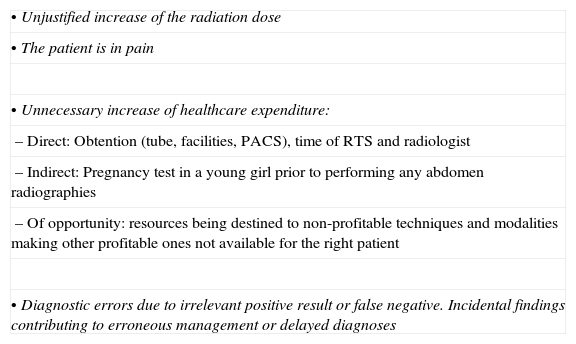
Table 1.Problems derived from using abdomen radiographies in the emergency room.
• Unjustified increase of the radiation dose • The patient is in pain • Unnecessary increase of healthcare expenditure: – Direct: Obtention (tube, facilities, PACS), time of RTS and radiologist – Indirect: Pregnancy test in a young girl prior to performing any abdomen radiographies – Of opportunity: resources being destined to non-profitable techniques and modalities making other profitable ones not available for the right patient • Diagnostic errors due to irrelevant positive result or false negative. Incidental findings contributing to erroneous management or delayed diagnoses PACS: Picture Archiving and Communication System; RTS: radiodiagnosis technical specialist.
- •
To develop and implement training programs for young physicians and foster constructive dialog in multidisciplinary sessions with senior physicians while promoting the role of the radiologist as a consultant.
- •
To develop research lines on the local, national and international level to clarify the guidelines for the use of AR (Table 2) and write them in clinical guidelines and recommendations.
- •
To control the demand for this type of examination as well as the quality of reports that should not be left at the mercy of clinicians under the consideration of a “lesser technique”.
These proposals aim to rationalize the use of AR, limit its use and offer the patients alternative modalities with a greater diagnostic yield in an effort to expedite the healthcare process and ultimately, reduce the dose of radiation, costs and unnecessary inconveniences.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments with human beings or animals have been performed while conducting this investigation.
Data confidentialityThe authors declare that the protocols of their institution on the publishing of data from patients have been followed.
Right to privacy and informed consentThe authors declare that in this article there are no personal data from patients.
Authors- 1.
Manager of the integrity of the study: JMAM, MMDG, PPH.
- 2.
Study idea: JMAM, PPH.
- 3.
Study design: JMAM.
- 4.
Data mining: CRT, DMM.
- 5.
Data analysis and interpretation: CRT, JMAM.
- 6.
Statistical analysis: NA.
- 7.
Reference search: CRT, DMM, JMAM, PPH.
- 8.
Writing: JMAM, MMDG.
- 9.
Critical review of the manuscript with intellectually relevant remarks: JMAM, MMDG, CRT, DMM, PPH.
- 10.
Approval of final version: JMAM, MMDG, CRT, DMM, PPH.
The authors declare no conflict of interests associated with this article.
This work is an update to be published in the journal Radiología exclusively. No material from former reviews or journals has been used yet some ideas and concepts were also summed up in the summary book from the 4th Meeting of SERAU 2013 “Radiología de urgencias. La oportunidad en la crisis”.
Please cite this article as: Artigas Martín JM, Martí de Gracia M, Rodríguez Torres C, Marquina Martínez D, Parrilla Herranz P. Radiografía del abdomen en Urgencias. ¿Una exploración para el recuerdo? Radiología. 2015;57:380–90.





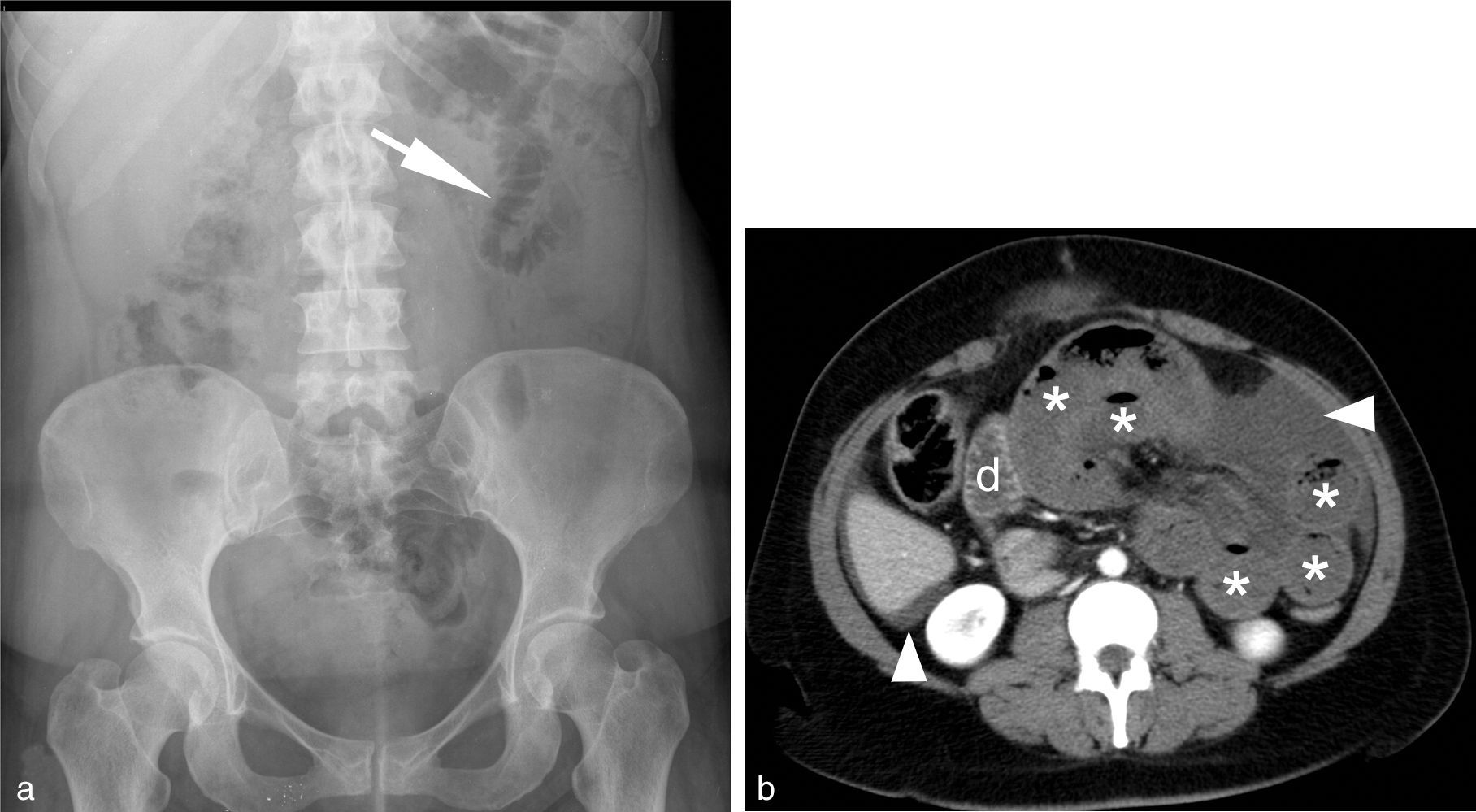



![Fifty-six (56) year-old woman at the emergency room presenting with diffuse abdominal pain and no gas or fecal expulsion. During the examination she shows poor health with the presence of tachycardia and hypotension, abdominal silence and “loop mass” palpation. The AR (a) does not show any significant findings with the exception of flexure thickening in a jejunal loop located at the left superior quadrant (arrow). (b) Computed tomography (axial view) in portal stage (70sg) of the middle abdomen region showing jejunal loop distention with no wall enhancement due to hypoperfusion (*) [compare it with the adjacent duodenum (d)]. Perihepatic intraperitoneal liquid in between the loops (arrow-heads). Surgery confirmed the diagnosis of intestinal obstruction caused by bridles complicated with strangulation; 55cm of necrotic small intestine were resected. Fifty-six (56) year-old woman at the emergency room presenting with diffuse abdominal pain and no gas or fecal expulsion. During the examination she shows poor health with the presence of tachycardia and hypotension, abdominal silence and “loop mass” palpation. The AR (a) does not show any significant findings with the exception of flexure thickening in a jejunal loop located at the left superior quadrant (arrow). (b) Computed tomography (axial view) in portal stage (70sg) of the middle abdomen region showing jejunal loop distention with no wall enhancement due to hypoperfusion (*) [compare it with the adjacent duodenum (d)]. Perihepatic intraperitoneal liquid in between the loops (arrow-heads). Surgery confirmed the diagnosis of intestinal obstruction caused by bridles complicated with strangulation; 55cm of necrotic small intestine were resected.](https://static.elsevier.es/multimedia/21735107/0000005700000005/v3_201510050314/S2173510715000543/v3_201510050314/en/main.assets/thumbnail/gr5.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)


