An infectious disease caused by a new type of coronavirus that can manifest as an acute respiratory infection was discovered in China in mid-December 2019 and soon spread throughout the country and to the rest of the world. Although chest X-rays are the initial imaging technique of choice for low respiratory infections with or without dyspnea, few articles have reported the radiologic findings in children with COVID-19.
ObjectiveTo describe the clinical, laboratory, and chest X-ray findings in pediatric patients with signs and symptoms of respiratory infection attended at our hospital in March 2020. To analyze the frequency of COVID-19 compared to other respiratory infections, and to describe the radiologic manifestations of COVID-19 in pediatric patients.
Material and methodsThis cross-sectional observational study included all children with clinical manifestations of respiratory infection (fever, rhinorrhea, cough, and/or dyspnea) that required chest X-rays in our hospital between March 1 and March 31.
ResultsA total of 231 pediatric patients (90 (39%) girls and 141 (61%) boys; mean age, 4 y, range 1 month–16 years) underwent chest X-rays for suspected respiratory infections. Most (88.4%) had mild symptoms; 29.9% had a family member positive for COVID-19 with symptoms similar to those of the patient. Nasal and/or throat swabs were analyzed for SARS-CoV-2 with PCR in the 47 (20.3%) children who presented at the emergency department; 3 (6.3%) of these were positive. Microbiological analyses were done in 85 (36.8%) of all patients, finding infections due to pathogens other than SARS-CoV-2 in 30 (35.3%). One of the patients with a PCR positive for SARS-CoV-2 had urine infection due to E. coli and blood culture positive for S. viridans. Abnormalities were observed on X-rays in 73.2% of the patients. Peribronchial thickening was the most common abnormal finding, observed in 57% of patients. Parenchymal consolidations were observed in 38.5%, being bilateral in 29.2% and associated with pleural effusion in 3.3%. The interstitial lines were thickened in 7.3%, and 7.3% had ground-glass opacities.
ConclusionDuring March 2020, COVID-19 and other symptomatic respiratory infections were observed. The radiologic pattern of these infections is nonspecific, and chest X-rays alone are insufficient for the diagnosis. Children with clinical manifestations compatible with COVID-19 (with or without PCR confirmation of infection by SARS-CoV-2) had mild symptoms and most did not require admission or invasive mechanical ventilation. In a context of community transmission, the absence of a known epidemiological antecedent should not be a contraindication for PCR to detect SARS-CoV-2.
A mediados de diciembre de 2019 se describió en China una enfermedad infecciosa causada por un nuevo tipo de coronavirus que provocaba infección respiratoria aguda y pronto se extendió por el país y por el resto del mundo. A pesar de que la radiografía de tórax es la prueba de elección inicial ante infecciones respiratorias bajas con o sin disnea, hay pocos artículos que describan los hallazgos radiológicos del niño con COVID-19.
ObjetivoDescribir las características clínicas, analíticas y los hallazgos en la radiografía de tórax de la población pediátrica atendida con clínica de infección respiratoria en nuestro hospital durante el mes de marzo. Analizar la frecuencia de COVID-19 frente a otras infecciones respiratorias y sus manifestaciones radiológicas.
Material y métodosEstudio observacional transversal desde el 1 de marzo al 31 de marzo del 2020 de todos los niños con clínica de infección respiratoria (fiebre, rinorrea, tos y/o disnea) que han precisado radiografía de tórax en nuestro hospital.
Resultados231 niños precisaron radiografía de tórax por clínica de infección respiratoria, 90 (38,9%) niñas y 141 (61%) niños; rango de edad 1 mes-16 años, con una mediana de 4 años. La mayoría de los niños presentaron síntomas leves (88,4%). Un 29,9% de los niños presentaba ambiente epidémico familiar positivo con clínica respiratoria similar a la que presentaba el paciente. Se realizó test PCR SARS-CoV-2 a 47 de los niños que acudieron a la urgencia (20,3%), que fue positivo en 3 (6,3% de los testados). Se realizaron determinaciones microbiológicas al 36,8% (85/231), demostraron otros agentes infecciosos diferentes al SARS-CoV-2 en el 35,3% de los pacientes (30/85). Únicamente uno de los pacientes PCR positivo para SARS-CoV-2 presentó infección de orina por Escherichia coli y hemocultivo positivo para Streptococcus viridans. El 73,2% de los pacientes presentó algún tipo de alteración en la radiografía de tórax. Los engrosamientos peribronquiales fueron el hallazgo más común en el 57%. El 38,5% presentó consolidación parenquimatosa, que en un 29,2% fue bilateral y en un 3,3% asoció derrame pleural. Se demostró aumento de la trama intersticial en el 7,3%. El 7,3% se manifestó con opacidades en vidrio deslustrado.
ConclusiónDurante el mes de marzo coexistieron infecciones respiratorias sintomáticas COVID-19 y no COVID-19. El patrón radiológico de las infecciones respiratorias, incluida la COVID-19, no es específico y la radiografía en ningún caso fue suficiente para establecer el diagnóstico. Los niños con clínica respiratoria compatible con COVID-19, con o sin PCR confirmatoria, presentaron síntomas leves y en su mayoría no requirieron ingreso ni ventilación invasiva. En un entorno de transmisión comunitaria, la ausencia de antecedente epidemiológico conocido no debería ser una contraindicación para realizar estudio de PCR para SARS-CoV-2.
In mid-December 2019, an infectious disease caused by a new type of coronavirus that caused acute respiratory infection was described in China and soon spread across the country and the rest of the world.
By the start of March 2020, 87,831 cases of COVID-19 had been recorded worldwide.1 On 3 March, the first coronavirus death occurred in Spain and there were 165 confirmed cases of infection. Control and prevention measures were adapted in light of the pandemic's characteristics and, on 14 March, a state of alarm was declared and a lockdown was introduced. By this point, 6391 confirmed cases and 195 deaths had already been recorded across the country.2 The Community of Madrid was declared a community transmission zone on 9 March and on 16 March 2020, of the 4695 confirmed cases in the province, 41 were children under 18 years of age (0.8%).3 According to epidemiological reports, children account for less than 2% of global cases of COVID-19.4,5 In Spain, on 1 April 2020, the National Epidemiological Surveillance Network recorded 313 children under 14 years of age among the 52,129 confirmed cases, which represented 0.6% of cases. Of these paediatric cases, 87 were hospitalised, four of them in ICU. Up to that date, only one death of a child under 2 years of age had been recorded.6 Although more articles on this new disease in the paediatric age group have gradually been published in recent months, to date there have been few articles that summarise the radiological manifestations in this age group.
The aim of this work is to describe the findings in chest X-rays of the paediatric population with clinical features of respiratory infection attended to in our hospital in March, a month with a high incidence of COVID-19 in Spain and Madrid when the virus had been circulating freely during the previous months with no lockdown measures.
Material and methodsWe conducted a retrospective, cross-sectional, observational study of all children who came to the accident and emergency department of our hospital (level IIIC maternity and children's hospital which attends to more than 50,000 paediatric emergencies per year) with upper or lower respiratory tract infection that required a chest X-ray during March 2020. The study was approved by the hospital's ethics committee.
Inclusion criteriaAll children aged 0–16 years who underwent a chest X-ray due to symptoms of respiratory infection with at least one of the following symptoms: fever, rhinorrhoea, cough or respiratory distress.
Exclusion criteriaChildren who did not have an X-ray taken or who had a clinical indication other than respiratory infection.
We collected data on demographics (age and sex), whether there was pre-existing comorbidity (heart disease, respiratory pathology, history of neoplasm, immunosuppression, etc.), the epidemiological environment history (contact with relatives or persons with respiratory infection, suspected of having COVID with or without confirmatory SARS-CoV-2 polymerase chain reaction (PCR) test), and assay and X-ray findings. A record was made of whether hospitalisation was required and, if so, for how many days and whether intensive care was necessary.
The X-ray findings were evaluated by 6 paediatric radiologists with between 6 and 30 years of experience.
Statistical analysisThe descriptive parameters were expressed as percentages, means and standard deviations. The normal distribution of the data was tested using the Kolmogorov–Smirnov test. The quantitative parameters were expressed as medians and interquartile ranges. All the analyses were performed with the programme R, version 3.6.1.7
ResultsDuring March, a total of 231 paediatric patients attended to at our hospital required a chest X-ray due to presenting clinical features of respiratory infection (with at least one of these 4 symptoms: fever, cough, respiratory distress and/or rhinorrhoea).
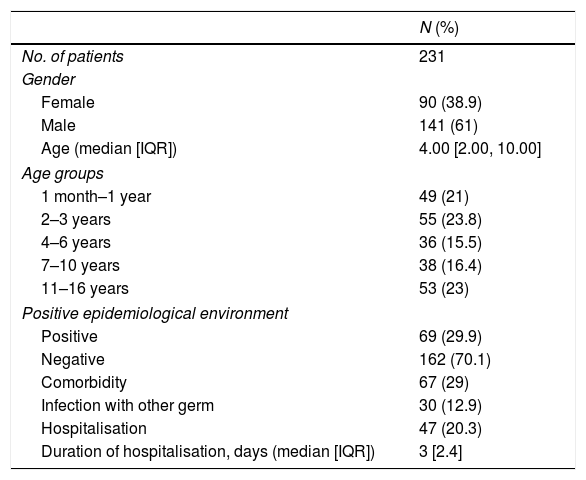
Of the 231 patients, 90 (39%) were girls and 141 (61%) were boys. Their ages ranged from 1 month to 16 years of age, with a median of 4 years. 29.9% of the children (69/231) had a history of a positive familial epidemiological environment.
71.4% of the children did not have any history of interest. 28.5% (66/231) had comorbidities, 31 had a chronic respiratory pathology (events related to bronchial hyperreactivity, for example, bronchiolitis, bronchospasm and asthma), 4 had a heart disease, 3 had a history of cancer and 2 had immunosuppression (Table 1).
Summary of patient characteristics.
| N (%) | |
|---|---|
| No. of patients | 231 |
| Gender | |
| Female | 90 (38.9) |
| Male | 141 (61) |
| Age (median [IQR]) | 4.00 [2.00, 10.00] |
| Age groups | |
| 1 month–1 year | 49 (21) |
| 2–3 years | 55 (23.8) |
| 4–6 years | 36 (15.5) |
| 7–10 years | 38 (16.4) |
| 11–16 years | 53 (23) |
| Positive epidemiological environment | |
| Positive | 69 (29.9) |
| Negative | 162 (70.1) |
| Comorbidity | 67 (29) |
| Infection with other germ | 30 (12.9) |
| Hospitalisation | 47 (20.3) |
| Duration of hospitalisation, days (median [IQR]) | 3 [2.4] |
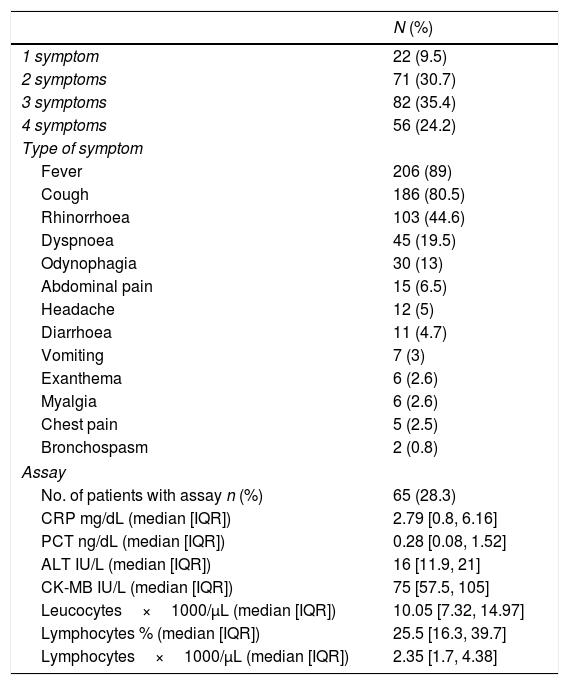
The most common symptoms that caused them to come to the accident and emergency department were fever, cough and rhinorrhoea. Other symptoms, such as diarrhoea, abdominal pain, headache, vomiting, myalgia and exanthema, were less common. The combination of three or more symptoms was the most prevalent among the patients in our study, with the combination of cough, fever and rhinorrhoea being the most common. Assays were performed on 65/231 (28.1%). The clinical-assay findings are shown in Table 2.
Summary of clinical features and assay.
| N (%) | |
|---|---|
| 1 symptom | 22 (9.5) |
| 2 symptoms | 71 (30.7) |
| 3 symptoms | 82 (35.4) |
| 4 symptoms | 56 (24.2) |
| Type of symptom | |
| Fever | 206 (89) |
| Cough | 186 (80.5) |
| Rhinorrhoea | 103 (44.6) |
| Dyspnoea | 45 (19.5) |
| Odynophagia | 30 (13) |
| Abdominal pain | 15 (6.5) |
| Headache | 12 (5) |
| Diarrhoea | 11 (4.7) |
| Vomiting | 7 (3) |
| Exanthema | 6 (2.6) |
| Myalgia | 6 (2.6) |
| Chest pain | 5 (2.5) |
| Bronchospasm | 2 (0.8) |
| Assay | |
| No. of patients with assay n (%) | 65 (28.3) |
| CRP mg/dL (median [IQR]) | 2.79 [0.8, 6.16] |
| PCT ng/dL (median [IQR]) | 0.28 [0.08, 1.52] |
| ALT IU/L (median [IQR]) | 16 [11.9, 21] |
| CK-MB IU/L (median [IQR]) | 75 [57.5, 105] |
| Leucocytes×1000/μL (median [IQR]) | 10.05 [7.32, 14.97] |
| Lymphocytes % (median [IQR]) | 25.5 [16.3, 39.7] |
| Lymphocytes×1000/μL (median [IQR]) | 2.35 [1.7, 4.38] |
ALT: alanine aminotransferase; CK-MB: creatinine kinase-MB; CRP: C-reactive protein; PCT: procalcitonin.
Pulmonary auscultation was normal in 65.3% of patients and was asymmetrical in 22.5%, mostly due to mild crackles. Hypoxaemia was recorded in only 11.6% of the children.
20.3% (47/231) of the patients required hospitalisation, with a mean duration of hospitalisation of 3.9 days [standard deviation (SD), 3.1], range 1–16 days. Three patients required admission to ICU, one of them for COVID-19. None of them required invasive mechanical ventilation.
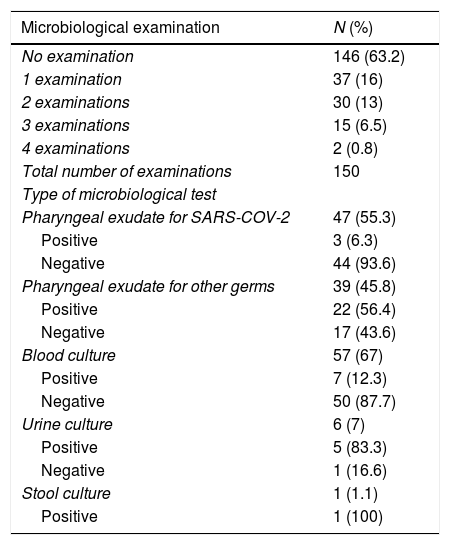
Different microbiological studies were carried out depending on the patients’ clinical features and the severity, and an infectious aetiological agent was demonstrated in 33 patients (Table 3).
Microbiological study.
| Microbiological examination | N (%) |
|---|---|
| No examination | 146 (63.2) |
| 1 examination | 37 (16) |
| 2 examinations | 30 (13) |
| 3 examinations | 15 (6.5) |
| 4 examinations | 2 (0.8) |
| Total number of examinations | 150 |
| Type of microbiological test | |
| Pharyngeal exudate for SARS-COV-2 | 47 (55.3) |
| Positive | 3 (6.3) |
| Negative | 44 (93.6) |
| Pharyngeal exudate for other germs | 39 (45.8) |
| Positive | 22 (56.4) |
| Negative | 17 (43.6) |
| Blood culture | 57 (67) |
| Positive | 7 (12.3) |
| Negative | 50 (87.7) |
| Urine culture | 6 (7) |
| Positive | 5 (83.3) |
| Negative | 1 (16.6) |
| Stool culture | 1 (1.1) |
| Positive | 1 (100) |
| Isolated germ | N |
|---|---|
| Influenza A | 4 |
| Rhinovirus | 4 |
| Mycoplasma pneumoniae | 3 |
| SARS-COV-2 | 3 |
| RSV | 2 |
| Influenza B virus | 2 |
| Escherichia coli | 2 |
| Influenza A virus+parainfluenza | 1 |
| Influenza B virus+rhinovirus | 1 |
| Rhinovirus+adenovirus | 1 |
| Adenovirus | 1 |
| Human metapneumovirus | 1 |
| Acinetobacter baumannii | 1 |
| CMV | 1 |
| EBV | 1 |
| Enterobacter cloacae | 1 |
| Neisseria | 1 |
| Streptococcus viridans | 1 |
| S. viridans+E. coli | 1 |
| Clostridium difficile | 1 |
| Total | 33 |
CMV: cytomegalovirus; EBV: Epstein-Barr virus; RSV: respiratory syncytial virus.
36.8% (85/231) of the patients underwent some type of microbiological determination: pharyngeal exudate for SARS-CoV-2 in 55.3% (47/85) or for other germs in 45.8% (39/85), blood culture and/or plasma determination in 67% (57/85), urine culture in 7% (6/85) and stool culture in 1.1% (1/85). The most common was the performance of a single test in 37/85 (16%).
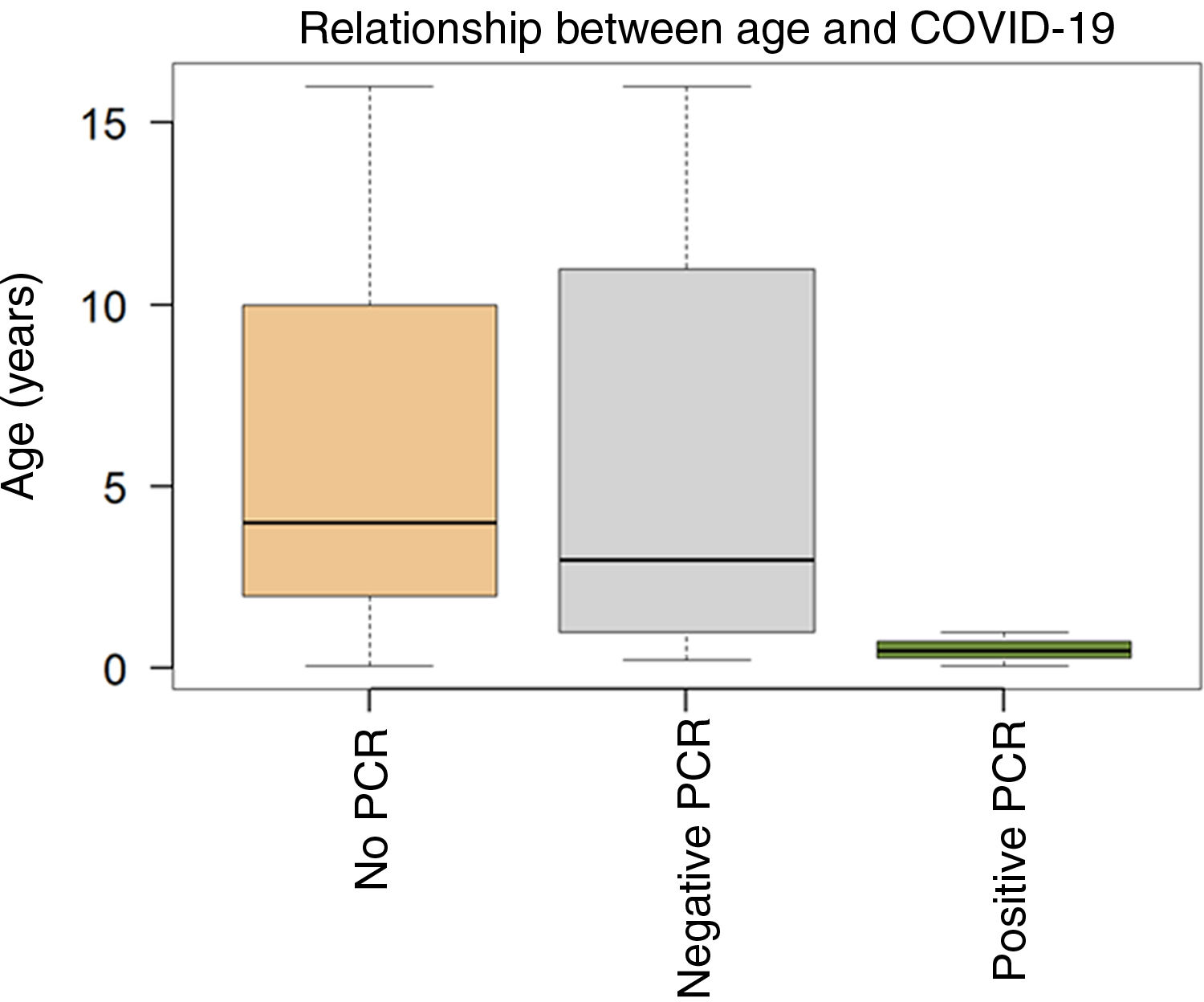
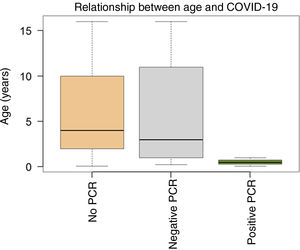
According to our hospital's clinical protocol, at that time SARS-CoV-2 PCR tests were performed on children with severe respiratory infection who required hospitalisation and on children with previous pathologies/comorbidities. The SARS-CoV-2 PCR was performed on 47 (20.3%) children and was positive in 3 (6.3% of those tested). The three COVID-19 positive patients did not have any history of interest. The relationship between age and clinical suspicion of COVID-19 infection is summarised in Fig. 1.
Age ranges by groups according to suspicion of COVID-19. Patients who did not undergo a PCR (n=187); mean age, 6 years; median, 4; range, 1 month–16 years. Children with negative SARS-CoV-2 PCR (n=41); mean age, 6 years; median, 3 range, 3 months–16 years. Children with positive SARS-CoV-2 PCR (n=3); mean age, 0.52 years (6 months); median, 0.5 years; range, 1 month–1 year.
In 27.2% (12/44) of the patients with a negative PCR for SARS-CoV-2, another kind of infectious agent was detected.
Nasopharyngeal exudate analysis for other germs was performed in 39 patients (16.8%), of which 56.4% (22/39) were positive. In one of the patients with a positive PCR for SARS-CoV-2, E. coli was isolated in urine and the blood culture was positive for S. viridans.
Multiple microbiological isolation was demonstrated in 4 patients, the majority due to respiratory viruses such as influenza A, influenza B, parainfluenza, rhinovirus and adenovirus.
The clinical indications for X-rays were the suspicion of lower respiratory tract infection or suspicion of complications.
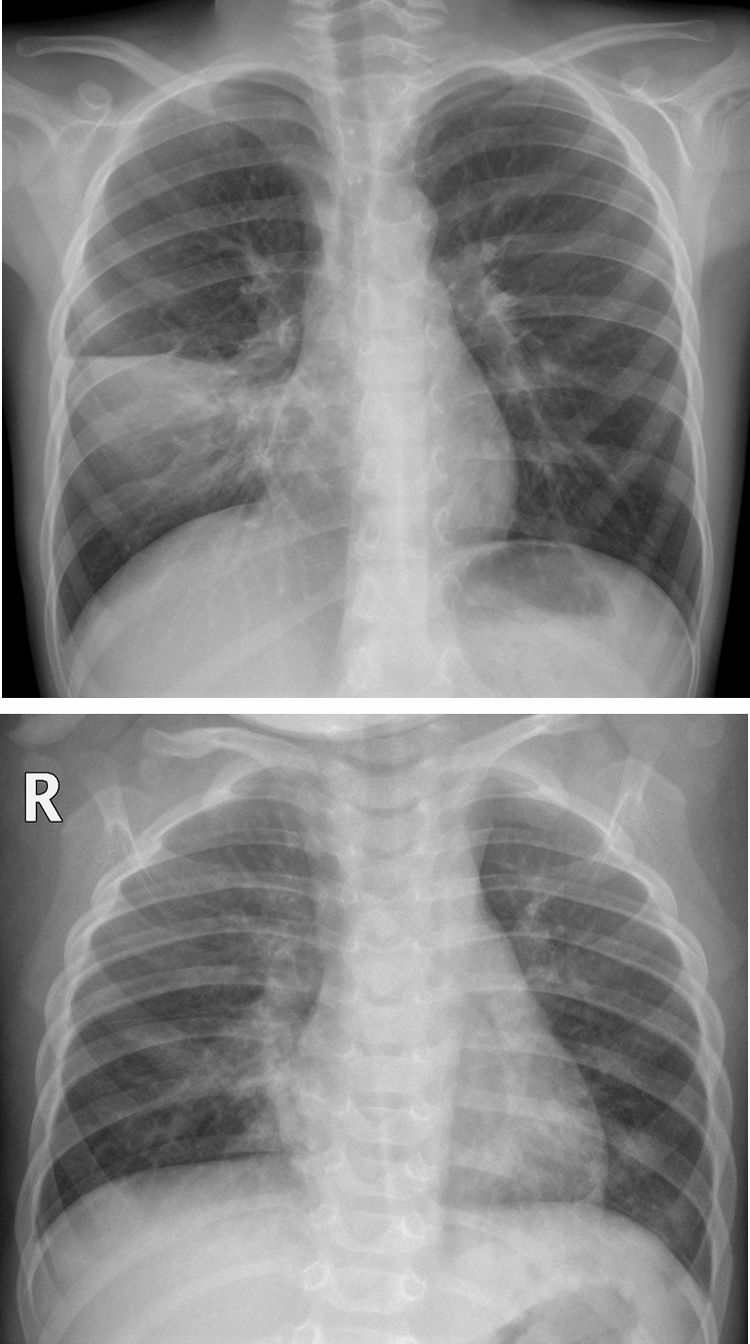
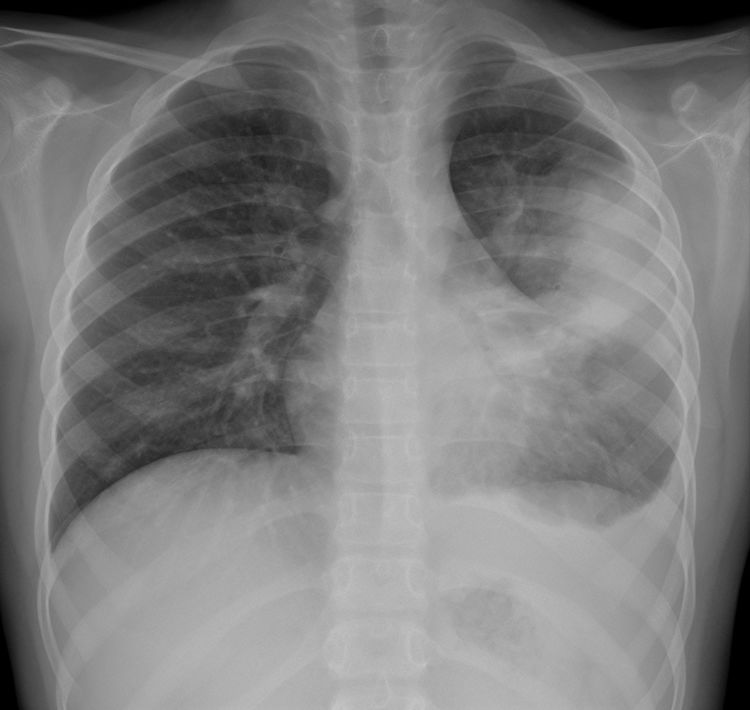
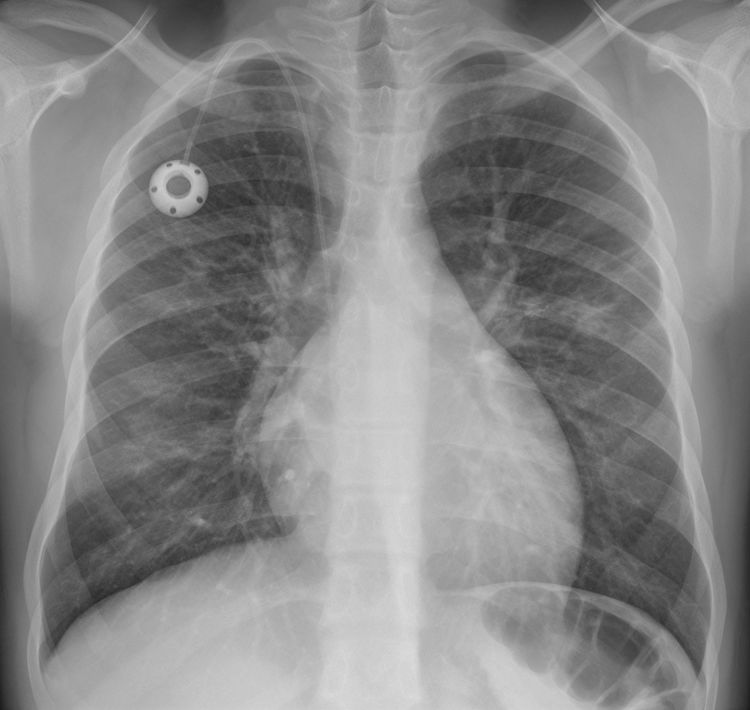
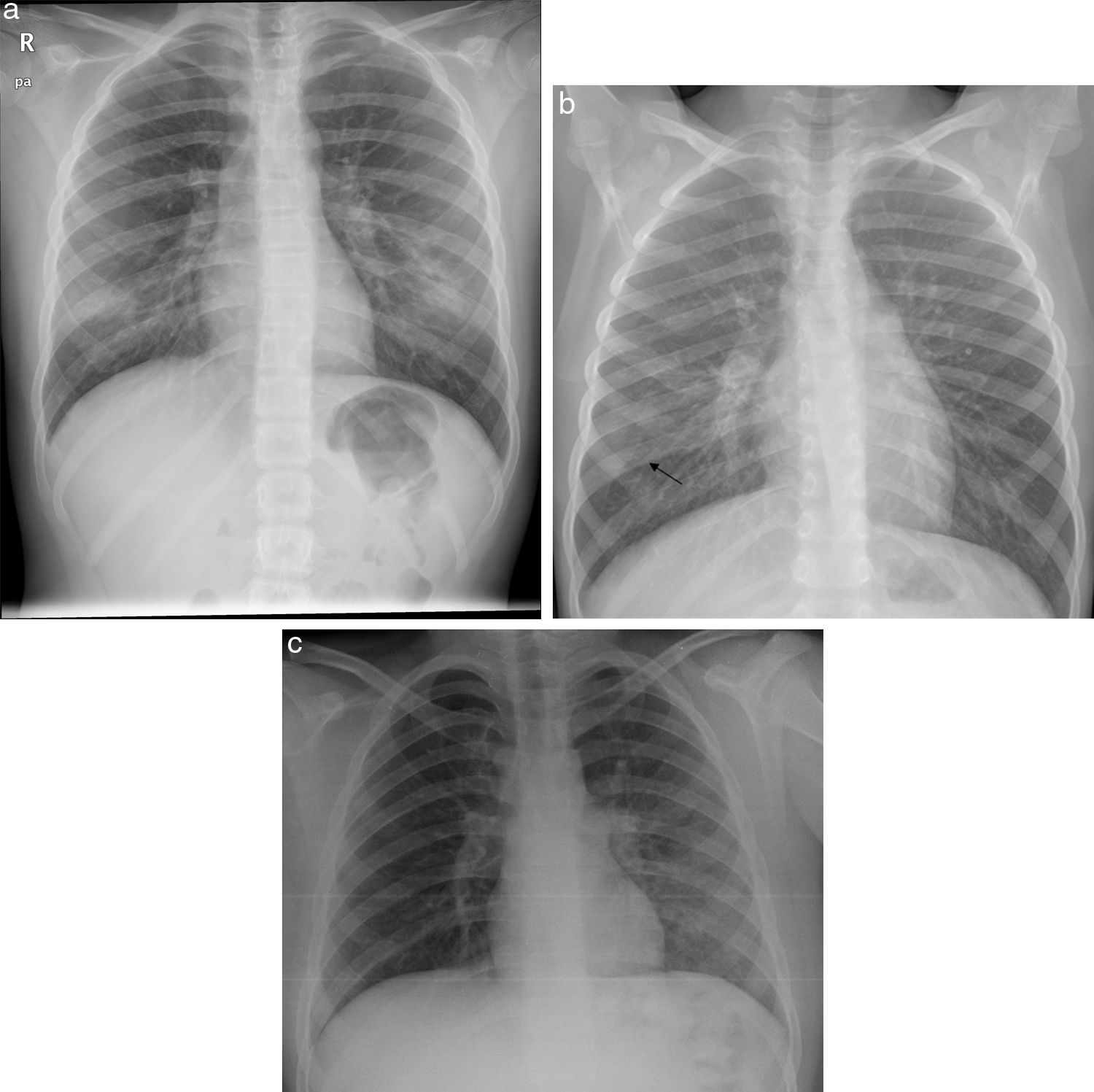
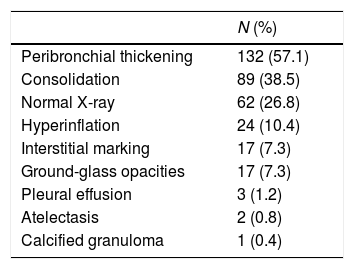
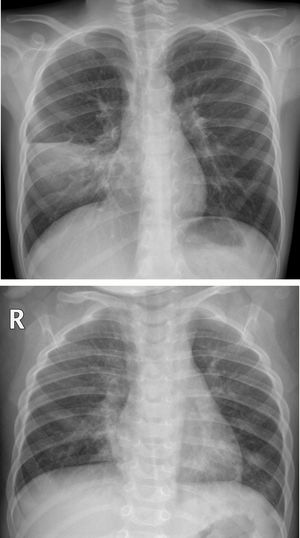
In our observational study, the X-ray findings on admission to the accident and emergency department are summarised in Table 4. 73.2% (169/231) of the patients had abnormalities in their chest X-ray. Peribronchial thickening, predominantly central, was the most common finding and was present in 57% (132/231). 38.5% (89/231) had parenchymal consolidation (Fig. 2A), which was bilateral in 29.2% (26/89) (Fig. 2B). 3.3% of the patients with consolidation also had pleural effusion, regardless of whether the consolidation was unilateral or bilateral (Fig. 3).
(A) Unilateral consolidation. 7-year-old boy with fever and cough of one week's course, with asymmetrical pulmonary auscultation. The posteroanterior X-ray showed parenchymal consolidation in the right middle lung field limited by the minor fissure, consistent with pneumonic consolidation. A SARS-CoV-2 PCR was not performed and COVID-19 was not suspected. No microbial agent was detected. (B) Bilateral consolidations. Girl aged 1 year and 2 months with fever and cough, with a family environment with similar cold symptoms. The anteroposterior X-ray shows bilateral peribronchial thickening, with areas of parenchymal consolidation in the middle lobe and left lower lobe. No SARS-CoV-2 PCR or other microbiological determinations were performed.
Consolidation with associated parapneumonic effusion in an 8-year-old girl with high fever and respiratory distress. The posteroanterior X-ray shows parenchymal consolidation in the upper-middle field of the left hemithorax with partial effacement of the heart border. There is also obliteration of the left lateral costophrenic angle associated with pleural effusion. She was hospitalised for 5 days with intravenous antibiotic therapy with a favourable course. No microbial agent was detected in the samples obtained and the SARS-CoV-2 PCR was negative.
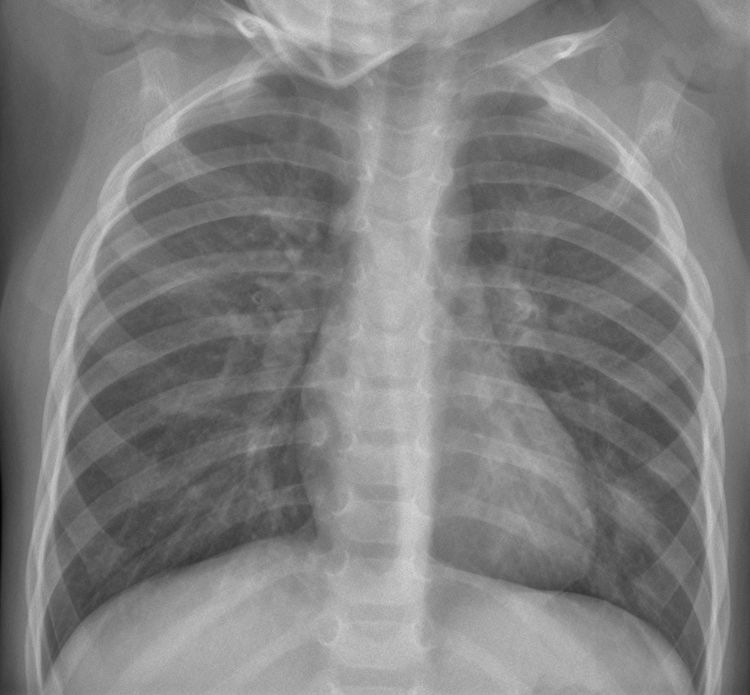
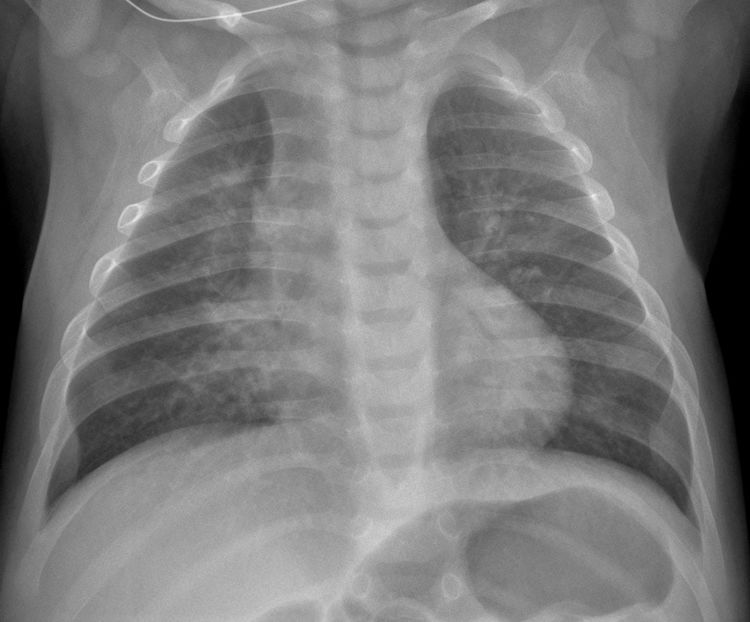
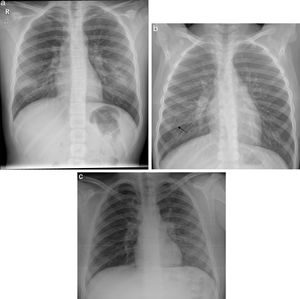
10.4% (24/231) of the patients had pulmonary hyperinflation (Fig. 4). 7.3% (17/231) had increased interstitial markings (Fig. 5). 7.3% (17/231) had ground-glass opacities, in 8 of these 17 cases, the opacities were bilateral (Fig. 6A) and in 5 of 17 cases, the distribution was subpleural (Fig. 6B) (Mycoplasma infection was demonstrated in one of the patients with this involvement (Fig. 6C).
Pulmonary hyperinflation and peribronchial thickening. 1-Month-old boy with respiratory distress, cough and bilateral crackles. The anteroposterior X-ray shows signs of pulmonary hyperinflation and bilateral perihilar and paracardiac peribronchial thickening, with no parenchymal consolidations. No SARS-CoV-2 PCR or other microbiological determinations were performed.
Increased interstitial markings. A 15-year-old adolescent with sickle cell anaemia and dilated myocarditis, with cough of 10 days’ course and hypoxaemia; a chest X-ray was performed with suspicion of COVID-19. The posteroanterior X-ray shows small faint opacities in the left and right middle lung fields, as well as increased interstitial markings. The cardiac silhouette is on the upper limit of normality with prominent hila and reservoir catheter with end in superior vena cava. The SARS-CoV-2 PCR was negative, and no other germs were detected in the microbiological study.
(A) Bilateral ground-glass opacities. 10-year-old girl with respiratory distress and signs and symptoms of fever of 4 days’ course associated with dry cough and rhinorrhoea. Positive familial epidemic context for COVID-19. The posteroanterior X-ray shows a slight increase in ground-glass density in the lower third of both hemithoraxes. No type of microbiological determination was performed, although it was clinically labelled as probable COVID-19. (B) Subpleural ground-glass opacity. 7-year-old boy with fever and cough of 5 days’ course, with a familial epidemic context positive for COVID-19. The anteroposterior X-ray shows a slight increase in subpleural ground-glass density in the middle-lower third of the right hemithorax (arrow), probably defined medially by the major fissure. No SARS-CoV-2 PCR or other microbiological determinations were performed; however, it was labelled as probable COVID-19. (C) Ground-glass opacities caused by Mycoplasma pneumoniae. 11-year-old boy with cough and fever of 8 days’ course (max. 39.5°C) with odynophagia. The portable supine decubitus X-ray shows increased ground-glass density with an increase in bronchovascular marking in the middle-lower field of the left hemithorax. In the assay, he had leucocytosis (14.9×1000/μL) and increased acute phase reactants (CRP 2.9mg/dL and procalcitonin 14ng/dL). Negative SARS-CoV-2 detection. He required hospitalisation for 3 days with good clinical course.
If we analyse according to severity/radiological pattern, no significant differences are found.
Of the 3 children admitted to the ICU, one was positive for COVID-19 with E. coli urinary infection. The other 2 patients had meningococcal sepsis with co-infection by Candida parasilopsis, and the other patient had a human metapneumovirus respiratory infection. These severe children did not have any significant abnormalities in the chest X-ray, and only one had pulmonary hyperinflation with peribronchial thickening (Fig. 7). Admission was based on clinical and assay criteria (median leucocytes 10.05×1000/μL; median PCR 2.79mg/dL).
Human metapneumovirus infection. Boy aged 2 years and 4 months with fever and asymmetry in his auscultation; severe bronchospasm. The anteroposterior X-ray shows signs of bilateral and symmetrical pulmonary hyperinflation, peribronchial thickening and bilateral interstitial pattern. There is a small paracardiac opacity in the base of the left lung that may be a small atelectasis/mucus plug. No SARS-CoV-2 PCR was performed. He required admission to ICU with leucocytosis of 18.7×1000/μL and CRP 6.09mg/dL. He had a favourable course and was discharged after 3 days.
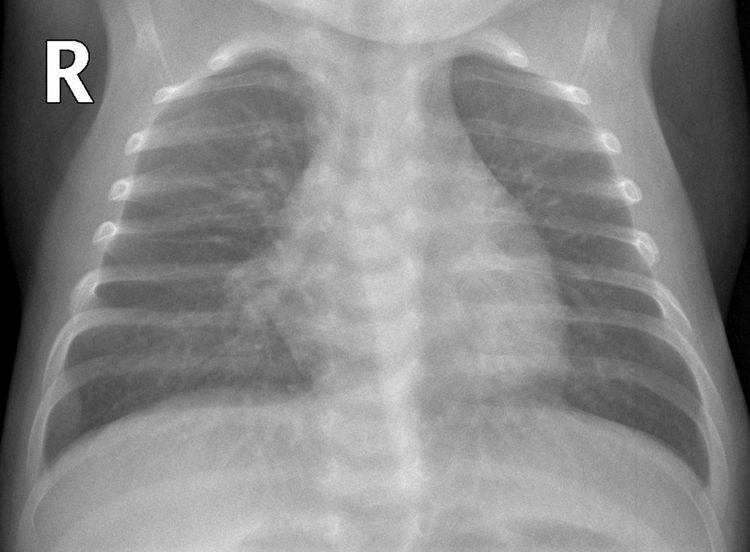
In the 3 children with confirmed COVID-19, different radiological manifestations were found, and given the small number it is not possible to describe a radiological pattern in our series. Of these 3 patients, only one showed parenchymal consolidation (Fig. 8).
COVID-19 with parenchymal consolidation. 6-month-old boy with fever and cough. The anteroposterior X-ray shows peribronchial thickening and faint opacity that blurs the right contour of the cardiac silhouette in association with parenchymal consolidation in the middle lobe. The SARS-CoV-2 PCR was positive.
Respiratory tract infections in children are one of the main causes of infant morbidity and mortality, and one of the main reasons behind visits to accident and emergency.8 The causative organisms may be viral, bacterial or atypical germs, but it is not possible to differentiate them based on radiological findings. In the youngest children, influenced by the immaturity of the immune system, there is a predilection for respiratory viruses.9,10 With the pneumococcal and Haemophilus influenzae conjugate vaccine, viral pathogens are starting to predominate. Similarly, a meta-analysis by Polack11 suggests that respiratory pathogens in paediatrics are changing, with an increase in pneumonias caused by more than one microorganism.
The respiratory syncytial virus (RSV) is the virus most commonly associated with pneumonia (15–40%), followed by the influenza A and B viruses, parainfluenza, human metapneumovirus and adenovirus.8 In our study, rhinovirus and influenza A virus were the most common, followed by Mycoplasma, influenza B virus, RSV, adenovirus and human metapneumovirus; the three recorded multiple isolations were rhinovirus-adenovirus, rhinovirus-influenza B and parainfluenza-influenza A virus. As this was an observational study during March, there is a seasonal bias, as different respiratory viruses circulate depending on the season.
In the context of respiratory infection in paediatrics, there is no specific pattern in conventional chest X-rays that enables us to establish the aetiological diagnosis of the infection. There is an overlap, both in terms of clinical features and the radiological manifestation, between respiratory infections caused by viruses (for example, influenza A virus and influenza B virus, among others), Mycoplasma12 and even COVID-19 infection, for which no specific findings have been described to date.13,14 The radiological pattern also makes it necessary to include inflammatory processes, such as hypersensitivity pneumonia and eosinophilic pneumonia, which we did not detect in our study, in the differential diagnosis. The most common radiological pattern in our study was peribronchial thickening, present in 57% of patients. This is the most common finding described in distal airway infections in children,15,16 but it is also a subjective sign with large interobserver variability.17
Despite the exponential increase of confirmed COVID-19 cases in our country and particularly in the Community of Madrid during March, the observed incidence of other symptomatic respiratory infections was higher than that of COVID-19, although this data is biased since many children with COVID-19 infection with mild or no symptoms did not go to hospital and PCR tests were not performed on all patients with respiratory symptoms.
It is known that SARS-CoV-2 affects everybody, children and adults.4 In the biggest series described by the Chinese Centre for Disease Control and Prevention of 72,314 cases, less than 2% were children.4 In children, there is no gender predilection and the manifestations are generally milder than in adults. However, within the paediatric population, infants are more vulnerable.18,19 In our series, we have observed that all COVID-19 cases are infants under 1 year of age, a finding that is consistent with the scientific literature. Consistent with this observation is the fact that, in our series, it is noteworthy that the COVID-19 positive group was younger than both negative groups and those that did not undergo PCR.
A positive familial epidemic environment is often associated with this type of infection.20 However, in our study, even though there was not a significant number of cases, in two of the three COVID-19 patients, it was reported that they did not have any relatives with COVID-19 or contacts who were a known risk at the time of the diagnosis.
The clinical manifestations in children are similar to those in adults (fever and cough), although diarrhoea, rhinorrhoea and abdominal pain have also been described.21–23 Manifestation as toxic or atypical Kawasaki disease, which may be associated with respiratory symptoms and fever, has been reported recently. This is believed to be a post-COVID inflammatory syndrome,24,25 but at the time of the study no cases of this type had been described in the literature.
The main route of transmission of the new coronavirus is, as in adults, through respiratory droplets or direct contact, and it is highly contagious. One the current hypotheses for children having a lower risk of infection by the new coronavirus is the lower expression, compared to adults, of nasal angiotensin-converting enzyme 2 (ACE2) receptors, which have been demonstrated to be a gateway for SARS-CoV-2 host entry.26
Even though it is the first choice test in lower respiratory infections with or without dyspnoea, there are hardly any articles describing chest X-ray findings in children with COVID-19. A lot of case series combine the description of the findings of the X-ray and the chest CT scan and, in a lot of articles, none of the authors were radiologists. Based on the specialist literature, chest X-rays are much less sensitive than computed tomography in terms of identifying pulmonary involvement in this disease. This is true to such an extent that the study by Choi et al. described a sensitivity of 25% and a specificity of 90%.27 In the few case series published to date, the majority of children with COVID-19 had no abnormalities in their chest X-ray.28 The most common findings in the children who did have abnormalities were focal or diffuse airway involvement with consolidation or ground-glass opacities.13,29 In children with severe clinical involvement admitted to intensive care units, the most common findings were parenchymal consolidations or ground-glass opacities, both multifocal and unilateral or bilateral.30
This study has several limitations. It is notable that, despite the exponential growth in confirmed cases in the Community of Madrid throughout March, the number of patients with a positive PCR for SARS-CoV-2 is very low in our series. However, these findings could be influenced by several factors, for example: the low detection capacity due to the scarcity of available PCR diagnostic tests; the test's low sensitivity, which in nasopharyngeal exudate is 32–71%,31 although this figure may have improved in this time32; low sensitivity that could also be exacerbated in children due to the low nasal viral load as they have fewer nasal receptors; and, lastly, that the incidence of COVID-19 is higher, as asymptomatic patients who did not need to attend hospital accident and emergency departments and who did not undergo the diagnostic test were not taken into account.
Conclusion- •
The radiological pattern of respiratory infections in children, including COVID-19, is not specific and in no cases were X-rays enough to establish the diagnosis.
- •
Children with respiratory symptoms consistent with COVID-19, with or without confirmatory PCR, had mild symptoms and most of them did not require hospitalisation or mechanical ventilation.
- •
Given that in our study, two of the three patients with a PCR positive for COVID-19 did not have risk contacts or a family history of COVID-19 infection, it can be concluded that, in a community transmission environment, the absence of a known epidemiological history should not be a contraindication for a PCR test, although more studies are needed to confirm this.
- 1.
Responsible for the integrity of the study: EAP.
- 2.
Study conception: EAP, CGH, DCR.
- 3.
Study design: EAP, CGH, DCR, MNI.
- 4.
Data collection: EAP, DCR.
- 5.
Data analysis and interpretation: EAP, CGH, DCR, MNI.
- 6.
Statistical processing: EAP, MNI.
- 7.
Literature search: EAP, MRP, MNI.
- 8.
Drafting of the article: EAP, CGH, DCR, MNI.
- 9.
Critical review of the manuscript with intellectually significant contributions: EAP, CGH, DCR, MNI, MRP.
- 10.
Approval of the final version: EAP, CGH, DCR, MNI, MRP, MPV.
The authors declare that they have no conflicts of interest.
Please cite this article as: Aguirre Pascual E, Coca Robinot D, Gallego Herrero C, Navallas Irujo M, Rasero Ponferrada M, Pont Vilalta M. Radiografía de tórax pediátrica en la era COVID. Radiología. 2021;63:106–114.