Magnetic resonance imaging (MRI) with gadoxetic acid is widely used in clinical practice in Spain for the diagnosis, treatment, and follow-up of patients with liver metastases, although its use varies. This paper aims to provide recommendations for the use of MRI with gadoxetic acid in the detection and diagnosis of liver metastases in clinical practice in Spain.
Material and methodsThis project was undertaken by a group of nine experts who analyzed a series of recommendations about the use of gadoxetic acid extracted from international consensus documents. From this analysis, the experts decided to reject, adopt, contextualize, or adapt each of the recommendations. Once established, the final recommendations were voted on by the same group of experts.
ResultsThe experts reached a consensus about five recommendations related to the use of this imaging technique in the management of liver metastases in three clinical situations: (i) in the detection, (ii) in the diagnosis and preoperative characterization, and (iii) in the detection after a chemotherapy treatment.
ConclusionThe results support a clinical benefit for MRI with gadoxetic acid in the detection of liver metastases, favoring preoperative planning, especially in metastases measuring less than 1 cm, thus facilitating early diagnosis of metastatic spread.
La resonancia magnética (RM) con ácido gadoxético es una técnica ampliamente usada en la práctica clínica en España para el diagnóstico, tratamiento y seguimiento de pacientes con metástasis hepáticas, aunque existe variabilidad en su uso. El objetivo de este trabajo fue emitir recomendaciones acerca del uso de la RM con ácido gadoxético en la detección y diagnóstico de metástasis hepáticas en el contexto de la práctica clínica en España.
Material y métodosEste proyecto ha sido realizado por un grupo de nueve expertos que analizaron una serie de recomendaciones sobre el uso de ácido gadoxético extraídas de documentos de consenso internacionales. A partir de este análisis, los expertos decidieron rechazar, adoptar, contextualizar o adaptar cada una de las recomendaciones. Una vez establecidas, las recomendaciones finales fueron votadas por el mismo grupo de expertos.
ResultadosLos expertos consensuaron 5 recomendaciones relacionadas con el uso de esta técnica de imagen en el manejo de metástasis hepáticas en tres situaciones clínicas: 1) en la detección, 2) en el diagnóstico y caracterización preoperatoria y 3) en la detección tras un tratamiento quimioterápico.
ConclusiónLos resultados apoyan el beneficio clínico de la RM con ácido gadoxético en la detección de metástasis hepáticas, favoreciendo la planificación preoperatoria, especialmente en aquellas menores de 1 cm, facilitando así el diagnóstico temprano de la diseminación metastásica.
The development of liver metastases is very common in the course of cancer, and metastasis is the most common malignant liver lesion.1 Early diagnosis and accurate differentiation and staging of malignant lesions is essential for the right treatment. Early detection of liver metastases prolongs the survival of patients treated surgically and improves the outcome in patients treated with chemotherapy.2
There are currently various diagnostic tests which have different degrees of sensitivity and specificity for the detection of liver metastases.3 Among the most useful techniques are ultrasound (US), computed tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography (PET).
Conventional US achieves a sensitivity of 69%. However, the addition of contrast methods to the ultrasound technique (contrast-enhanced US [CEUS]) improves the sensitivity and specificity in the detection of liver metastases from primary extrahepatic tumours of different origins.4,5 Multiphase CT achieves greater sensitivity (92%) in the detection of hypovascular liver metastases.6 Although PET reflects the metabolic activity of tumour cells, it has low spatial resolution, so is particularly recommended for the detection of extrahepatic lesions.7 Various studies8–10 show that MRI is the imaging technique with the best performance in the detection and characterisation of liver metastases. On that basis, MRI is proposed as first-choice technique for assessing colorectal liver metastases in patients who have had no prior therapy, as it can provide anatomical details and a high detection rate even in lesions less than 10 mm in size.9 Although MRI can be performed without contrast for the detection of liver lesions, the use of liver-specific contrast media is reported to increase its sensitivity, in addition to having a series of advantages over other imaging techniques or other contrast media.11,12
Unlike non-liver-specific contrast media, the liver-specific contrast media, such as gadoxetic acid and gadobenate dimeglumine, were designed to differentiate liver lesions. There is a lack of comparative studies on the use of non-liver-specific contrasts and liver-specific contrast agents for the detection of liver metastases. In 2014 Ding et al. compared the sensitivity and specificity of gadopentetate dimeglumine and gadoxetic acid with the hepatobiliary phase, with gadoxetic acid showing greater sensitivity and specificity, especially in small lesions.13
Among the liver-specific contrast media, the main differences lie in the excretion route, the intensity of the hepatocellular phase and the image acquisition time.6,14 In terms of cost-effectiveness, the evidence suggests that MRI with gadoxetic acid should be the initial imaging procedure of choice to assess liver resectability in patients with colorectal and neuroendocrine liver metastases.15,16 However, the availability of studies comparing the different liver-specific contrast agents, and gadoxetic acid and gadobenate dimeglumine in particular, is very limited.
Despite its common application in clinical practice in Spain, due to the lack of comparative studies with other liver-specific and non-liver-specific contrast media, and the heterogeneity in its use, it would be of great interest to learn what experts think about the use of gadoxetic acid, and to define and update clinical guidelines to optimise and reduce variability in its use at a local level.
In this context, our aim here is to review a series of international recommendations and adapt them to the situation in Spain, in accordance with the clinical experience and opinion of a group of Spanish experts.
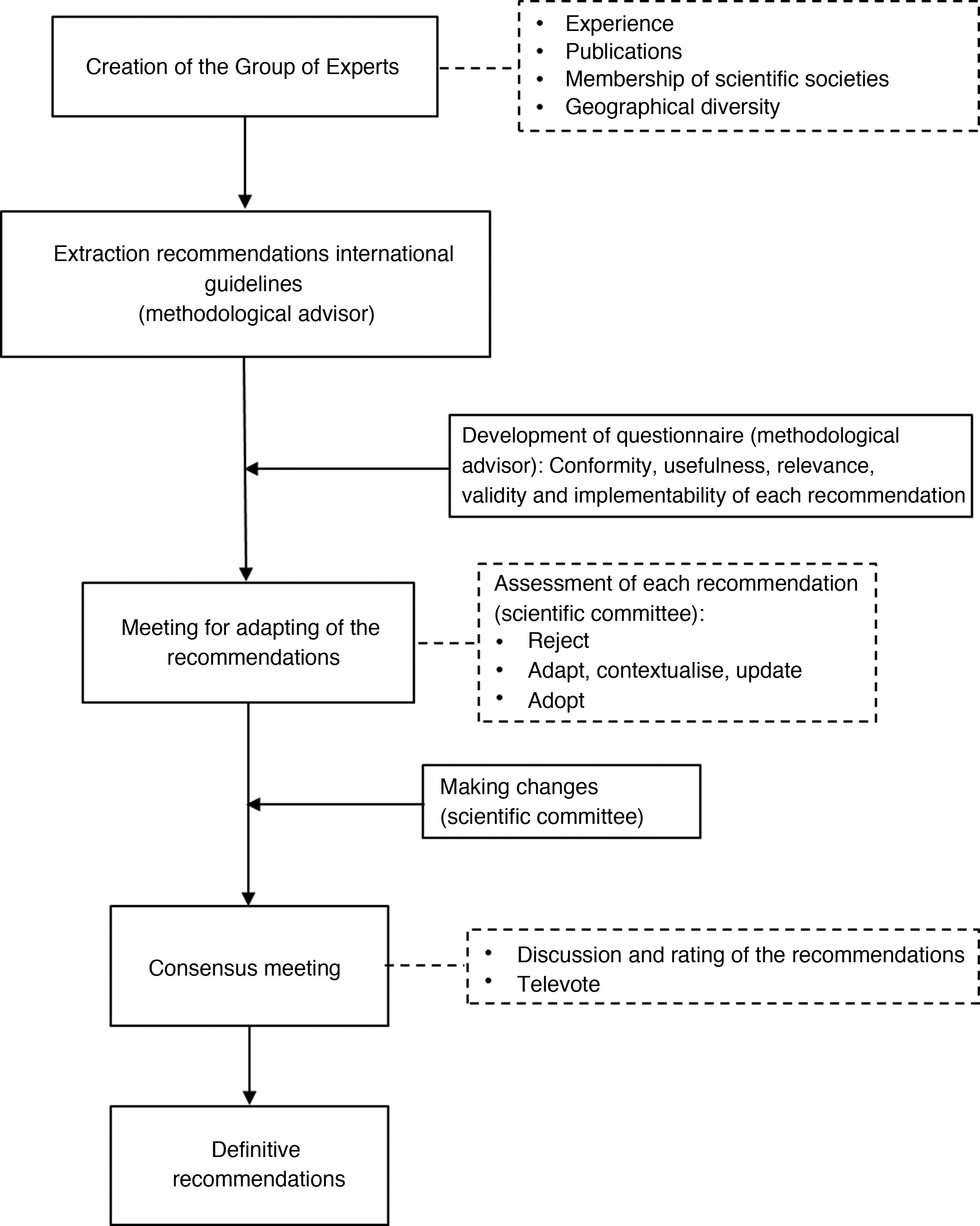
Material and methodsCreation of the working groupIn conjunction with the sponsor of the project (BAYER), a coordinating committee was initially formed, made up of two radiologists, the last two signatories of this article, who were responsible for approving the methodology, defining the objectives, identifying the literature references, proposing the individuals who would sit on the expert group (EG) and reviewing and validating the results of the project. The EG was composed of eight radiologists (including the two members of the coordinating committee) and one hepatobiliary surgeon, from eight hospitals in Spain, one secondary level care, but the rest all tertiary care hospitals, which had hepatobiliary units. The experts were chosen based on their broad background and professional experience in this field. They all had more than ten years of experience in abdominal radiology and in the management of patients with liver lesions, over ten years of experience in the use of gadoxetic acid, and on average saw from 100 to 300 patients a year. Participation in scientific societies and varied territorial representation were also considered in the selection process for this working group.
The methodology followed for obtaining recommendations is described in Fig. 1.
Review of international consensus documents and previous publicationsAt the beginning of this project, the methodological advisor (GOC Health Consulting) carried out a review of international consensus documents containing recommendations for the use of MRI with gadoxetic acid published up to 2018 in electronic databases (Medline/PubMed, EMBASE, Cochrane). In view of the project’s objectives, the search included the terms “gadoxetic acid”, “contrast agent”, “MRI” and “liver metastases”. “Ten documents were identified, four of which were selected by the methodological advisor to prepare the recommendations, based on their relevance to the scope of the project and recent date of publication: 1) “Consensus Statements from a multidisciplinary expert panel on the utilization and application of a liver-specific MRI contrast agent — gadoxetic acid”17; 2) “ESGAR consensus statement on liver MT imaging and clinical use of liver-specific contrast agents”18; 3) “Consensus Report of the Third International Forum for Liver Magnetic Resonance Imaging”19; 4) “Consensus report from the 7th International Forum for Liver Magnetic Resonance Imaging”.20 Once these documents were selected, the methodological advisor analysed the recommendations made in each one regarding the use of gadoxetic acid in the detection and diagnosis of liver metastases, as well as the evidence on which they were based. The review process was then validated jointly by the experts, with the aim of identifying whether each of the recommendations needed to be adapted in the context in which it applied.
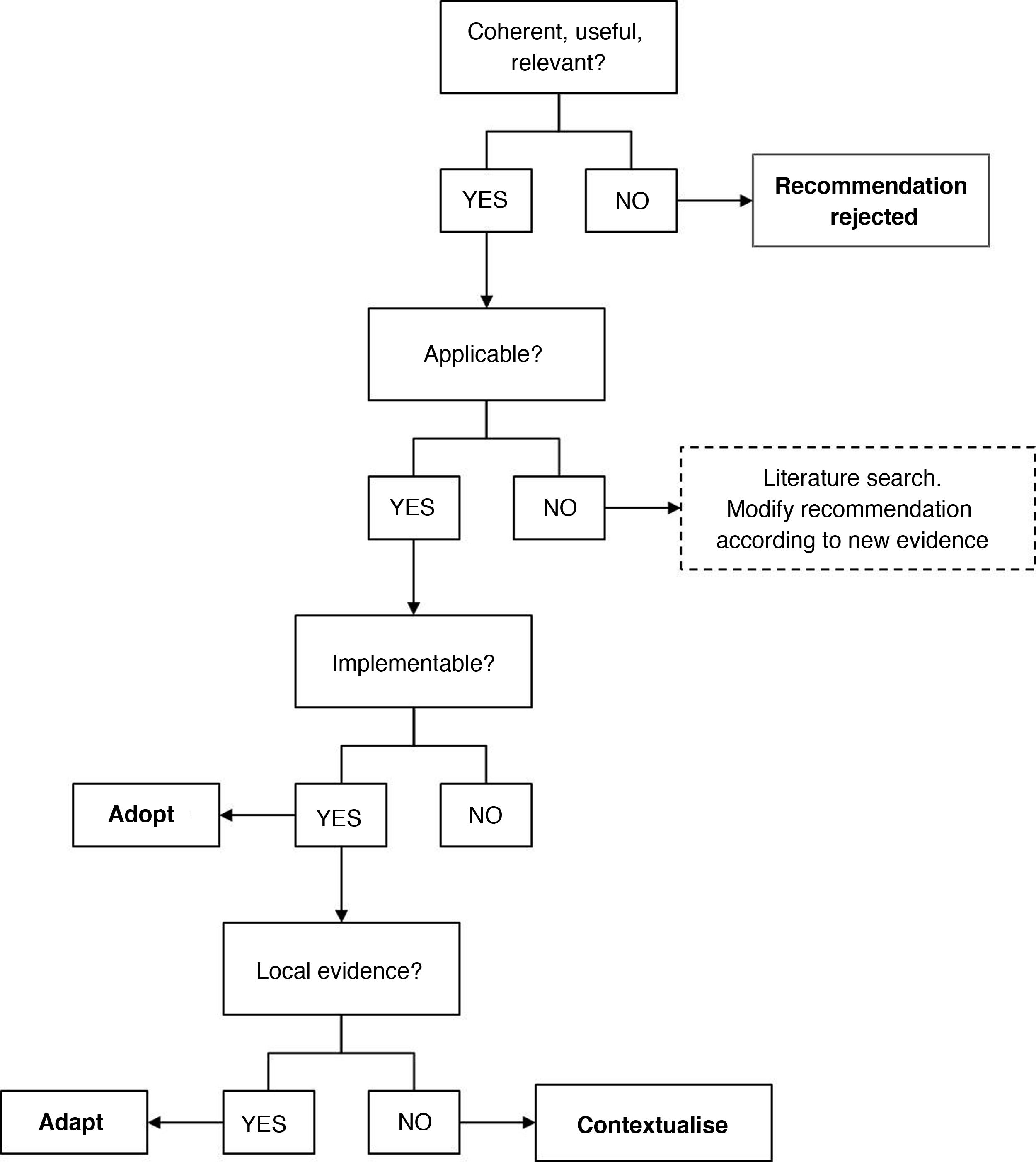
Questionnaire on the need to adapt the recommendationsTo categorise the recommendations, a structured decision-making process was applied, based on the evaluation of conformity, usefulness, relevance, validity, implementability and existence of local evidence, using the algorithm shown in Fig. 2. The questions in the questionnaire were formulated based on an adaptation of the criteria described in the methodological manuals21,22 and are shown in Table S1 of the Supplementary material. The members of the EG completed the questionnaire and the aggregate results were shared in a face-to-face session, in which the EG discussed and agreed on the relevance of the recommendations and whether or not they needed to be adapted. At this meeting, using the same methodology as the questionnaire, three types of decisions were made on the recommendations following the methodological recommendations of the ADOLOPMENT proposal: 1) adoption; 2) adaptation; or 3) contextualisation.23,24
Making changes to adapt the recommendationsAfter identifying which recommendations were not applicable and which could be adapted or contextualised, a literature search was carried out to review and/or complete the supporting evidence. The recommendations finally formulated were based on the judgement and experience of the experts in the subject at hand, and on the evidence found, to ensure that they were consistent with Spanish clinical practice. After this assessment, the experts agreed on contextualisation of the recommendations as described in Appendix B Table S2 of the Supplementary material.
Consensus meetingThe last step involved the EG meeting to discuss and validate the changes made to each recommendation. These were submitted for debate and then, by a televote, the percentage agreement was obtained for adopting each of the recommendations finally proposed. Recommendations in which the percentage agreement was 80% or above were accepted, considering those between 80% and 100% as a consensus agreement and those with 100% as unanimous. The data from the televote are shown in Table 1.
Recommendations for the use of gadoxetic acid in the diagnosis and characterisation of liver metastases. The percentage of agreement corresponds to the degree of consensus in the approval of the recommendations after the adaptations applied.
| Recommendations | Percentage agreement (PA) |
|---|---|
| 1. Use of gadoxetic acid as a technique for detecting liver metastases | |
| a. MRI with gadoxetic acid is the most sensitive technique for the detection of liver metastases, in particular for very small-sized metastases, and is the technique of choice in potentially resectable lesions, candidates for rescue surgery and radical ablative treatments. | 100% |
| 2. Use of gadoxetic acid in the diagnosis and preoperative characterisation of liver metastases | |
| a. In preoperative planning, for an accurate assessment of liver metastases and to establish an adequate surgical plan, liver MRI with gadoxetic acid is recommended, as it has been shown to have higher sensitivity and specificity compared to ultrasound, PET and CT | 100% |
| b. The combination of the hepatobiliary phase with gadoxetic acid and diffusion-weighted imaging provides the highest sensitivity for the preoperative diagnosis of liver metastases | 100% |
| 3. Use of gadoxetic acid in the detection of liver metastases after chemotherapy treatment | |
| a. In the assessment of patients with liver metastases who have been treated with chemotherapy, gadoxetic acid is of particular benefit in preoperative management | 100% |
| b. In the assessment of patients treated with chemotherapy, when the differential diagnosis is between benign hepatocellular lesion and metastasis, the use of MRI with liver-specific contrast agents is recommended, particularly for detecting nodular hyperplasia | 100% |
Six recommendations were selected from international consensus documents in the field being studied; five of them were contextualised and in four, new evidence was provided to give them validity (Appendix B Table S2, Supplementary material). Only one was discarded, as it was similar to recommendation 1 after the changes had been made, and therefore not considered relevant (Appendix B Table S3, Supplementary material).
The five recommendations finally issued by the expert group correspond to three clinical situations: 1) use of gadoxetic acid as a technique for detecting liver metastases; 2) use of gadoxetic acid in the diagnosis and preoperative characterisation of liver metastases; and 3) use of gadoxetic acid in the detection of liver metastases after chemotherapy. The recommendations are shown below with the percentage agreement (PA) (Table 1).
DiscussionUse of gadoxetic acid as a technique for detecting liver metastasesMRI with gadoxetic acid is the most sensitive technique for the detection of liver metastases, in particular for very small-sized metastases, and is the technique of choice in potentially resectable lesions, candidates for rescue surgery, and radical ablative treatments (PA: 100%). SeeTable 1a.
The original recommendation19 was considered coherent, useful and relevant, and was contextualised by the expert group (Appendix B Table S2, Supplementary material), based on their clinical experience and the following evidence.
Several meta-analyses have been carried out showing that MRI is superior to CT in the detection and characterisation of liver metastases,8–10,17 and although PET with 18F-fluorodeoxyglucose (18FDG PET-CT) is a cost-effective tool in the evaluation of extrahepatic/extrapulmonary disease, in patients diagnosed with local recurrence, MRI is the modality of choice to assess local spread.25 In addition, the use of specific contrast agents for the liver gives MRI greater sensitivity in the detection of metastases.26,27 With the use of gadoxetic acid in the hepatobiliary phase, both hypovascular and hypervascular liver metastases appear hypointense in relation to the adjacent parenchyma due to the absence of functional hepatocytes in these lesions.28 In this phase, the washing of the lesion, associated with the enhancement of the surrounding healthy parenchyma, improves the liver-tumour contrast, increasing the conspicuousness of the lesion and enabling a higher rate of lesion detection.28 However, as published in the ESGAR consensus,18 there are few comparative studies available on the efficacy of gadoxetic acid and gadobenate dimeglumine in detecting liver metastases.
Use of gadoxetic acid in the diagnosis and preoperative characterisation of liver metastasesTo avoid failure in the treatment in our patients and to obtain better outcomes, the correct identification and preoperative characterisation of liver metastases is crucial for optimal tumour resection. It is therefore appropriate to make recommendations in this area.
In preoperative planning, for an accurate assessment of liver metastases and to establish an adequate surgical plan, liver MRI with gadoxetic acid is recommended, as it has been shown to have higher sensitivity and specificity compared to US, PET and CT (PA: 100%). SeeTable 1.
The original recommendation17 was considered coherent, useful and relevant, and was contextualised by the expert group (Appendix B Table S2, Supplementary material), based on their judgement and clinical experience and the following evidence.
Compared to dynamic CT, liver-specific MRI contrast media, and gadoxetic acid in particular, have shown superior sensitivity and specificity for the detection and characterisation of liver metastases, particularly for small lesions, making it a useful modality for assessing patients who are candidates for liver resection.8,9,11,29–36 In a multicentre, intra-individual prospective study,35 MRI with gadoxetic acid showed superior characterisation of focal liver lesions compared to biphasic contrast-enhanced CT, results later backed by Hammerstingl et al.34 and Ichikawa et al.,36 who reported the superiority of MRI with gadoxetic acid compared to CT for the detection of lesions smaller than 1 and 2 cm in size respectively, although the limited number of patients with confirmed metastases in the second of the two studies meant the improvement in the detection of metastases by MRI with gadoxetic acid compared to CT could not be confirmed. Furthermore, compared with the diagnostic performance of 64-detector multidetector computed tomography (64-MDCT) and gadoxetic acid 3-T MRI, Scharitzer et al.33 concluded that gadoxetic acid-enhanced MRI should be the preferred choice in the preoperative setting, particularly for assessing small lesions. In terms of the superior clinical benefit of MRI with extracellular contrasts compared to CT, more data are necessary for a full evaluation.
Chen et al.37 summarise the diagnostic performance of MRI with gadoxetic acid in a meta-analysis. It included 13 publications with 1900 lesions, and evaluated the detection of liver metastases from colorectal cancer, in which a sensitivity of 93% and a specificity of 95% were reported.
Regarding the signal intensity shown by liver metastases, it should be noted that, although metastases do not take up gadoxetic acid because they lack hepatocyte activity and are typically hypointense in the hepatobiliary phase, retained gadoxetic acid uptake has been seen in breast cancer patients with intratumoral fibrosis, resulting in a target-like appearance in the hepatobiliary phase.38
Also important is the VALUE study, in which the group of patients in whom gadoxetic acid-enhanced MRI was used did not require additional diagnostic examinations, with it showing better diagnostic performance than contrast-enhanced CT and CT with extracellular contrasts.15
The combination of the hepatobiliary phase with gadoxetic acid and diffusion-weighted imaging provides the highest sensitivity for the preoperative diagnosis of liver metastases (PA: 100%). SeeTable 1.
The original recommendation20 was considered coherent, useful and relevant, and was contextualised by the expert group (Table S2, Supplementary material), based on their clinical experience and the following evidence.
MRI with gadoxetic acid shows greater sensitivity and positive predictive value for the preoperative period of patients with liver metastases from colorectal cancer (CRCLM)39 and is more sensitive than multidetector CT (MDCT) for the detection of histologically proven CRCLM, especially those less than 1 cm in size.33 In addition, the combination of MRI with gadoxetic acid with diffusion-weighted imaging seems to improve the detection of CRCLM compared to individual imaging techniques,29,33,40,41 particularly for small metastases,29–33,42 the conclusion being that MRI with a specific contrast agent can improve the assessment of small colorectal liver metastases.
Use of gadoxetic acid in the detection of liver metastases after chemotherapy treatmentAs chemotherapy can have effects on the liver parenchyma, the effectiveness of the use of different imaging techniques, as well as MRI with gadoxetic acid, in detecting metastases in patients who have been treated with chemotherapy needs to be assessed.
In the assessment of patients with liver metastases treated with chemotherapy, gadoxetic acid is of particular benefit in preoperative management (PA: 100%). SeeTable 1.
The original recommendation17 was considered coherent, useful and relevant, and was contextualised by the expert group (Appendix B Table S2, Supplementary material), based on their clinical experience and the following evidence.
In a meta-analysis, which included studies with contrast based on gadolinium, superparamagnetic iron oxides and gadoxetic acid, van Kessel et al.43 reported MRI to be the most sensitive and recommended technique for detecting metastatic lesions in patients who have had chemotherapy, and, more specifically, a prospective analysis by Berger-Kulemann et al. showed MRI with gadoxetic acid to be superior to 64-MDCT in the preoperative detection of colorectal liver metastases less than 1 cm in size in patients with fatty liver disease.44
In the assessment of patients treated with chemotherapy, when the differential diagnosis is between benign hepatocellular lesion and metastasis, the use of MRI with liver-specific contrast agents is recommended, particularly for detecting nodular hyperplasia (PA: 100%). See Table 3b:Table 1 (Section 3b).
The original recommendation18 was considered coherent, useful and relevant, and was contextualised by the expert group (Appendix B Table S2, Supplementary material), based on their judgement and clinical experience.
Several studies have demonstrated the importance of the use of MRI with gadoxetic acid in the detection, differentiation and understanding of the pathogenesis of benign hepatocellular nodules and nodular hyperplasia.45–47 However, there are still no studies to support the differences in sensitivity of MRI with liver-specific contrast agents in the detection of benign hepatocellular lesions vs metastasis. The contextualisation made in this recommendation is based primarily on the personal experience and clinical practice of the experts.
Despite the advantages of gadoxetic acid in the detection of liver metastases, there are also some limitations in its use, such as dyspnoea and transient respiratory distress, which can degrade the arterial phase of the dynamic study.48 This limitation can be minimised by performing multiple arterial phases.49 Furthermore, in patients with severe hepatic impairment, there may be a marked delay in obtaining images of the hepatobiliary phase, and it may even be impossible50; and in cases where hepatic haemangioma is strongly suspected, the behaviour of these lesions with gadoxetic acid may vary in the dynamic study with respect to extracellular contrast agents.51
In this project, we used an approach based on the adaptation and updating of international consensus documents, which is considered as a rigorous, valid and reproducible alternative methodology for obtaining clinical recommendations at a local level in less time and using fewer resources. The use of a non-systematic review to search for the starting documents and support for the modifications made to the recommendations, in addition to the lack of evaluation of the level of evidence, may be a limitation due to the risk of bias. Despite that, it was considered important to cultivate a systematic debate, in which, based on critical discussion, clinical experience and local knowledge provided by local experts and opinion leaders, we were able to shed light on the need to adapt international recommendations to a local level. In this context, the critical reflection carried out by local experts for the choice and contextualisation of the recommendations underlines the need to standardise decisions in routine clinical practice and to promote the generation of evidence on this subject at a national level.
ConclusionsThis document contains five recommendations for the use of MRI with gadoxetic acid aimed at helping and standardising decisions in routine clinical practice in Spain. The formulated recommendations have been contextualised based on the judgement and clinical experience of the experts, and supported by the evidence. The recommendations confirm the benefits of MRI with gadoxetic acid in the detection of liver metastases, aiding preoperative planning, particularly in the detection of lesions less than 1 cm in size, and facilitating the early diagnosis of metastatic spread.
Authorship- 1.
Responsible for the integrity of the study: RMLlO, ERB.
- 2.
Study concept: RMLlO, ERB.
- 3.
Study design: RMLlO, ERB.
- 4.
Data collection: JBG, NR, JMT, LC, JDF, MF, IV, ERB and RMLlO.
- 5.
Data analysis and interpretation: JBG, NR, JMT, LC, JDF, MF, IV, ERB and RMLlO.
- 6.
Statistical processing: N/A.
- 7.
Literature search: JBG, NR, JMT, LC, JDF, MF, IV, ERB and RMLlO.
- 8.
Drafting of the article: RMLlO, ERB.
- 9.
Critical review of the manuscript with intellectually significant contributions: JBG, NR, JMT, LC, JDF, MF, IV, ERB and RMLlO.
- 10.
Approval of the final version: JBG, NR, JMT, LC, JDF, MF, IV, ERB and RMLlO.
This article was funded by Bayer Hispania, S.L.
Conflicts of interestThe authors JBG, NR, JMT, LC, JDF, MF, IV, ERB and RMLlO declare having been paid fees by BAYER Hispania, S.L.
The authors express their gratitude to the company GOC Health Consulting for its methodological support throughout the process; to Bayer Hispania for its funding in editorial terms; and the hepatologist, Dr Ana Matilla, for her advisory role in this work.
Please cite this article as: Borrego Gómez J, Romera N, Tellado JM, del Campo L, Díaz Formoso J, Fuster M, et al. Recomendaciones de expertos sobre el uso de ácido gadoxético en pacientes con metástasis hepáticas en España. Radiología. 2022;64:300–309.