To study the clinical usefulness of ultrasound-guided alcohol sclerosis as a treatment alternative to surgical intervention for breast fistulas.
Material and methodsThis was a retrospective study of data collected in a hospital breast unit over a 3-year period (January 2011 through December 2013). The procedure consists of introducing a sclerosing solution into the lumen of the breast fistula under ultrasound guidance. All cases were reviewed by a multidisciplinary committee; patients were offered ultrasound-guided alcohol sclerosis as a first treatment option with surgical intervention as a rescue therapy for those with unsatisfactory outcomes.
ResultsTen fistulas were treated in 9 women (median age, 33 years; interquartile range 18.5 years). Five patients (50%) attributed the clinical findings to recurrent mastitis, four (40%) to a previous surgical intervention, and one (10%) to lactation. Seven patients (78%) were smokers. The procedure was well tolerated: nine patients (90%) rated the pain as one or 2 (mild pain) on a visual analog scale. There were no immediate complications. The response to treatment was considered excellent (absence of secretion and complete closure) in eight fistulas (80%).
ConclusionUltrasound-guided alcohol sclerosis achieved excellent outcomes in 80% of cases and is a viable alternative to surgical treatment.
Estudiar la utilidad clínica de la esclerosis con alcohol guiada con ecografía como tratamiento innovador y alternativo a la intervención quirúrgica de las fístulas de mama.
Material y métodosEstudio retrospectivo basado en los datos recogidos en una Unidad de mama hospitalaria durante tres años (enero de 2011 - diciembre de 2013). El procedimiento consistió en introducir en la luz de la fístula mamaria una solución esclerosante guiada con ecografía. Todos los casos fueron revisados por un comité multidisciplinar, se planteó a las pacientes la esclerosis con alcohol guiada con ecografía como primera opción terapéutica, dejando la intervención quirúrgica para los casos con resultados desfavorables.
ResultadosSe reunieron 10 fístulas en 9 mujeres. La mediana de edad fue de 33 años (rango intercuartílico 18.5 años). Cinco pacientes atribuyeron los datos clínicos a mastitis de repetición (50%), cuatro a una intervención quirúrgica previa (40%) y una a la lactancia (10%). Siete pacientes eran fumadoras (78%). El procedimiento se toleró bien, 9 pacientes (90%) puntuaron un valor de uno o 2 en la escala analógica visual del dolor (dolor leve). No hubo complicaciones inmediatas. La respuesta al tratamiento se consideró excelente (ausencia de secreción y cierre completo) en 8 fístulas (80%).
ConclusiónLa esclerosis con alcohol guiada con ecografía es una alternativa terapéutica a la quirúrgica que ha acabado con la curación del 80% de las fístulas tratadas.
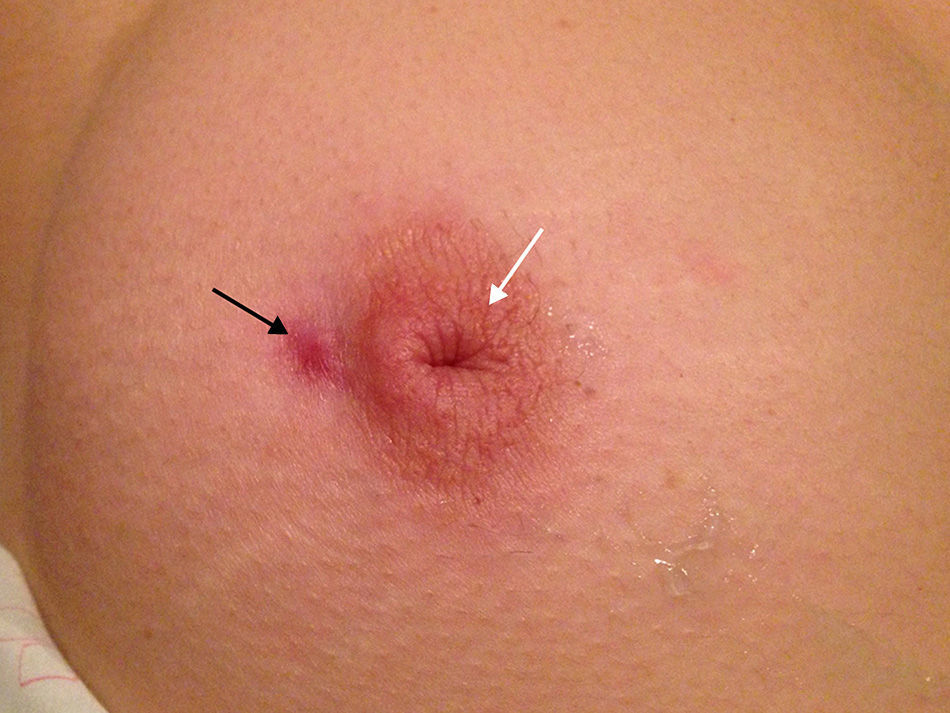
Breast fistulas, also known as Zuska's alteration, are a passage between one or several galactophorous ducts and the skin1; hence, its most frequent location is periareolar (Fig. 1). They can be single or multiple, unilateral or bilateral. Its origin is really uncertain,1,2 although they have been associated with previous surgical interventions of the breast and infectious or inflammatory processes such as mastitis and abscesses.2 They can also be related to the breastfeeding period3 and there is an obvious relation with smoking.4,5 The literature also describes the association with inflammatory intestinal diseases, stress, menstruation and clinical exacerbation in winter.6 The patient frequently presents with nipple inversion (Fig. 1) and, to a lesser degree, duct ectasia and abscesses.7 It generally affects young women in the ages ranging between 20 and 50.1–8 It is a process with great clinical repercussion, of torpid evolution and with a high recurrence rate8,9 whose treatment of choice has classically been surgery.7–11
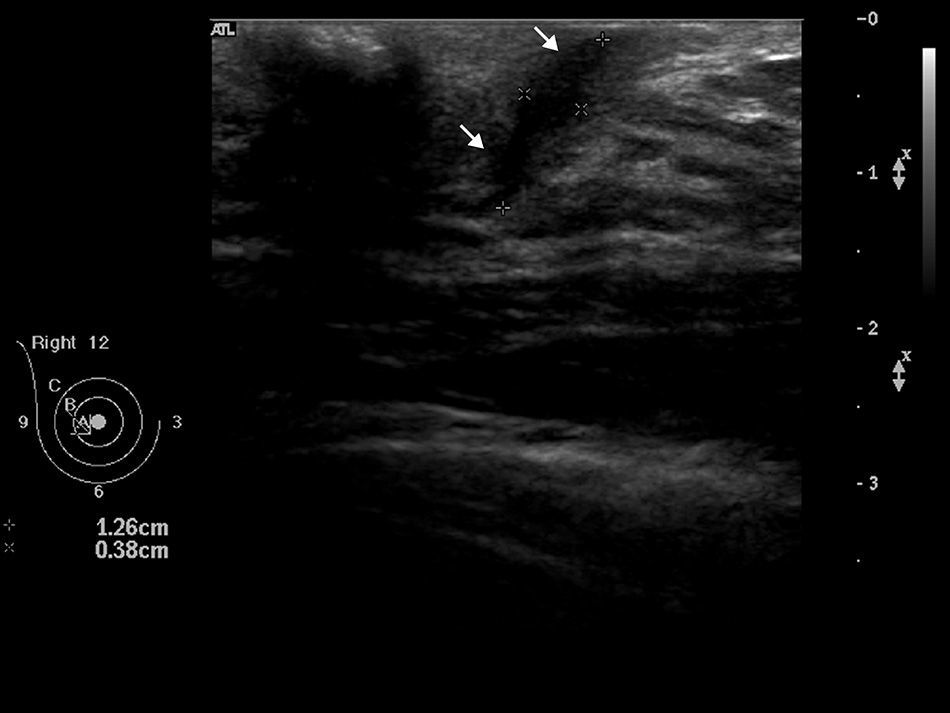
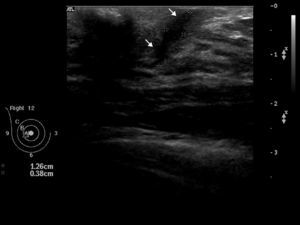
Our technique arises empirically after observing the benefits and good results of alcohol sclerotherapy in other type of processes in which it induced the formation of granulation tissue and the closure of cavities.12 In the past, the diagnostic modality of choice was fistulography, a technique that consisted in injecting contrast in the alveolar ducts and obtaining X-rays of both the aspect and distribution of ducts. Today it has been replaced by ultrasound12–15 which, due to its innocuousness, low cost and availability are more and more the most appropriate modality to visualize the fistulous trajectory (Fig. 2) and other associated alterations such as surrounding edema, duct ectasia and collections.
The goal of our work is to study the clinical usefulness of ultrasound-guided alcohol sclerosis–one innovative and alternative therapy to surgery in breast fistulas.
Material and methodsWe conducted a retrospective study of a series of cases from the Radiology Service Breast Unit of our institution over a period of 3 years, between January, 2011 and December, 2013. The study was approved by the hospital ethics committee. In the study we included data from all breast fistulas diagnosed and treated through ultrasound-guided alcohol sclerosis, a total of 10. In the course of the study one fistula was diagnosed that was not treated. It belonged to a patient with a paraareolar skin lesion who did not present suppuration. The ultrasound identified a closed fistulous trajectory in the skin surface; so it was not eligible to undergo percutaneous treatment with alcohol at that moment. All cases were reviewed by the Breast Unit Multidisciplinary Committee that proposed the ultrasound-guided alcohol sclerosis to the patients as the first therapeutic option. The general contraindications were those of all interventional procedures: refusal of consent, coagulation disorders and known allergic reactions, and those typical of alcohol sclerosis: inflammation, skin infection or abscesses, acute pain and complete closure of fistula since it would lead to a new suppuration.
The variables gathered in each patient included age, sex, tobacco use, number of fistulas, location, time of evolution, nipple inversion, clinical exacerbation with menstruation, stress or season of the year and a history of mastitis, surgical intervention and breastfeeding. Similarly, the length and thickness of the fistulous trajectory was measured in the presence of abscesses and duct ectasia. When it comes to the procedure, the quantity of sclerosing material permitted, the number of injections, the Visual Analog Pain Scale and the complications were written down. Evolutionary data such as persistence of symptoms, new treatments (number of procedures) and clinical and ultrasound response were also gathered, classified into poor (persistence of secretion and incomplete closure of the fistula), good (minimal secretion and incomplete closure of the fistula) and excellent (no secretion and complete closure of the fistula).
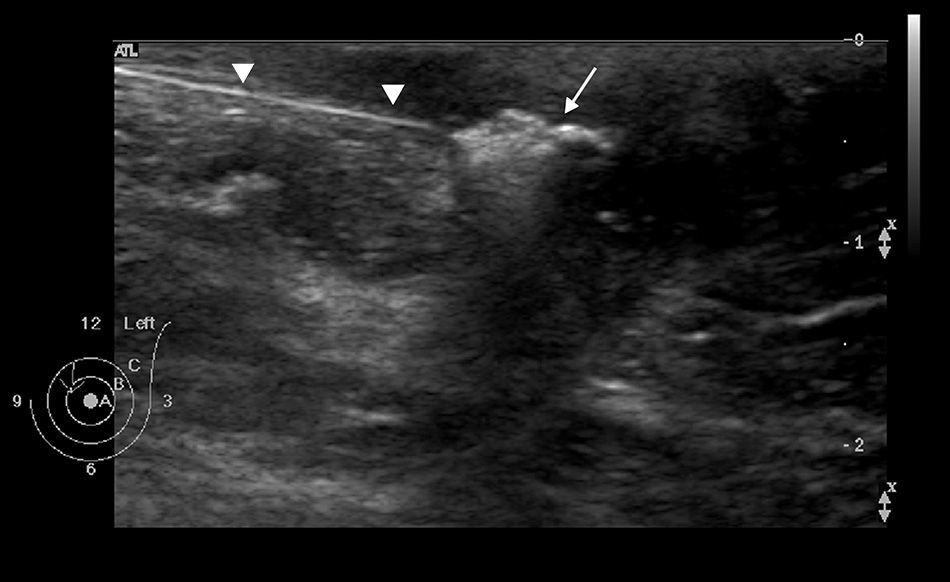
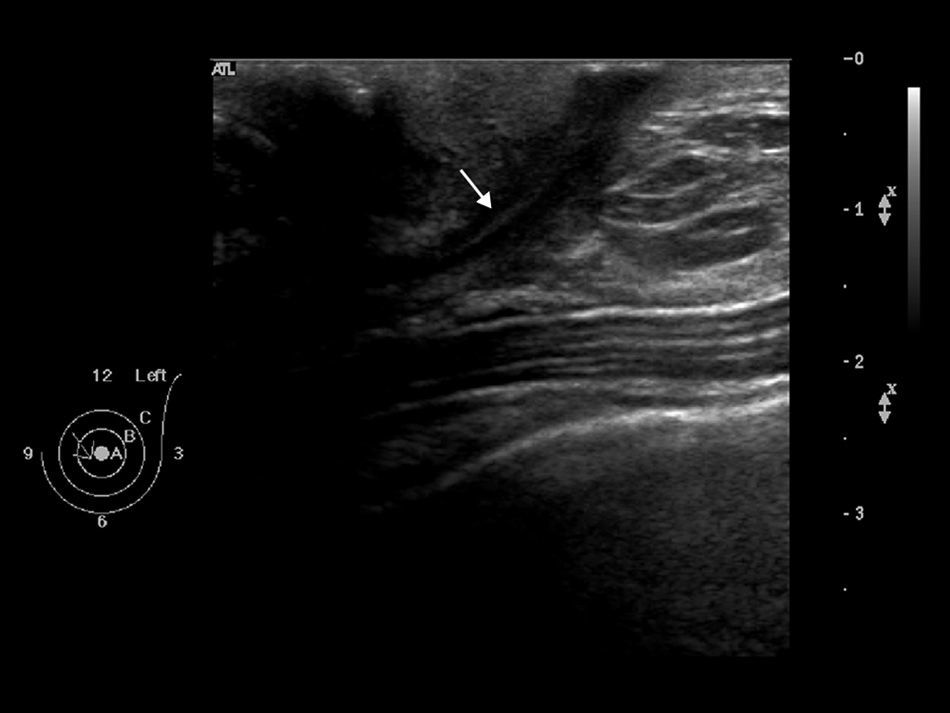
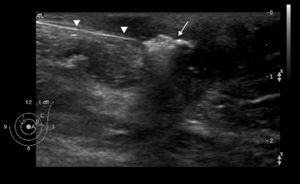
All studies were conducted by the same radiologist in conditions of asepsis. In all of them the patients’ coagulation analyses and history of allergic reaction were checked and written informed consent obtained. There were no contraindicated cases. The procedure began with a routine examination of both breasts and the axillary region. Once the fistula had been identified, it was studied thoroughly with a 7–12MHz linear ultrasound probe (Philips HDI 5000 SonoCT, Eindhoven, Holland), to determine the location, number, shape, vascularization and dimensions and reference measurements were taken of the length and width for further comparison in subsequent controls. After cleaning and disinfecting the area where the fistula was located, an 18G intramuscular needle was inserted connected to a syringe loaded with 5ml of pure alcohol diluted at 50% with local anesthesia (mepivacaine 2%; B. Braun Medical, Bethlehem, PA, EE.UU.). The content was injected retrogradely, from the distal to the proximal end (Fig. 3). The whole procedure was ultrasound-guided, so it was possible to observe in real time how the echogenicity of the fistula was modified as the solution was injected (Fig. 4). Tolerance to the procedure was classified through the Analogical Visual Pain Scale assigning the values of: 0 no pain, 1–2 light pain, 3–7 moderate pain, 8–9 acute pain and 10 maximum imaginable pain.
Aspect of left breast immediately after alcohol sclerosis in a 32-year-old patient showing an inner paraareolar fistula with 3 years of evolution. A retrograde puncture was performed (black arrow) in which the injected solution filled the fistula lumen, suppurated outwards (arrow head) and accumulated in a superficial collection (star). The nipple is inverted (white arrow).
Upon finishing, it was recommended immobilizing the corresponding upper limb for 24h and not touching the puncture area to prevent forced suppuration. Patients were recommended to take an oral painkiller or anti-inflammatory medication upon request in case they presented discomfort once the effect of the local anesthetic wore off. Drugs with anti-aggregating action were contraindicated for 24h to prevent the appearance of hematomas in the puncture area. Prophylactic antibiotics were not necessary. Patients were explained that a hematoma could appear in the treated area and that, in case fever or a lump appeared, they should go to the Emergency Services.
The clinical and ultrasound controls were carried out 15 days after the procedure, and then 3 and 6 months later. The subsequent controls depended on the patient's clinical data. Once the period of ultrasound controls had passed, the Surgery Service conducted a clinical follow-up that discharged the patients once healed. In the successive controls the echogenicity of the fistula lumen and the fistula measurements with respect to the dimensions prior to the procedure (Fig. 5) was taken into account. Alcohol sclerosis was repeated as many times as it was tolerated in all cases when the patient would not have a favorable clinical and ultrasound response.
The variables collected were introduced into a Microsoft Excel spreadsheet and the data analyzed using the statistical SPSS software version 19.0 for Windows (SPSS Inc, Chicago, IL, U.S.A.). The qualitative variables were described as absolute number and percentage and the quantitative ones as median and interquartile range as it was a sample of non-normal distribution due to its reduced number.
Results10 fistulas were identified in 9 women. The median age was 33 years with an interquartile range of 18.5 years. The median time of clinical evolution was 24 months (interquartile range, 30 months). In all the cases the fistulous trajectory was identified in the ultrasound examination, the smallest was 8mm×0.7mm and the largest one 29mm×5.2mm. Five patients (50%) attributed the lesion to repeated mastitis, 4 (40%) to a previous surgical intervention and one (10%) to breastfeeding. Seventy eight per cent of patients suffered clinical exacerbation in winter and the remaining 22% in spring. In 3 patients (33%) the symptoms were associated with menstruation, in 2 (22%) with situations of stress and 4 (45%) they did not describe any association. Seven patients (78%) were smokers. In 4 patients (45%) their nipple was inverted. Lesions were more frequent in the right breast (70%) and in the internal paraareolar position (80%). In all cases the sclerosis was performed with a single injection. In the first session, the quantity of alcohol introduced was one or two ml in 6 cases, however, 4 fistulas required up to 4ml. There were no immediate complications. The procedure was well-tolerated in almost all cases (9 out of 10 patients scored one or 2 in the visual analogical pain scale) and only one patient regarded it as moderate pain (value 7). The response to the treatment was excellent (absence of secretion and complete closure) in 8 (80%) fistulas. Three (37.5%) of them closed after only one sclerosis procedure, another 3 required 2 injections and in 2 cases more than 3 procedures were necessary. Follow-up time ranged from a minimum of 6 months to a maximum of 3 years. During that time none of them relapsed. In the two fistulas that did not close completely (followed up until today, 6 and 7 months of evolution from the last sclerosis procedure, respectively), the response was classified as good, with a decrease of secretion but without complete ultrasound closure, in one fistula after four procedures and in the other fistula after five procedures. They are both on ultrasound controls and have not been referred to the surgery services.
DiscussionIn our patients treated with alcohol in the fistula lumen using an ultrasound-guided percutaneous procedure the responses were excellent in 80% of the cases.
The ultrasound allowed us to identify fistulas in all cases, characterize the fistulous trajectory, assess the associated complications and perform the sclerosis procedure in real time. It was not necessary to undertake any other type of complementary imaging tests to diagnose or treat them. Magnetic resonance, especially with a contrast agent, is more sensitive than ultrasound for the detection of impalpable mammary masses and diagnose alterations located beneath the nipple-areolar complex such as abscesses and fistulas that sit in peri-areolar location.16,17 However because there were no limitations to diagnose and treat the fistulas with ultrasound and due to the scarce availability of magnetic resonance we did not think of conducting the study with such modality.
The procedure was uncomfortable but bearable and all patients preferred closing the fistula through sclerotherapy than having surgery even if they had to undergo several sessions. The main complications after the percutaneous procedure are local pain and inflammation and in rare cases the infection of puncture site. That is why it was not considered necessary to use antibiotics prophylactically. In our study there were no immediate complications. After the surgical intervention we can see complications associated with the procedure following the incision, manipulation and closure with suture.7,10 The clinical and ultrasound results of our study have been optimal (excellent responses in 80% of the cases) which in addition to how good this modality was tolerated, its few complications and low cost make the procedure a real therapeutic alternative to surgery.
The main limitation of our study is that it is a series of cases and it has not been possible to compare the percutaneous therapy with the surgical one. Another relevant limitation is the small number of patients. This is why we need to increase the sample and compare the percutaneous modality with the surgical one to be able to confirm these results.
In sun ultrasound-guided alcohol sclerosis can be a therapeutic alternative to surgical intervention for the management of breast fistulas.
Ethical responsibilitiesProtection of people and animalsAuthors declare that the proceedings followed abide by the ethical regulations of the corresponding human experimentation committee and the World Health Organization and the Helsinki Declaration.
Data confidentialityAuthors claim that they have followed the protocols of their institutions on the publication of data from patients.
Right to privacy and informed consentAuthors have obtained the prior written informed consent from patients and/or individuals aforementioned in this article. This paper is in possession of the corresponding author.
Authors’ contributions- 1.
Manager of the integrity of the study: AMFM, LLG.
- 2.
Original Idea of the Study: AMFM, LLG.
- 3.
Study design: AMFM, LLG, GSL.
- 4.
Data mining: AMFM, LLG, GSL, IAS, TCM.
- 5.
Data analysis and interpretation: AMFM, GSL, IAS, TCM.
- 6.
Statistical analysis: AMFM, GSL.
- 7.
Reference search: AMFM, LLG, IAS, TCM
- 8.
Writing: AMFM, LLG.
- 9.
Critical review of the manuscript with intellectually relevant remarks: AMFM, LLG, GSL, IAS, TCM.
- 10.
Approval of final version: AMFM, LLG, GSL, IAS, TCM.
Authors declare no conflict of interests.
Please cite this article as: Fernández Martínez AM, López González L, Santana-Lopez G, Álvarez Silva I, Cuesta Marcos T. Utilidad clínica de la esclerosis con alcohol guiada con ecografía en pacientes con fístulas de mama. Radiología. 2015;57:321–325.