Transient loss of consciousness (TLoC) is a symptom that has several differential etiologic diagnosis, causes significant morbidity and mortality with impact on quality of life.
ObjectiveThe purpose of this study was to access the diagnosis and prognosis of these patients admitted in a Portuguese University Hospital.
MethodsThe study included 125 patients with TLoC admitted in the emergency room and then admitted to the hospital during the year 2013. Patients were contacted by phone for follow-up evaluations, during the 18 months from the date of admission.
ResultsCardiogenic syncope was the most common etiology of TLoC (39.2%). The 18-month overall mortality was 11.2%, however this was higher in patients with unexplained TLoC, with an 18-month mortality of 27.8% (p=0.031); It was found that half of patients who died, did so in the first month from admission date; 20% of patients had recurrent episodes of TLoC (mean number of 5.6 episodes), with a higher percentage of recurrence occurring in patients with reflex syncope (35.3%; p=0.023). 60% of patients with recurrent episodes suffered accidents and/or injuries, and 20% of recurrence patients gave up driving (p=0.019).
ConclusionThe results obtained highlight the burden of TLoC in terms of morbidity and mortality, similar results to those previously published, except for the prevalence of the etiology, cause of death and recurrence's etiology of TLoC. This study emphasizes the significant implications that TLoC leads on morbidity and mortality being essential its accurate diagnosis.
Transient loss of consciousness (TLoC) is a frequent manifestation in the general population. An estimated 6.2/1000 person-years have syncope,1 constituting a significant reason for admission in the Emergency Department (ED) and subsequent hospitalization. TLoC cases correspond to 0.6–1.2% of visits to the ED2–4 and 6% of hospital admissions.5
TLoC can occur in benign situations, such as reflex syncope1,6; it may be a manifestation of a disease with origin in the central nervous system (CNS), such as epilepsy or cerebrovascular disease6–9; or may be a symptom of cardiac disease, associated with a high mortality risk and increased incidence of sudden death.1,6,10–12
Recurrent episodes of TLoC carries significant morbidity,6,11–13 increased need of medical care2,14–16 and determine significant changes in quality of life.17,18
Because it is a public health problem with high frequency and variable risk of mortality and morbidity, it is important to establish the correct diagnosis and prognosis of patients with TLoC.
Little is known about the diagnosis and specially the prognosis of Portuguese patients with TLoC. Therefore, this study aimed to evaluate the diagnosis and prognosis over 18 months in patients with different causes of TLoC, assessing mortality, recurrence episodes of TLoC, injuries and traffic accidents associated with recurrent episodes, limitation of driving and the impact on quality of life.
MethodsTLoC is defined as a rapid onset, short duration loss of consciousness that occurs transiently and with spontaneous recovery. TLoC may occur due to several traumatic and non-traumatic causes, including: syncope, epilepsy and psychogenic pseudosyncope, among others.7
Syncope is defined as a sudden loss of consciousness due to transient global cerebral hypoperfusion characterized by rapid onset, short duration and spontaneous complete recovery.7,19 Syncope is associated to an inability to maintain postural tone. Therefore, it is not compatible with seizures, vertigo, dizziness, coma, shock or other states of altered consciousness10
We selected all patients with 18 years or more of age who were admitted consecutively in the ED of a university hospital during the year 2013 with TLoC and who were admitted in this hospital. This was considered the TLoC index episode. We reviewed the clinical data from the ED and inpatient and outpatient records of all patients selected for this study. The determination of TLoC etiology was based on the attributable cause considered by the physicians that observed the patient in the ED, during hospitalization and in the outpatient visits, after evaluation of diagnostic tests. 156 patients were included in this study, with the causes of TLoC classified in 6 groups: reflex syncope (includes neurocardiogenic and situational syncope and carotid sinus hypersensitivity), cardiogenic syncope (structural or arrhythmic), syncope due to orthostatic hypotension, TLoC with CNS origin (including epilepsy and cerebrovascular diseases), psychogenic pseudosyncope and unexplained TLoC.
Patient follow-up was obtained through clinical records and telephone contact with patients or relatives/caregivers. This information was gathered between July and August of 2015. We collected information regarding mortality, recurrent episodes of TLoC, consequences of new episodes, medical care and new hospitalization for TLoC. Mortality data was obtained by hospital process of the patient and by the information given by relatives/caregivers. Death certificates and autopsy reports were not evaluated. Furthermore we collected information about limitation on driving and the impact of TLoC in quality of life. Quality of life assessment was made through telephone contact asking the patient to define his quality of life in better, equal or worse in relation to the impact of TLoC in their lives. Follow-up corresponds to the period between the date of hospital admission for the TLoC index episode in 2013 to 18 months after, for each patient. Relatives or caregivers of patients who died during hospitalization from the index episode were not contacted with the information being obtained from clinical records.
We excluded patients who refused to participate, patients unable of giving the pretended information and patients, relatives/caregivers that could not be contacted by telephone.
This research was conducted in a university hospital and approved by the Ethics Committee for Health of the Hospital. All patients contacted by telephone were asked for their consent.
Data was analyzed using IBM SPSS 22.0. The qualitative variables are presented through frequency tables and the quantitative variables are presented by the mean, standard deviation, minimum and maximum values. Chi-square test and t-Student test were used for statistical analysis. Values were considered statistically significant at a 95% confidence interval (p-value: p<0.05).
ResultsThis study selection included 156 patients. However, we were unable to contact 31 of these patients (19.9%): 24 because it was not possible to contact them by telephone (77.4%) and 7 for refusal (22.6%). Of patients excluded, 14 were women (45.2%), 17 men (54.8%) with a mean age of 72 years (±14).
For analysis and in total were included in the study 125 patients (80.1%), whose follow-up was assessed from admission date up to 18 months after. Fifty-one patients were women (40.8%), 74 men (59.2%), the mean age was 70 years (±15) and ranged from 18 years up to 96 years.
Regarding the service where they remained hospitalized during the TLoC index episode, 65 patients were admitted in internal medicine (52.0%), 43 in cardiology (34.4%), 8 in neurology (6.4%), 5 in surgery (4%) and the remaining 4 patients in intensive/neurocritical care (3.2%). The average stay for the TLoC index episode was 11 days (±11.1), a median of 7 days, with the range varying between 1 day and a maximum of 74 days.
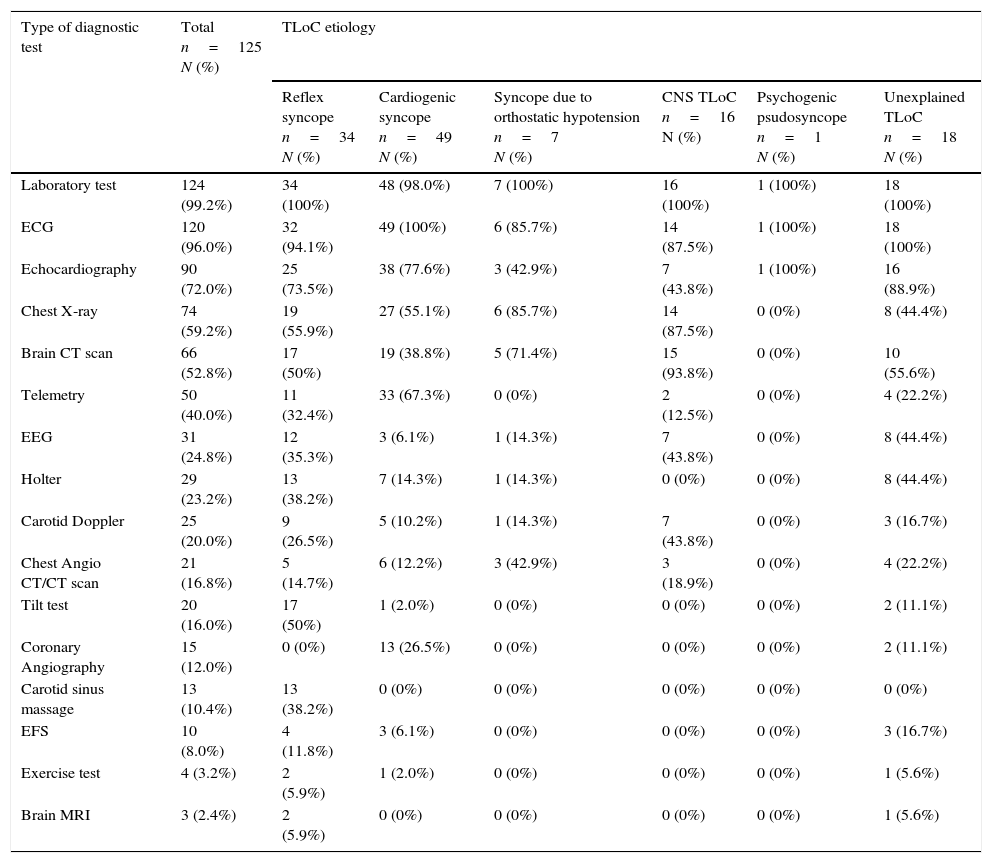
Regarding diagnostic tests performed, due to the TLoC index episode (Table 1), 99.2% of patients underwent Laboratory test (hemogram, kidney and renal function, electrolytes, C-reactive protein and myocardial necrosis markers, in some) an initial Electrocardiogram (ECG) was performed in 96% of patients (in those 9.2% had third-degree atrioventricular (AV) block and 2.5% had Mobitz II AV block, echocardiography in 72% (43.3% with changes), Chest X-ray in 59.2%, brain computerized tomography (CT) scan in 52.8% (30.3% with changes), Telemetry in 40% (44% with changes), Electroencephalogram in 24.8% (29% with changes), Holter in 23.2% (Mobitz II AV block in 6.9%), Carotid Doppler in 20% (changes in 20%), chest Angio-CT and/or chest CT in 16.8% (33.3% with changes), Tilt test in 16% (positive and with TLoC reproduction in 55%), Coronary Angiography in 12% (changes in 53.3%), Carotid sinus massage in 10.4% (positive in 23.1%), Electrophysiological study in 8% (changes in 30%), Exercise test in 3.2% (25% with changes) and brain Magnetic Resonance Imaging in 2.4%.
Diagnostic tests performed for the TLoC index episode (total and by TLoC etiology).
| Type of diagnostic test | Total n=125 N (%) | TLoC etiology | |||||
|---|---|---|---|---|---|---|---|
| Reflex syncope n=34 N (%) | Cardiogenic syncope n=49 N (%) | Syncope due to orthostatic hypotension n=7 N (%) | CNS TLoC n=16 N (%) | Psychogenic psudosyncope n=1 N (%) | Unexplained TLoC n=18 N (%) | ||
| Laboratory test | 124 (99.2%) | 34 (100%) | 48 (98.0%) | 7 (100%) | 16 (100%) | 1 (100%) | 18 (100%) |
| ECG | 120 (96.0%) | 32 (94.1%) | 49 (100%) | 6 (85.7%) | 14 (87.5%) | 1 (100%) | 18 (100%) |
| Echocardiography | 90 (72.0%) | 25 (73.5%) | 38 (77.6%) | 3 (42.9%) | 7 (43.8%) | 1 (100%) | 16 (88.9%) |
| Chest X-ray | 74 (59.2%) | 19 (55.9%) | 27 (55.1%) | 6 (85.7%) | 14 (87.5%) | 0 (0%) | 8 (44.4%) |
| Brain CT scan | 66 (52.8%) | 17 (50%) | 19 (38.8%) | 5 (71.4%) | 15 (93.8%) | 0 (0%) | 10 (55.6%) |
| Telemetry | 50 (40.0%) | 11 (32.4%) | 33 (67.3%) | 0 (0%) | 2 (12.5%) | 0 (0%) | 4 (22.2%) |
| EEG | 31 (24.8%) | 12 (35.3%) | 3 (6.1%) | 1 (14.3%) | 7 (43.8%) | 0 (0%) | 8 (44.4%) |
| Holter | 29 (23.2%) | 13 (38.2%) | 7 (14.3%) | 1 (14.3%) | 0 (0%) | 0 (0%) | 8 (44.4%) |
| Carotid Doppler | 25 (20.0%) | 9 (26.5%) | 5 (10.2%) | 1 (14.3%) | 7 (43.8%) | 0 (0%) | 3 (16.7%) |
| Chest Angio CT/CT scan | 21 (16.8%) | 5 (14.7%) | 6 (12.2%) | 3 (42.9%) | 3 (18.9%) | 0 (0%) | 4 (22.2%) |
| Tilt test | 20 (16.0%) | 17 (50%) | 1 (2.0%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (11.1%) |
| Coronary Angiography | 15 (12.0%) | 0 (0%) | 13 (26.5%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (11.1%) |
| Carotid sinus massage | 13 (10.4%) | 13 (38.2%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| EFS | 10 (8.0%) | 4 (11.8%) | 3 (6.1%) | 0 (0%) | 0 (0%) | 0 (0%) | 3 (16.7%) |
| Exercise test | 4 (3.2%) | 2 (5.9%) | 1 (2.0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (5.6%) |
| Brain MRI | 3 (2.4%) | 2 (5.9%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (5.6%) |
CNS, central nervous system; CT, computed tomography; ECG, Electrocardiogram; EEG, Electroencephalogram; EFS, Electrophysiological study; MRI, Magnetic resonance; TLoC, Transient loss of consciousness.
Although 4% of all patients were not submitted to an initial evaluation in the emergency room, all patients with unexplained TLoC were evaluated with an ECG (Table 1).
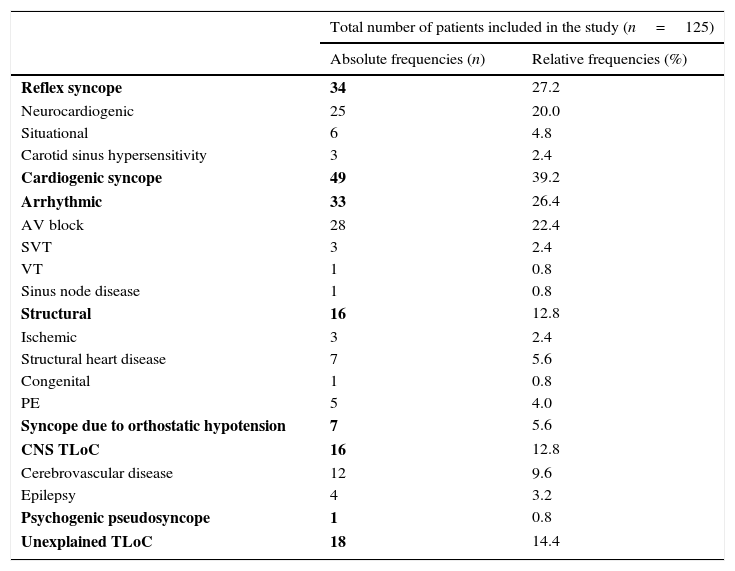
The most frequent etiology of TLoC was cardiogenic syncope (39.2%), reflex syncope corresponded to 27.2% of patients and psychogenic pseudosyncope was the least frequent etiology (0.8%) (Table 2).
Etiology of TLoC.
| Total number of patients included in the study (n=125) | ||
|---|---|---|
| Absolute frequencies (n) | Relative frequencies (%) | |
| Reflex syncope | 34 | 27.2 |
| Neurocardiogenic | 25 | 20.0 |
| Situational | 6 | 4.8 |
| Carotid sinus hypersensitivity | 3 | 2.4 |
| Cardiogenic syncope | 49 | 39.2 |
| Arrhythmic | 33 | 26.4 |
| AV block | 28 | 22.4 |
| SVT | 3 | 2.4 |
| VT | 1 | 0.8 |
| Sinus node disease | 1 | 0.8 |
| Structural | 16 | 12.8 |
| Ischemic | 3 | 2.4 |
| Structural heart disease | 7 | 5.6 |
| Congenital | 1 | 0.8 |
| PE | 5 | 4.0 |
| Syncope due to orthostatic hypotension | 7 | 5.6 |
| CNS TLoC | 16 | 12.8 |
| Cerebrovascular disease | 12 | 9.6 |
| Epilepsy | 4 | 3.2 |
| Psychogenic pseudosyncope | 1 | 0.8 |
| Unexplained TLoC | 18 | 14.4 |
AV, atrioventricular; CNS, central nervous system; PE, pulmonary embolism; SVT, supraventricular tachyarrhythmias; TLoC, transient loss of consciousness; VT, ventricular tachyarrhythmias.
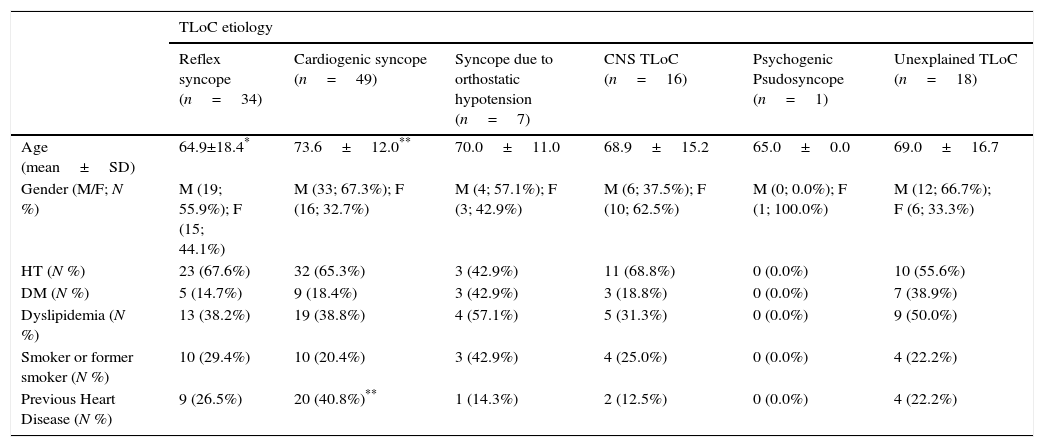
We can concluded through the comparative analysis of the different etiological groups of TLoC, that there are statistically significant differences in age by some etiologies, including those who had reflex syncope had a significantly lower mean age (p=0.044) compared to other causes of TLoC and who had cardiogenic syncope had a significantly higher mean age (p=0.030) compared to patients without this diagnosis. There is a significant relationship (p=0.025) between previous heart disease and cardiogenic syncope, being that 40.8% of those who had cardiogenic syncope show heart disease (Table 3).
Demographic characteristics, cardiovascular risk factors and previous heart disease by etiology of TLoC.
| TLoC etiology | ||||||
|---|---|---|---|---|---|---|
| Reflex syncope (n=34) | Cardiogenic syncope (n=49) | Syncope due to orthostatic hypotension (n=7) | CNS TLoC (n=16) | Psychogenic Psudosyncope (n=1) | Unexplained TLoC (n=18) | |
| Age (mean±SD) | 64.9±18.4* | 73.6±12.0** | 70.0±11.0 | 68.9±15.2 | 65.0±0.0 | 69.0±16.7 |
| Gender (M/F; N %) | M (19; 55.9%); F (15; 44.1%) | M (33; 67.3%); F (16; 32.7%) | M (4; 57.1%); F (3; 42.9%) | M (6; 37.5%); F (10; 62.5%) | M (0; 0.0%); F (1; 100.0%) | M (12; 66.7%); F (6; 33.3%) |
| HT (N %) | 23 (67.6%) | 32 (65.3%) | 3 (42.9%) | 11 (68.8%) | 0 (0.0%) | 10 (55.6%) |
| DM (N %) | 5 (14.7%) | 9 (18.4%) | 3 (42.9%) | 3 (18.8%) | 0 (0.0%) | 7 (38.9%) |
| Dyslipidemia (N %) | 13 (38.2%) | 19 (38.8%) | 4 (57.1%) | 5 (31.3%) | 0 (0.0%) | 9 (50.0%) |
| Smoker or former smoker (N %) | 10 (29.4%) | 10 (20.4%) | 3 (42.9%) | 4 (25.0%) | 0 (0.0%) | 4 (22.2%) |
| Previous Heart Disease (N %) | 9 (26.5%) | 20 (40.8%)** | 1 (14.3%) | 2 (12.5%) | 0 (0.0%) | 4 (22.2%) |
CNS, Central nervous system; DM, diabetes mellitus; F, female; H, hypertension; M, male; SD, standard deviation; TLoC, transient loss of consciousness.
Regarding the 31 patients that were excluded from the study, the most common TLoC etiology was also cardiogenic syncope (32.3%), however, contrary to what happened with the patients included in the study, unexplained TLoC was the second most frequent etiology (25.8%), followed by reflex syncope (22.6%) and CNS TLoC (16.1%). One patient had psychogenic pseudosyncope (3.2%) and none had syncope due to orthostatic hypotension.
MortalityFourteen patients died (11.2%). Of these, 5 patients (35.7%) died during hospitalization for the TLoC index episode. Six patients were women (42.9%) and 8 were men (57.1%). The mean age was 80±11 years, ranging between 61 and 96 years. 42.9% had previous heart disease. The average time since admission by the TLoC index episode until death was 5.8±5.9 months, though half of the subjects (7) died within the first month from the date of admission to the TLoC index episode. Five patients died between the first month and 12th month (35.7%) and the remaining 2 patients died between months 12 and 18 from the date of admission (14.3%).
Of the 5 patients who died during hospitalization for the index episode of TLoC, 2 patients had cardiogenic syncope, 2 unexplained TLoC and 1 CNS TLoC.
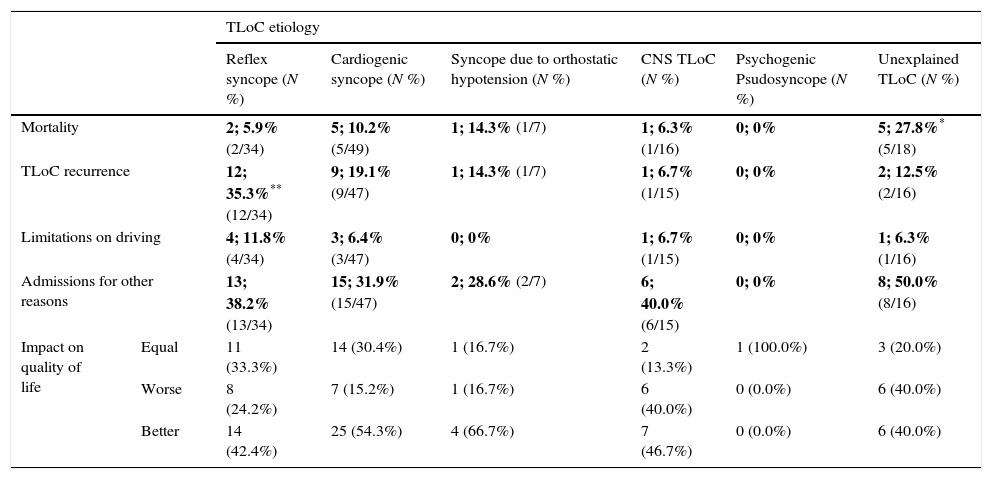
In relation to the total of patients with unexplained TLoC (18 patients), 5 of these died (27.8%) and there is a significant relationship (p=0.031) between this unknown etiology and mortality (Table 4).
Mortality, recurrence of TLoC, limitations on driving, admissions for other reasons and impact on quality of life by etiology of TLoC.
| TLoC etiology | |||||||
|---|---|---|---|---|---|---|---|
| Reflex syncope (N %) | Cardiogenic syncope (N %) | Syncope due to orthostatic hypotension (N %) | CNS TLoC (N %) | Psychogenic Psudosyncope (N %) | Unexplained TLoC (N %) | ||
| Mortality | 2; 5.9% (2/34) | 5; 10.2% (5/49) | 1; 14.3% (1/7) | 1; 6.3% (1/16) | 0; 0% | 5; 27.8%* (5/18) | |
| TLoC recurrence | 12; 35.3%** (12/34) | 9; 19.1% (9/47) | 1; 14.3% (1/7) | 1; 6.7% (1/15) | 0; 0% | 2; 12.5% (2/16) | |
| Limitations on driving | 4; 11.8% (4/34) | 3; 6.4% (3/47) | 0; 0% | 1; 6.7% (1/15) | 0; 0% | 1; 6.3% (1/16) | |
| Admissions for other reasons | 13; 38.2% (13/34) | 15; 31.9% (15/47) | 2; 28.6% (2/7) | 6; 40.0% (6/15) | 0; 0% | 8; 50.0% (8/16) | |
| Impact on quality of life | Equal | 11 (33.3%) | 14 (30.4%) | 1 (16.7%) | 2 (13.3%) | 1 (100.0%) | 3 (20.0%) |
| Worse | 8 (24.2%) | 7 (15.2%) | 1 (16.7%) | 6 (40.0%) | 0 (0.0%) | 6 (40.0%) | |
| Better | 14 (42.4%) | 25 (54.3%) | 4 (66.7%) | 7 (46.7%) | 0 (0.0%) | 6 (40.0%) | |
CNS, central nervous system; TLoC, transient loss of consciousness.
The cause of death could be established in nearly all patients (13 patients; 92.9%). Four patients (28.6%) died of cardiorespiratory arrest, 3 (21.4%) of stroke, 2 (14.3%) with acute myocardial infarction and the remaining patients (4 patients; 28.6%) died due to cardiogenic shock, adenocarcinoma of cardia/distal esophagus with liver metastasis, acute rejection from prior cardiac transplantation complicated by decompensated congestive heart failure, and complete AV block that resulted in Cranioencephalic trauma (CET), Subdural Hemorrhage (SH) with secondary intracranial hypertension.
The causes of death of the 5 patients with unexplained TLoC were stroke, cardiogenic shock, acute rejection from prior cardiac transplantation complicated by decompensated congestive heart failure and cardiorespiratory arrest (2 patients).
For patients who died during follow-up period (excluding those who died during hospitalization at index episode), 3 presented new episodes of TLoC before death (33.3%). The average number of new episodes was 5.3 (±5.9) and have a mean time from admission to recurrence of 5.3 months. One patient with cardiogenic syncope had 12 recurrent TLoC episodes before he died. For this patients who died during the follow-up period and had recurrences all were driven to the hospital.
Recurrence of TLoCRecurrence of TLoC after the index episode was 20% (25 patients). The mean number of new episodes was 5.6 (±6.7) and the median was 3 and ranged between 1 and 31 new episodes.
Patients with TLoC recurrence had an average of 69±15 years. Of these 7 were female (28%) and 18 male (72%) and 32% had previous heart disease.
Seven patients experienced only one episode of TLoC (28%). Eight patients had 2–4 (32%), 4 patients between 5 and 10 (16%) and the remaining 6 patients had more than 10 recurrent episodes of TLoC (24%).
The average time from admission date to the first recurrent episode of TLoC was 4.5±5.1 months, though 10 patients had the first episode of TLoC in the first month since the date of admission (40%), 9 patients between the first month until one year from the date of admission (36%) and 4 patients from one year to 18 months (16%). In two patients has not been possible to establish the time of the first episode (8%).
In Table 4 are present the recurrence rates by TLoC etiology, excluding patients who died during hospitalization for the index episode. Patients with reflex syncope had a higher recurrence rate (35.3%) compared to patients without these etiology of TLoC (p=0.023).
Twenty-two patients (88%) resorted to medical care because of new episodes of TLoC. Of those, 6 patients (27.3%) were re-admitted. The average number of hospitalizations was 1.5 (±0.8). Four patients had one new hospitalization for new episode of TLoC, one was hospitalized for two times and another patient was hospitalized three times due to new episodes of TLoC. The average time of readmission was 13.7 days ±9.9, ranging between 3 and 30 days.
Injuries and accidents associated with episodes of TLoC recurrenceIn patients with recurrence of TLoC, 15 patients (60%) had injuries and/or accidents. Of these, 3 patients (20%) had mild CET, 2 (13.3%) SH and other 2 (13.3%) significant fractures. In addition, 11 patients (73.3%) had falls and 8 patients (53.3%) hematomas.
Two patients (8%) had traffic accidents due to recurrent episodes of TLoC.
Of these 15 patients with injuries or accidents almost half (46.7%) had reflex syncope (7 patients), 5 had cardiogenic syncope (33.3%), 2 unexplained TLoC (13.3%) and 1 CNS TLoC (6.7%).
Although all patients with CNS and unexplained TLoC that had recurrence presented injuries/accidents associated with the recurrence of TLoC, there was no statistically significant relationship between the etiology of TLoC and injuries/accidents due to recurrence.
Limitation of drivingNine patients (7.2%) had to quit driving completely or for a prolonged period of time, due to the index episode or new episodes of TLoC. Five of these had recurrent episodes of TLoC and the remaining 4 had no recurrence. It was found that 20% of patients with new episodes of TLoC had their vehicles use limited, with the relationship between the recurrence of TLoC and limitation of driving being significant (p=0.019).
Table 4 presents the patients with limitation of driving, by etiology of TLoC (excluding patients who died during hospitalization for the index episode). Among patients with reflex syncope, 4 (11.8%) reported limitation of driving, among patients with cardiogenic syncope were 3 (6.4%) and between patients with CNS and unexplained TLoC only one of each etiology was limited in driving (6.7% and 6.3%, respectively). Although reflex syncope was the etiology with the highest percentage of patients with limitation of driving it was not found a significant relationship (p=0.260) between this TLoC etiology and the limitation on driving.
Impact on quality of lifeOf the 116 patients who responded to the question about quality of life, almost half of the patients (48.3%) stated that their quality of life was better after hospitalization from the TLoC index episode. Thirty-two patients (27.6%) stated that their quality of life was equal and the remaining 28 patients (24.1%) stated that their quality of life worsened. There was no statistically significant association between any of the etiologies and the impact on quality of life (Table 4).
Regarding the 24 patients with recurrence of TLoC who responded to the question about quality of life, 10 patients (41.7%) reported a worse quality of life, 8 patients (33.3%) reported an improvement and in 6 patients (25%) reported no difference in quality of life. On the other hand, in patients without recurrent episodes of TLoC, in 48 patients (52.2%) the quality of life improved, in 26 patients (28.3%) it remained the same and in 18 patients (19.6%) the quality of life worsened. However, despite these differences in the impact on quality of life between patients with recurrence and no recurrence of TLoC, there was no statistically significant relationship observed.
DiscussionIn this study, it was found that the cardiogenic syncope corresponded to the most common TLoC etiology (39.2%), followed by reflex syncope (27.2%), unexplained TLoC (14.4%), CNS TLoC (12.8%), syncope due to orthostatic hypotension (5.6%) and only one patient with psychogenic pseudosyncope as diagnosis. Compared to other studies, the proportion of patients with syncope of cardiogenic origin was higher,1,6,12,20,21 perhaps because physicians are more aware of the risk of high mortality inherent in cardiogenic syncope and many patients with reflex syncope have been discharged from the ED and studied ambulatory. It is noteworthy that the percentage of patients whose etiology of TLoC was not possible to establish was significantly lower than that reported in previous studies,1,11,12,14,22,23 which shows a good diagnostic accuracy in this hospital.
Although we excluded 31 patients (19.9%) from the study, that follow-up could not done, these patients did not differ much in terms of gender, age, cardiovascular risk factors and TLoC etiology distribution, from the ones included in this study. So, a hypothetical bias is possible, but less probable.
After 18 months of follow- up, 11.2% of patients died, data similar to the study conducted by Sarasin et al.,20 who reported an 18-month total mortality of 9% and other studies published recently.24 It should be noted the high mortality in the short term, verifying that half of the patients died in the first month from the date of admission by the TLoC index episode, and most of these died during the hospitalization from the index episode. Patients with unexplained TLoC had significantly higher mortality compared with other etiologies. One possible explanation may be due to the absence of treatment directed to the cause, and it is therefore important to strengthen efforts in the search for their specific etiology. Despite most patients having died due to unexplained TLoC and cardiogenic syncope as initial diagnosis of the etiology of TLoC, we were not able to establish any statistically significant relationship between cardiogenic syncope and mortality, unlike many studies where it was found that the cardiogenic syncope increases the risk of mortality compared to other etiologies as reflex syncope or unexplained cause,1,6,10,12 probably because in our study patients admitted with reflex syncope were older and had died of other causes.
Twenty percent of patients experienced one or more new episodes of TLoC, a value similar to other studies.11,12,20,25,26 The average number of recurrent episodes of TLoC was 5.6 and the great majority of patients had their first recurrence during the first year after the index admission episode of TLoC as Sarasin et al. had described.20 In our study reflex syncope corresponded to the etiology of TLoC that significantly presented a higher number of patients with recurrences (35.3%). However, follow-up study EGSYS 227 found that different TLoC etiologies do not affect recurrence rates. This could be because in our study patients with cardiogenic syncope or other etiologies receive a more specific treatment, since they are associated with higher mortality1 and therefore treated more incisively. Reflex syncope is classically associated with benign1 nature and the first-line treatment includes the instruction for the implementation of lifestyle changes such as avoidance of triggering factors, recognition of prodromes and physical maneuvers to avoid TLoC, which may not have been explained and effectively applied by the patients and moreover pharmacotherapy presents neutral or negative results when compared to placebo and therefore is not recommended.7
The problem of recurrence is the high morbidity that it entails.6,11–13 These have significant impact on the quality of life of patients,17,18 namely the limitation of vehicle driving. In this study, patients with recurrent episodes of TLoC had a major limitation in driving vehicles, with 20% having stopped driving. In addition, two patients with recurrent episodes of TLoC had road accidents due to these recurrences. It was recently published a study in which patients with recurrent episodes of TLoC and vasovagal syncope were not more likely of having road accidents compared with general population.28 However, in another study it was found that syncope increases the likelihood of automobile accidents compared to general population.29 As traffic accidents and driving limitation can be translated into a significant change in quality of life and have significant social impact, it is pertinent to consider further the implications of TLoC in car driving in prospective studies.
The recurrent episodes, in addition to being associated to car accidents they originated injuries as CET, SH, fractures, falls or hematomas, present in about 60% of patients with recurrence. The health care demand of patients with recurrence also entails the implementation of new diagnostic tests, new admissions that lead to significantly increased costs.20,30 This study confirmed that approximately half of the patients reported that their quality of life improved after discharge from the TLoC index episode. On the other hand, and in relation to patients with recurrence of TLoC, most said their quality of life worsened or remained the same compared to those who had no new episodes of TLoC, data similar to that reported by Barón-Esquivias et al.31
This study has limitations. It is an observational and retrospective study and therefore patients were not submitted to any extra exam on purpose for the study. The sample population is relatively small, limiting the detection of any statistically significant differences between groups. For follow-up data there may have been difficult for patients to remember the events during the year 2013 and beyond. Despite the impact on quality of life seem to be relevant, specific scales or specific questionnaires were not used. The average population age was 70 years, mostly elderly so the study cannot be generalized to other populations and age groups. The concept of TLoC, that incudes syncope and other causes, is recent, and in literature the term TLoC is often used as a synonym of syncope, despite being different entities. As it is a new concept, most of the data and large scale studies are related to syncope. Although the study only included patients who were admitted to the emergency department and who were hospitalized, excluding those that presented in the emergency department with this symptom but were discharged, it would be interesting to evaluate also the diagnosis and prognosis for these patients and compare with the hospitalized ones. This could be investigated in a future study.
This research is a contribution to the study of portuguese reality of TLoC, making it possible to compare the diagnosis and prognosis of TLoC patients with the international literature.
In our study we found that the rates of mortality and recurrence of TLoC are similar to other countries, as well as the consequences that these episodes have. However, differences were found regarding the prevalence of TLoC etiologies, with the highest number of cases of cardiogenic syncope, increased mortality associated with unexplained TLoC and a higher recurrence in reflex syncope. These differences in etiology, recurrence and mortality of TLoC should be clarified by future studies.
The data obtained in our study help reinforce the idea that TLoC episodes should be effectively diagnosed and treated. Thus, the etiology of TLoC should be diagnosed as early as possible, seeking effective therapeutic strategies to prevent new episodes of TLoC and its possible consequences. To achieve this, standardized guidelines must be followed.
Conflict of interestThe authors declare no conflicts of interest.